Abstract
The transient receptor potential melastatin member 8 (TRPM8) is a newly characterized oncoprotein involved in various malignant tumors. However, its expression pattern and biological function in osteosarcoma remain unclear. The present study aimed to explore the expression and prognostic significance of TRPM8 in osteosarcoma (OS). The results revealed that the expression of TRPM8 mRNA and protein in OS tissue was significantly higher than that in paired normal bone tissue (P<0.05). Additionally, the level of TRPM8 mRNA and protein in patients with a higher clinical stage and with distant metastasis was markedly higher than in those with a lower clinical stage and no metastasis (P<0.05). Furthermore, a high TRPM8 level was closely associated with clinical stage and distant metastasis (P=0.007 and 0.030), but not associated with the patient age (P=0.481), gender (P=0.905), tumor size (P=0.429), histological subtype (P=0.207) or anatomical location (P=0.369). In addition, OS patients with high TRPM8 expression had significantly shorter overall survival (P=0.008) and disease-free survival times (P=0.008) when compared with patients with low expression of TRPM8. In Cox multivariate analysis, TRPM8 overexpression was identified to be an independent and significant prognostic factor for overall survival (P=0.040), but not for disease-free survival (P=0.051). Collectively, the present data suggest that TRPM8 may play a crucial role in the development and progression of OS, and thus may be considered as a novel molecular target for therapy in patients with OS.
Keywords: TRPM8, osteosarcoma, prognosis, overall survival, disease-free survival
Introduction
Osteosarcoma (OS) is the most common type of primary malignant cancer originating from the bone in children and young adolescents (1). Considerable advances have been made in surgical technology and combined therapeutic strategies, which has significantly increased the survival rate of patients with OS to 65–75%. However, the survival rate of OS patients with lung metastasis and advanced clinical stage is poor, and this is a major cause of mortality in such patients (2).
Several molecular factors have been explored for their prognostic significance in OS, including cluster of differentiation 44, ezrin and papillomavirus binding factor (3–5). However, no reliable prognostic factors have yet been established for OS. Therefore, the identification of novel strong predictors of tumor progression and survival is of significance in improving therapeutic strategies against OS.
The role of Ca2+ in global cancer-associated cell signaling pathways is well known. Fluctuations in Ca2+ homeostasis may lead to an increase in cell proliferation (6,7) and even induce differentiation (8) and apoptosis (9). A previous study demonstrated that the family of transient receptor potential (TRP) channels are essential mediators of sensory signals with marked effects on cellular functions and signaling pathways, including calcium homeostasis (10). Further evidence indicated that TRP channels are associated with oncogenesis and that these channels might be potential targets for cancer treatment (11). The transient receptor potential melastatin member 8 (TRPM8), a member of the TRP family, is a Ca2+-permeable cation channel also known as the ‘cold receptor’ as it may be activated by cold temperature and menthol (12). Since the identification of the TRPM8 gene in 2001, it has been observed that the abnormal expression of TRPM8 is associated with the phenotype of cancers (13). Furthermore, the prognostic significance of TRPM8 has been described in several cancer types, including prostate (14), breast (15), pancreatic (16) and bladder cancer (17). A previous study indicated that TRPM8 is overexpressed in OS and that knockdown of TRPM8 suppresses cancer malignancy and enhances epirubicin-induced apoptosis in human OS cells (18), However, little is known about the expression and clinical significance of TRPM8 in OS.
The present study assessed the expression profile of TRPM8 messenger RNA (mRNA) in OS by reverse transcription-quantitative polymerase chain reaction (RT-qPCR), and TRPM8 protein expression by western blot analysis and immunohistochemistry. In addition, the association of TRPM8 expression with clinicopathological parameters and prognosis in patients with OS receiving curative surgical resection was investigated.
Materials and methods
Patients and tissue samples
Tumor specimens were collected from two consecutive cohorts of patients with primary OS. Cohort A consisted of 20 patients treated at the First Affiliated Hospital of China Medical University (Shenyang, China) between July and October 2014, from whom fresh tumor samples coupled with adjacent non-tumorous bone tissues 5–10 cm away from the tumor edge were obtained for later analysis of TRPM8 mRNA and protein expression. All the fresh specimens were stored at −80°C until use. Cohort B consisted of 98 OS patients who underwent curative tumor resection at the First Affiliated Hospital of China Medical University between March 2003 and November 2008. None of the patients had received chemotherapy or radiotherapy prior to surgery. The study was approved by the Institutional Review Board of China Medical University. Written informed consent was obtained from all participants. The clinical stage of the OS patients was determined according to the tumor-node-metastasis (TNM) classification of the International Union Against Cancer (UICC) (19). The clinicopathological information of the patients is shown in Table I.
Table I.
Association of TRPM8 expression with clinicopathological features of osteosarcoma.
| TRPM8 | ||||
|---|---|---|---|---|
| Features | Cases, n | Positive, n (%) | Negative, n (%) | P-valuea |
| Age at diagnosis | 0.481 | |||
| <18 years | 47 | 30 (63.8) | 17 (36.2) | |
| ≥18 years | 51 | 29 (56.9) | 22 (43.1) | |
| Gender | 0.905 | |||
| Female | 42 | 25 (59.5) | 17 (40.5) | |
| Male | 56 | 34 (60.7) | 22 (39.3) | |
| Histological subtype | 0.207 | |||
| Osteoblastic | 44 | 22 (50.0) | 22 (50.0) | |
| Chondroblastic | 20 | 15 (75.0) | 5 (25.0) | |
| Fibroblastic | 14 | 9 (64.3) | 5 (35.7) | |
| Mixed | 20 | 14 (70.0) | 6 (30.0) | |
| Clinical stage | 0.007 | |||
| I+IIA | 62 | 31 (50.0) | 31 (50.0) | |
| IIB/III | 36 | 28 (77.8) | 8 (22.2) | |
| Distant metastasis | 0.030 | |||
| Absent | 60 | 31 (51.7) | 29 (48.3) | |
| Present | 38 | 28 (73.7) | 10 (26.3) | |
| Tumor size | 0.429 | |||
| <5 cm | 53 | 30 (56.6) | 23 (43.4) | |
| ≥5 cm | 45 | 29 (64.4) | 16 (35.6) | |
| Anatomic location | 0.369 | |||
| Tibia/femur | 60 | 34 (56.7) | 26 (43.3) | |
| Elsewhere | 38 | 25 (65.8) | 13 (34.2) | |
P-value obtained from Pearson χ2 test or Fisher's exact test. TRPM8, transient receptor potential melastatin member 8.
All 98 OS patients received follow-up for a period ranging from 72 to 132 months. Ten patients were lost to follow-up. The median overall survival and disease-free survival time of patients was 68 and 55 months, respectively.
RT-qPCR
RT-qPCR was performed using the SYBR-Green PCR Master mix (Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA) in a total volume of 20 µl on a 7500 Real-Time PCR system (Applied Biosystems; Thermo Fisher Scientific, Inc.). In brief, total RNA was extracted from tissues using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. The reverse transcription reaction was performed using a high-capacity cDNA synthesis kit (Applied Biosystems; Thermo Fisher Scientific, Inc.). A dissociation step was performed to generate melting curves to confirm the specificity of the amplification. Expression levels of the analyzed genes were normalized to the expression of GAPDH. The fold change in gene expression was calculated by the 2−ΔΔCq method (Cq of TRPM8 - Cq of GAPDH). The sequences of the primer pairs were as follows: TRPM8 forward, 5′-GAGCTGGATGAGCACAAC-3′; TRPM8 reverse, 5′-GAAGTAAGCGAAGACGATG-3′; GAPDH forward, 5′-TGACTTCAACAGCGACACCCA-3′; and GAPDH reverse, 5′-CACCCTGTTGCTGTAGCCAAA-3′. The primers were synthesized by Sangon Biotech (Shanghai, China).
Western blot analysis
Total protein from cells was extracted in lysis buffer (Pierce, Rockford, IL, USA) and quantified using the Bradford method. Samples were separated by sodium dodecyl sulphate-polyacrylamide gel electrophoresis, transferred to polyvinylidene fluoride membranes (Millipore, Billerica, MA, USA), and incubated overnight at 4°C with polyclonal rabbit anti-mouse TRPM8 (dilution, 1:1,000; cat. no. ab3243; Abcam, Cambridge, MA, USA) and monoclonal rabbit anti-human GAPDH (dilution, 1:1,000; cat. no. 2118; Cell Signaling Technology, Inc., Danvers, MA, USA) antibodies. Following incubation with horseradish peroxidase-conjugated goat anti-mouse/rabbit IgG (dilution, 1:10,000; cat. no. 7074; Cell Signaling Technology, Inc.) at 37°C for 2 h, bound proteins were visualized using enhanced chemiluminescence (Pierce) and detected using a Bioimaging System (UVP Inc., Upland, CA, USA). Relative protein levels were quantified using GAPDH as a loading control.
Immunohistochemistry
Tissue sections (4 µm thick) were obtained from formalin-fixed and paraffin-embedded tissue blocks from the OS samples. Sections were washed in xylene to remove the paraffin, rehydrated with serial dilutions of alcohol, and then washed in phosphate-buffered saline solution. Endogenous peroxidase activity was blocked by 3% H2O2 at 37°C for 30 min. Sections were incubated in 10% normal goat serum (Boster Biological Technology, Ltd., Wuhan, China) to block non-specific protein binding sites. Sections were then incubated in primary antibodies against TRPM8 (dilution, 1:200; Abcam) overnight at 4°C. After the primary antibody was washed off, sections were incubated with polyclonal goat anti-rabbit biotin-conjugated secondary antibodies (dilution, 1:1,000; cat. no. E043201; Dako, Glostrup, Denmark) for 30 min at 37°C. Sections were then incubated with streptavidin horseradish peroxidase for 30 min at 37°C. 3,3′-diaminobenzidine substrate (Sigma-Aldrich, St. Louis, MO, USA) was applied to the section, and then sections were counterstained with hematoxylin (Abcam). Sections in which primary antibodies were omitted were used as negative control.
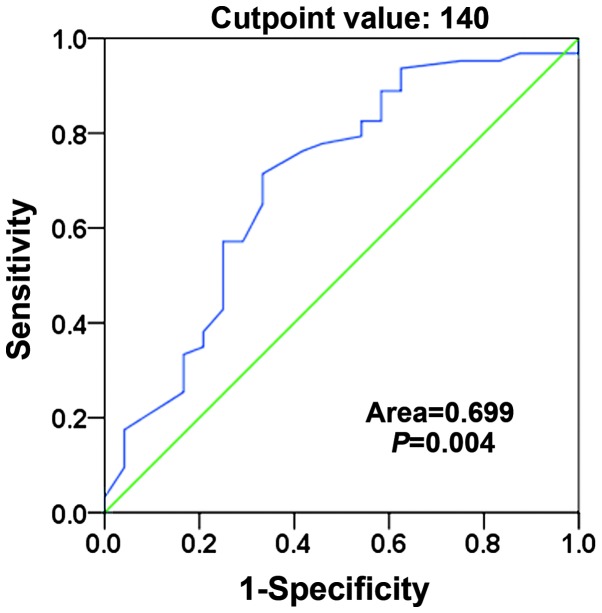
Immunohistochemistry evaluation and selection of cutoff score
The immunostaining was examined under a light microscope (Olympus-IX83; Olympus, Tokyo, Japan) by two pathologists blinded to the experimental conditions. The agreement on the scores between the two pathologists was almost 100%. In cases where the pathologists disagreed on the score, the immunohistochemical scoring was repeated by the two pathologists until the same score was achieved. Each section was assigned an intensity score from 0–3 (0 for no staining, 1 for weak staining, 2 for moderate staining, and 3 for strong staining) and the proportion of tumor cells for that intensity over the total number of tumor cells was recorded in 5% increments from a range of 0–100. A final score (range, 0–300) was achieved by adding the sum of scores obtained for each intensity and the proportion of the area stained. Receiver operating characteristic (ROC) curve analysis was used to determine the cutoff value for TRPM8 expression in the training set using the 0, 1-criterion. In the TRPM8 score, the sensitivity and specificity for survival status in the present study was plotted to generate the ROC curve to determine the cutoff score for positive expression of TRPM8 in osteosarcoma (Fig. 1). The score closest to the points of maximum sensitivity and maximum specificity (140) was selected as the cutoff value. The tumors designated as having negative expression of TRPM8 were those with scores below the cutoff value. Those deemed to have positive expression were those with scores above or equal to the cutoff value.
Figure 1.
Receiver operating characteristic curves were created to determine the cutoff score for positive expression of transient receptor potential melastatin member 8 in osteosarcoma. The sensitivity and specificity for survival status was plotted and the areas under the curve are indicated.
Statistical analysis
Analyses were performed using SPSS 16.0 (SPSS, Inc., Chicago, IL, USA). The t-test was used to analyze data from OS tissues and matched normal bone tissues detected by RT-qPCR and western blot analysis. The association between TRPM8 expression and clinicopathological parameters was evaluated by Pearson's χ2 test or Fisher's exact probability test. Survival probabilities were estimated by the Kaplan-Meier method and assessed by a log-rank test. Univariate and multivariate Cox proportional hazard regression models were used for assessing the association between potential confounding variables and prognosis (overall survival or disease-free survival). P<0.05 was considered to indicate a statistically significant difference.
Results
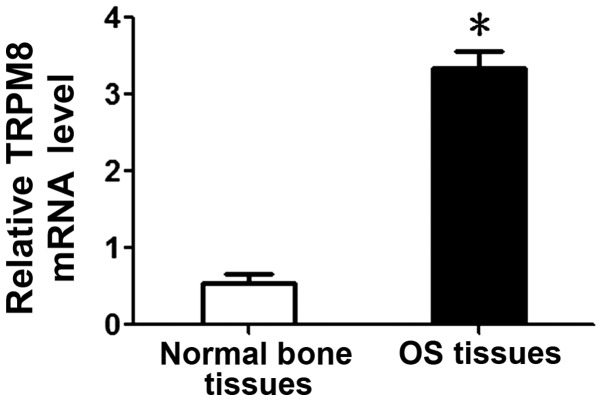
Overexpression of TRPM8 mRNA in OS tissues
TRPM8 mRNA levels were investigated by qPCR in 20 cases of frozen OS and paired normal bone tissues. It was observed that the mean TRPM8 mRNA level in OS tissues was significantly higher than that in normal bone tissues (3.34±0.23 vs. 0.55±0.12; P<0.05; Fig. 2).
Figure 2.
Relative mRNA expression of transient receptor potential melastatin member 8 (TRPM8) in osteosarcoma (OS) tissues compared with normal bone tissues. The gene expression of TRPM8 in OS tissues was much higher (3.34±0.23) than that in normal bone tissues (0.55±0.12; P<0.05). *P<0.05 OS tissues vs. normal bone tissues.
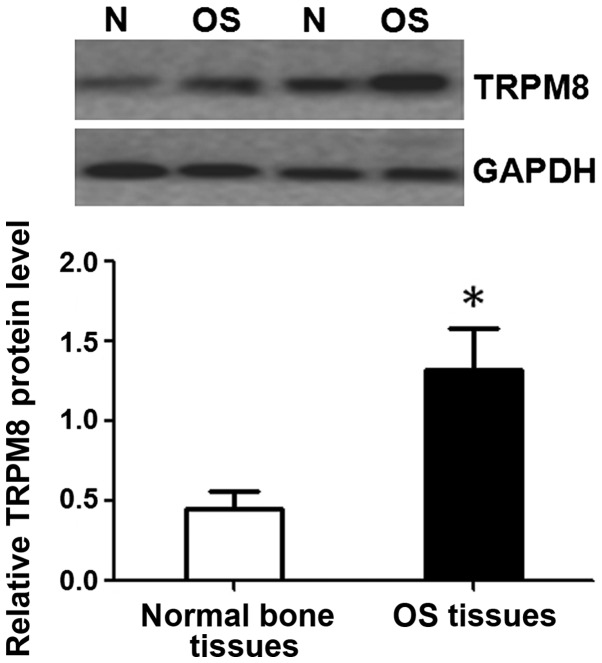
Overexpression of TRPM8 protein in OS tissues
To investigate whether TRPM8 was also elevated at the protein level, western blot analysis was performed on the same specimens that were used in the detection of TRPM8 mRNA. Western blot also demonstrated that the expression of TRPM8 protein was significantly higher in OS tissues compared with that in normal bone tissues (1.32±0.26 vs. 0.45±0.11; P<0.05; Fig. 3).
Figure 3.
Western blot analysis of transient receptor potential melastatin member 8 (TRPM8) protein expression in osteosarcoma tissues (OS) and normal bone tissues (N). The protein expression of TRPM8 in OS tissues was significantly higher than that in normal bone tissues (1.32±0.26 vs. 0.45±0.11; P<0.05). *P<0.05 OS tissues vs. normal bone tissues.
Elevated TRPM8 expression contributes to higher aggressiveness in patients with OS
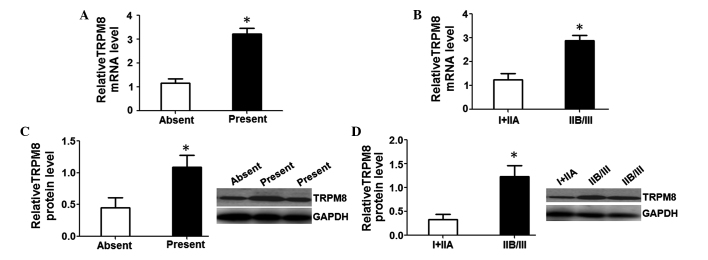
To determine the underlying function of TRPM8 in the occurrence and development of OS, TRPM8 mRNA and protein levels were assessed in patients with distant metastasis or without metastasis as well as in patients with various clinical stages. The results revealed that relative TRPM8 mRNA (3.23±0.23) and protein (1.09±0.19) levels in patients with distant metastasis were markedly higher than in those without metastasis (1.16±0.18 and 0.45±0.16; P<0.05; Fig. 4A and C). Further investigation revealed that relative TRPM8 mRNA (2.89±0.21) and protein (1.23±0.22) levels in the patients with clinical stage IIB/III were also notably higher than in those with clinical stages I+IIA (1.25±0.24 and 0.33±0.11; P<0.05; Fig. 4B and D). These data suggest that an elevated TRPM8 level predicts stronger aggressiveness and a higher clinical stage in OS patients.
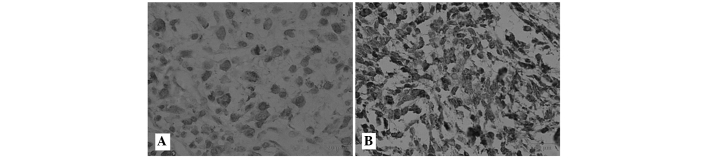
Figure 4.
Immunohistochemical analysis of transient receptor potential melastatin member 8 (TRPM8) expression in osteosarcoma patients. (A) Negative expression level of TRPM8. (B) Positive expression level of TRPM8. Original magnification ×400.
Association between TRPM8 expression and clinicopathological characteristics of OS patients
To further evaluate whether TRPM8 protein upregulation was associated with the clinical characteristics of OS patients, the expression of TRPM8 protein in 98 OS tissue samples was examined by immunohistochemistry. The positive immunoreactivity of TRPM8 was localized in the membrane and cytoplasm of the OS cells. In accordance with the TRPM8 immunoreactive intensity, 60.2% (59/98) patients were classified as having positive TRPM8, and 39.8% (39/98) were classified as having negative TRPM8 (Fig. 5). Table I shows the associations between TRPM8 expression and clinicopathological characteristics in OS patients. TRPM8 protein expression was noted to be strongly associated with distant metastasis and clinical stage (P=0.030 and P=0.007), but not associated with age (P=0.481), gender (P=0.905), tumor size (P=0.429), histological subtype (P=0.207) or anatomical location (P=0.369), suggesting that the TRPM8 protein level may be closely associated with the development and progression of OS.
Figure 5.
High levels of transient receptor potential melastatin member 8 (TRPM8) predict stronger aggressiveness in osteosarcoma. TRPM8 mRNA and protein were investigated in tissues with various clinicopathological features including metastasis and clinical stage by quantitative polymerase chain reaction and western blot analysis. (A,C) TRPM8 mRNA and protein levels in patients with metastasis were significantly higher than those in non-metastatic patients (*P<0.05). (B,D) TRPM8 mRNA and protein levels in patients with a higher clinical stage (IIB/III) were significantly higher than in those with a lower stage (I/IIA; P<0.05).
Prognostic significance of TRPM8 expression in OS
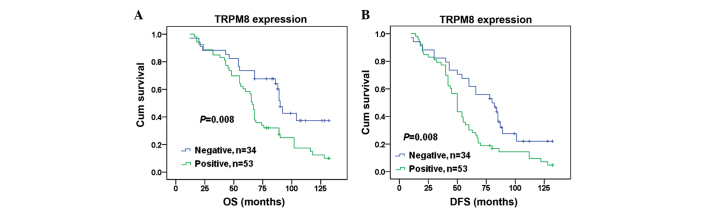
Finally, the prognostic value of TRPM8 expression in OS was assessed. Kaplan-Meier analysis demonstrate a significantly shorter median overall survival and disease-free survival time in patients with positive TRPM8 OS compared with those with negative TRPM8 OS (71 vs. 91 months, P=0.008 and 57 vs. 76 months, P=0.008, respectively; Fig. 6). Univariate analyses demonstrated that tumor size (P=0.036 and P=0.042), clinical stage (P=0.005 and P=0.034), distant metastasis (P=0.001 and P=0.009), anatomic location (P=0.036 and P=0.003) and TRPM8 (P=0.011 and P=0.011) were significant predictors of overall survival and disease-free survival in OS patients (Table II). The multivariate survival analysis (Table II) further confirmed that TRPM8 was an independent prognostic factor (P=0.040), as were distant metastasis (P=0.024) and tumor size (P=0.011) in overall survival, while distant metastasis (P=0.027), tumor size (P=0.030) and anatomic location (P=0.028) were independent prognostic factors in disease-free survival.
Figure 6.
(A) Overall survival (OS) and (B) disease-free survival (DFS) rate in patients with osteosarcoma estimated according to the transient receptor potential melastatin member 8 (TRPM8) expression level (Kaplan-Meier method) with immunohistochemical staining. Patients with positive TRPM8 expression were inclined to have a significantly shorter OS and DFS than those with negative TRPM8 expression.
Table II.
Cox regression analysis of clinicopathological data associated with OS and DFS in osteosarcoma.
| OS | DFS | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate | Multivariate | Univariate | Multivariate | |||||
| Factor | RR | Pa | RR | Pb | RR | Pa | RR | Pb |
| Age, years (≥18/<18) | 1.309 | 0.289 | 1.230 | 0.434 | 1.263 | 0.322 | 1.164 | 0.536 |
| Gender (male/female) | 0.904 | 0.694 | – | – | 1.109 | 0.666 | – | – |
| Tumor size, cm (≥5/<5) | 1.711 | 0.036 | 2.018 | 0.011 | 1.617 | 0.042 | 1.723 | 0.030 |
| Histological subtype (mixed/fibroblastic/chondroblastic/osteoblastic) | 0.978 | 0.827 | – | – | 1.017 | 0.855 | – | – |
| Clinical stage (IIB/III/I+IIA) | 2.065 | 0.005 | 0.369 | 0.251 | 4.294 | 0.034 | 0.308 | 0.166 |
| Distant metastasis (present/absent) | 2.364 | 0.001 | 7.196 | 0.024 | 1.885 | 0.009 | 6.579 | 0.027 |
| Anatomic location (tibia/femur/elsewhere) | 1.709 | 0.036 | 1.408 | 0.288 | 2.017 | 0.003 | 1.752 | 0.028 |
| TRPM8 (positive/negative) | 2.045 | 0.011 | 1.855 | 0.040 | 1.910 | 0.011 | 1.700 | 0.051 |
P-value and RR were assessed using univariate Cox regression analysis
P-value and RR were assessed using multivariate Cox regression analysis. OS, overall survival; DFS, disease-free survival; RR, relative risk.
Discussion
To the best of our knowledge, this is the first study involving a large number of clinical samples that aimed to assess the expression of TRPM8 in OS tissues and its association with OS clinicopathological characteristics and to evaluate the association between TRPM8 expression levels and the prognosis of OS patients. The study firstly confirms that expression levels of TRPM8 mRNA and protein are significantly higher in OS tissues compared with matched normal bone tissues, which is consistent with the findings of a previous study (18). The present study further indicated that TRPM8 may play an essential role in the development and progression of OS.
Accumulating evidence has demonstrated that tumor metastasis and clinical stage are often considered to be the most significant prognostic indicators in various tumors (20–24). To prove whether TRPM8 affects the occurrence of tumor metastasis and the clinical stage, and thereby regulates the development and progression of OS, the present study analyzed TRPM8 mRNA and protein levels in OS tissues with various metastatic states and clinical stages using RT-qPCR and western blot analysis. It was observed that TRPM8 mRNA and protein levels were markedly higher in OS tissues with metastasis and higher clinical stage (IIB/III) than in those without metastasis and with a lower clinical stage (I/IIA), indicating that TRPM8 may be a novel predictor for metastasis and advanced status in patients with OS.
It is well documented that age, tumor size, resectability of the primary tumor, metastatic status and clinical stage are notable clinical characteristics in OS (25). Several studies have demonstrated that TRPM8 overexpression was frequently associated with a number of clinicopathological features, which also confirms the significance of TRPM8 in the development and progression of numerous tumors. In order to explore the possible roles of TRPM8 in OS, the association between TRPM8 protein expression and various clinicopathological features was investigated. In line with the expectations of the present study, it was revealed that TRPM8 protein expression was strongly associated with distant metastasis and clinical stage, further suggesting that TRPM8 may play a major role in the development and progression of OS.
Several studies have demonstrated that TRPM8 overexpression is unfavorable in the prognosis of patients with various tumors (14–17), suggesting a connection between TRPM8 and prognosis of tumor patients, and thus highlighting TRPM8 as a crucial prognosis factor for these tumors. Therefore, to seek new molecular therapeutic targets for patients with OS, the association between TRPM8 and the prognosis of OS patients was further investigated. The present findings revealed that TRPM8 expression was closely associated with disease-free and overall survival in OS patients, with the disease-free and overall survival of patients with positive TRPM8 expression being significantly shorter than in those with negative TRPM8 expression, indicating that TRPM8 may be a novel prognosis predictor and therapeutic target in patients with OS.
Although the precise role of TRPM8 in OS remains unclear, the present study hypothesizes that TRPM8 overexpression may lead to the generation of more Ca2+ release channels in OS cell membrane and cytoplasm, including endoplasmic reticulum and mitochondria, in which TRPM8 is possibly located. This may result in a greater influx of Ca2+ through the TRPM8 channel (26). The increasing concentration of Ca2+ may enhance the participation of mitochondria in numerous metabolic functions including cell growth, death and apoptosis (12), and could account for a significant positive association between the expression of TRPM8 and distant metastasis and clinical stage in OS, with poor survival rates observed in OS patients with high TRPM8 expression.
There are several limitations to the present study, as it was a single-center and retrospective study, using smaller samples. Therefore, to validate the roles of TRPM8 in the pathogenesis and oncogenesis of OS, it will be necessary to carry out in vitro and xenograft functional research in the future, in order to detect the biological alteration of OS cells by the regulation of TRPM8 expression.
In conclusion, elevated TRPM8 expression may play a pivotal role in the occurrence, development and progression of OS. Detection of TRPM8 levels may serve as a clinical predictor in the diagnosis or prediction of clinical outcome in OS patients. Data from the present study may provide novel prospects for molecular target therapy in OS patients, although details are still to be clarified through ongoing investigation.
Acknowledgments
This study was supported by grants from the General Science Research Program of the Education Department of Liaoning Province in China (no. L2014428) and the Natural Science Foundation of Liaoning Province (no. 2013225086).
References
- 1.Gill J, Ahluwalia MK, Geller D, Gorlick R. New targets and approaches in osteosarcoma. Pharmacol Ther. 2013;137:89–99. doi: 10.1016/j.pharmthera.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Ta HT, Dass CR, Choong PF, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer Metastasis Rev. 2009;28:247–263. doi: 10.1007/s10555-009-9186-7. [DOI] [PubMed] [Google Scholar]
- 3.Li H, Min D, Zhao H, Wang Z, Qi W, Zheng S, Tang L, He A, Sun Y, Yao Y, Shen Z. The prognostic role of Ezrin immunoexpression in osteosarcoma: a meta-analysis of published data. PLoS One. 2013;8:e64513. doi: 10.1371/journal.pone.0064513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Y, Wu Y, Gu S, Sun Z, Rui Y, Wang J, Lu Y, Li H, Xu K, Sheng P. Prognostic role of CD44 expression in osteosarcoma: evidence from six studies. Diagn Pathol. 2014;9:140. doi: 10.1186/1746-1596-9-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsukahara T, Kawaguchi S, Torigoe T, Kimura S, Murase M, Ichimiya S, Wada T, Kaya M, Nagoya S, Ishii T, et al. Prognostic impact and immunogenicity of a novel osteosarcoma antigen, papillomavirus binding factor, in patients with osteosarcoma. Cancer Sci. 2008;99:368–375. doi: 10.1111/j.1349-7006.2008.00695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Legrand G, Humez S, Slomianny C, Dewailly E, Vanden Abeele F, Mariot P, Wuytack F, Prevarskaya N. Ca2+ pools and cell growth. Evidence for sarcoendoplasmic Ca2+-ATPases 2B involvement in human prostate cancer cell growth control. J Biol Chem. 2001;276:47608–47614. doi: 10.1074/jbc.M107011200. [DOI] [PubMed] [Google Scholar]
- 7.Thebault S, Flourakis M, Vanoverberghe K, et al. Differential role of transient receptor potential channels in Ca2+ entry and proliferation of prostate cancer epithelial cells. Cancer Res. 2006;66:2038–2047. doi: 10.1158/0008-5472.CAN-05-0376. [DOI] [PubMed] [Google Scholar]
- 8.Vanoverberghe K, Vanden Abeele F, Mariot P, et al. Ca2+ homeostasis and apoptotic resistance of neuroendocrine-differentiated prostate cancer cells. Cell Death Differ. 2004;11:321–330. doi: 10.1038/sj.cdd.4401375. [DOI] [PubMed] [Google Scholar]
- 9.Skryma R, Mariot P, Bourhis XL, et al. Store depletion and store-operated Ca2+ current in human prostate cancer LNCaP cells: involvement in apoptosis. J Physiol. 2000;527:71–83. doi: 10.1111/j.1469-7793.2000.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaneko Y, Szallasi A. Transient receptor potential (TRP) channels: a clinical perspective. Br J Pharmacol. 2014;171:2474–2507. doi: 10.1111/bph.12414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen J, Luan Y, Yu R, Zhang Z, Zhang J, Wang W. Transient receptor potential (TRP) channels, promising potential diagnostic and therapeutic tools for cancer. Biosci Trends. 2014;8:1–10. doi: 10.5582/bst.8.1. [DOI] [PubMed] [Google Scholar]
- 12.Knowlton WM, McKemy DD. TRPM8: From cold to cancer, peppermint to pain. Curr Pharm Biotechnol. 2011;12:68–77. doi: 10.2174/138920111793937961. [DOI] [PubMed] [Google Scholar]
- 13.Tsavaler L, Shapero MH, Morkowski S, Laus R. Trp-p8, a novel prostate-specific gene, is up-regulated in prostate cancer and other malignancies and shares high homology with transient receptor potential calcium channel proteins. Cancer Res. 2001;61:3760–3769. [PubMed] [Google Scholar]
- 14.Kim SH, Nam JH, Park EJ, Kim BJ, Kim SJ, So I, Jeon JH. Menthol regulates TRPM8-independent processes in PC-3 prostate cancer cells. Biochim Biophys Acta. 2009;1792:33–38. doi: 10.1016/j.bbadis.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Chodon D, Guilbert A, Dhennin-Duthille I, Gautier M, Telliez MS, Sevestre H, Ouadid-Ahidouch H. Estrogen regulation of TRPM8 expression in breast cancer cells. BMC Cancer. 2010;10:212. doi: 10.1186/1471-2407-10-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yee NS, Zhou W, Lee M. Transient receptor potential channel TRPM8 is over-expressed and required for cellular proliferation in pancreatic adenocarcinoma. Cancer Lett. 2010;297:49–55. doi: 10.1016/j.canlet.2010.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao N, Jiang LM, Ge B, Zhang TY, Zhao XK, Zhou X. Over-expression of TRPM8 is associated with poor prognosis in urothelial carcinoma of bladder. Tumour Biol. 2014;35:11499–11504. doi: 10.1007/s13277-014-2480-1. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Yang Z, Meng Z, Cao H, Zhu G, Liu T, Wang X. Knockdown of TRPM8 suppresses cancer malignancy and enhances epirubicin-induced apoptosis in human osteosarcoma cells. Int J Biol Sci. 2013;10:90–102. doi: 10.7150/ijbs.7738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spiessl B, Scheibe O, Wagner G, editors. Illustrated Guide to the Classification of Malignant Tumours. Springer-Verlag; Berlin: Soft tissue sarcomas. In: International Union Against Cancer (UICC) TNM-Atlas; pp. 170–172. [Google Scholar]
- 20.Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9:606–616. doi: 10.1634/theoncologist.9-6-606. [DOI] [PubMed] [Google Scholar]
- 21.Greene FL, Stewart AK, Norton HJ. A new TNM staging strategy for node-positive (stage III) colon cancer: an analysis of 50,042 patients. Ann Surg. 2002;236:416–421. doi: 10.1097/00000658-200210000-00003. (Discussion 421) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jatoi I, Hilsenbeck SG, Clark GM, Osborne CK. Significance of axillary lymph node metastasis in primary breast cancer. J Clin Oncol. 1999;17:2334–2340. doi: 10.1200/JCO.1999.17.8.2334. [DOI] [PubMed] [Google Scholar]
- 23.Madu CO, Lu Y. Novel diagnostic biomarkers for prostate cancer. J Cancer. 2010;1:150–177. doi: 10.7150/jca.1.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol. 2003;10:65–71. doi: 10.1245/ASO.2003.03.058. [DOI] [PubMed] [Google Scholar]
- 25.Rech A, Castro CG, Jr, Mattei J, Gregianin L, Di Leone L, David A, Rivero LF, Tarrago R, Abreu A, Brunetto AL. Clinical features in osteosarcoma and prognostic implications. J Pediatr (Rio J) 2004;80:65–70. doi: 10.2223/1136. (In Portuguese) [DOI] [PubMed] [Google Scholar]
- 26.Li Q, Wang X, Yang Z, Wang B, Li S. Menthol induces cell death via the TRPM8 channel in the human bladder cancer cell line T24. Oncology. 2009;77:335–341. doi: 10.1159/000264627. [DOI] [PubMed] [Google Scholar]