Abstract
Inflammation is a part of the complex biological response of inflammatory cells to harmful stimuli, such as pathogens, irritants, or damaged cells. This inflammation has been linked to several chronic diseases including cancer, atherosclerosis, rheumatoid arthritis, and multiple sclerosis. Major biomarkers of inflammation include tumor necrosis factor, interleukins (IL)-1, IL-6, IL-8, chemokines, cyclooxygenase, 5-lipooxygenase, and C-reactive protein, all of which are regulated by the transcription factor nuclear factor-kappaB. Although examining inflammatory biomarkers in blood is a standard practice, its identification in saliva and/or urine is more convenient and non-invasive. In this review, we aim to (1) discuss the detection of these inflammatory biomarkers in urine and saliva; (2) advantages of using salivary and urinary inflammatory biomarkers over blood, while also weighing on the challenges and/or limitations of their use; (3) examine their role(s) in connection with diagnosis, prevention, treatment, and drug development for several chronic diseases with inflammatory consequences, including cancer; and (4) explore the use of innovative salivary and urine based biosensor strategies that may permit the testing of biomarkers quickly, reliably, and cost-effectively, in a decentralized setting.
Keywords: Inflammation, chronic diseases, biomarkers, urine, saliva, cancer
Introduction
Inflammation is a part of the complex biological response of vascular tissues to harmful stimuli, such as pathogens, irritants, or damaged cells. The word inflammation was derived from the Latin word inflammare, which meant, ‘to set on fire.’ The classic signs of inflammation as first described by a Roman encyclopedist, Cornelius Celsus (25 BC–50 AD), were calor (heat), dolor (pain), rubor (redness), and tumor (swelling). Much later, in the 1800s, German pathologist Rudolf Virchow, added functio laesa (loss of function) to the definition of inflammation.1
Inflammation occurs as a stereotyped response, and therefore is considered a mechanism of innate immunity, as compared to adaptive immunity, which is specific for each pathogen. Therefore, inflammation is not a synonym for infection, even in cases when inflammation is caused by an infection. In current medicine, inflammation is classified to be acute (an initial, immediate, and short-term response of the body to harmful stimuli) or chronic (a long-term response leading to a progressive shift in the types of cells present at the site of inflammation, characterized by simultaneous destruction and healing of the tissue from the inflammatory process).2 Some of the known potential sources of inflammation may include environmental/industrial pollutants (e.g. cigarette smoke, carbon dioxide emissions, smog, sulfur dioxide/nitrogen dioxide emissions); ultraviolet radiation; dietary factors (e.g. consumption of a Westernized dietary pattern comprising of refined carbohydrates and/or fried foods or red/processed meats and cooking methods such as grilling/charbroiling); other lifestyle factors (e.g. smoking, alcohol consumption); obesity; bacteria (e.g. Helicobacter pylori, Salmonella typhi, Streptococcus bovis, Escherichia coli, Chlamydia, pneumonia); viruses (e.g. herpes simplex virus B, hepatitis viruses, human papilloma virus, human immunodeficiency virus [HIV], Epstein-Barr virus); as well as stress factors (e.g. pH, hypoxia, chemotherapy, heavy metals).3
Link between inflammation and chronic diseases
Most chronic diseases are caused by chronic inflammation. However, acute inflammation exerts therapeutic potential. The association between inflammation and chronic diseases is supported by epidemiological, pharmacological, and genetic studies.4 In 1850, Rudolf Virchow, a German scientist from Wurzburg, was the first to link inflammation with various chronic diseases, which include cancer, atherosclerosis, arthritis, diabetes, asthma, multiple sclerosis, and Alzheimer’s disease.5 To date, over 200 different types of diseases caused by inflammation have been described. Usually inflammatory diseases are represented by suffix ‘itis.’ For example, arthritis, bronchitis, sinusitis, gastritis, esophagitis, pancreatitis, meningitis, rhinitis, and gingivitis are, respectively, inflammation of the joints, bronchi, sinuses, stomach, esophagus, pancreas, brain, nose, and gums. Today, inflammation is considered a risk factor for most cancers (e.g. 11–24% of patients with bronchitis progress to develop lung cancer; 15% of patients with esophagitis progress to develop esophageal cancer; 10–15% of patients with asbestosis progress to develop mesothelioma; ≤10% of patients with pancreatitis progress to develop pancreatic cancer; and 1% of patients with inflammatory bowel disease progress to develop colorectal cancer).6
How chronic inflammation resulted in the development of chronic diseases is well documented by numerous studies. Various reports revealed that free radicals are generated during chronic inflammation, which activates the process of damage and deterioration in target cells and organs and leads to further chronic disease. Mechanistically, these free radicals are known to induce the activation of signaling molecules and transcription factors associated with several chronic diseases.4,7,8 The master inflammatory transcription factors are nuclear factor-kappaB (NF-κB) and STAT3. Activation of these transcription factors have been implicated in a wide variety of diseases, including cancers, diabetes mellitus, cardiovascular diseases, autoimmune diseases, viral replication, septic shock, neurodegenerative disorders, ataxia telangiectasia, arthritis, asthma, inflammatory bowel disease, and several other inflammatory conditions.9
Besides these transcription factors, several other biomarkers of inflammation are implicated in chronic diseases. Common factors include inflammatory cytokines and chemokines (tumor necrosis factor [TNF]-α, interleukin-1 [IL-1], IL-6, IL-8, and monocyte chemotactic protein 1), proinflammatory enzymes (e.g. cyclooxygenase [COX]-2, 5-lipoxygenase [LOX], 12-LOX, and matrix metalloproteinases [MMPs]), prostate-specific antigen [PSA], C-reactive protein, adhesion molecules, vascular endothelial growth factor [VEGF], and TWIST.10 Thus, it is clear that most chronic diseases are preceded by a chronic low level of inflammation.
Biomarkers for detection of diseases
Diagnosis, stratification, prognosis, and therapy for inflammation include the measurement of biological markers (i.e. biomarkers) in biological specimens. In 1998, the National Institutes of Health Biomarkers Definitions Working Group defined a biomarker as a characteristic that is objectively measured and evaluated as an indicator of normal biological, pathogenic, or pharmacological responses to a therapeutic intervention. Numerous biomarkers of inflammation have been discovered in the last two decades (e.g. cytokines [TNF, IL-1, -6, etc], chemokines, COX-2, 5-LOX, MMPs, VEGF, TWIST, cell surface adhesion molecules).11 Since NF-κB is an up-regulator of all these biomarkers, its activation is considered a major mediator of inflammation in most chronic diseases, including cancer. Biomarkers may be measured in several biological specimens (e.g. blood, urine, sputum/saliva, hair, feces, cerebrospinal fluid, body tissues). It is evident that examining inflammatory biomarkers in blood is a standard practice when it comes to clinical diagnosis; however, recent trends suggest that measuring diagnostic biomarkers in novel biological specimens (e.g. saliva and urine) is becoming increasingly popular due to its non-invasive nature.12
The diagnostic use of salivary and urinary biomarkers poses several advantages over the traditional measurements of inflammatory biomarkers in blood. For example, (i) they not only spare the patients of the stress from venipuncture, but also eliminate the need of specialized technicians for specimen collection, thereby reducing the healthcare costs; (ii) they do not clot, and therefore eliminate the need of anticoagulation treatment after collection; (iii) they are less likely to transmit diseases than blood through contact or needle-stick injury and therefore are safer; (iv) they are ‘quiescent,’ meaning that their molecular activity doesn’t change much after sampling; (v) they are a relatively clean medium and contain few interfering proteins; and (vi) the simplicity of specimen collection opens an avenue for self-collection of specimens at home by the patients.
In this review, we aim to (1) further discuss the advantages of using novel biological specimens (i.e. saliva and urine) for detecting inflammatory biomarkers over those in blood, while also weighing on the challenges and limitations of their use; (2) examine their role(s) in connection with diagnosis, prevention, treatment, and drug development for several chronic diseases with inflammatory consequences, including cancer; and (3) explore the use of innovative salivary and urine based biosensor strategies that may permit the testing of biomarkers quickly, reliably, and cost-effectively, in a decentralized setting.
Importance of saliva and urine for detection of biomarkers
Saliva and urine are important physiologic fluids containing a highly complex mixture of substances including proteins and genetic molecules. Saliva provides non-invasiveness and stress-free sample collection, easy and multiple sampling opportunities, reduced need for sample pre-processing, and minimal risk of contracting infectious organisms, and it is also an ideal biofluid for collecting specimens from patients in developing countries.13 Urine is also one of the most interesting and useful biofluids for routine testing and provides an excellent resource for the discovery of novel biomarkers, with the advantage over tissue biopsy samples due to the ease and less invasive nature of collection.14 Because of these, saliva and urine could be used in clinical practice for monitoring and diagnosis.
Saliva is used diagnostically for numerous diseases including neurological diseases, Cushing’s syndrome,15 HIV,16 and cancer.17,18 The possibility to identify and measure biomarkers in saliva also opens the avenue for screening at-risk populations and monitoring disease progression and compliance with treatment modalities. As an example, cetuximab (Erbitux) is an epidermal growth factor receptor (EGFR) inhibitor currently used for the treatment of metastatic head and neck squamous cell carcinoma (HNSCC). Saliva contains soluble EGFRs, and by analyzing the levels in saliva over time it is possible to determine the patient’s response to cetuximab treatment.19 In urine, approximately 40% of the pyridinoline, biomarker of osteoclastogenesis, crosslinks are eliminated as free components, and the rest as peptide-bound forms.20,21 A number of biomarkers in urine including PSA for urologic cancers such as prostate cancer are determined.22 Considering these facts, saliva and urine could be used as an important source of biomarkers for disease diagnosis.
Saliva in diagnosis, prevention, and treatment of diseases
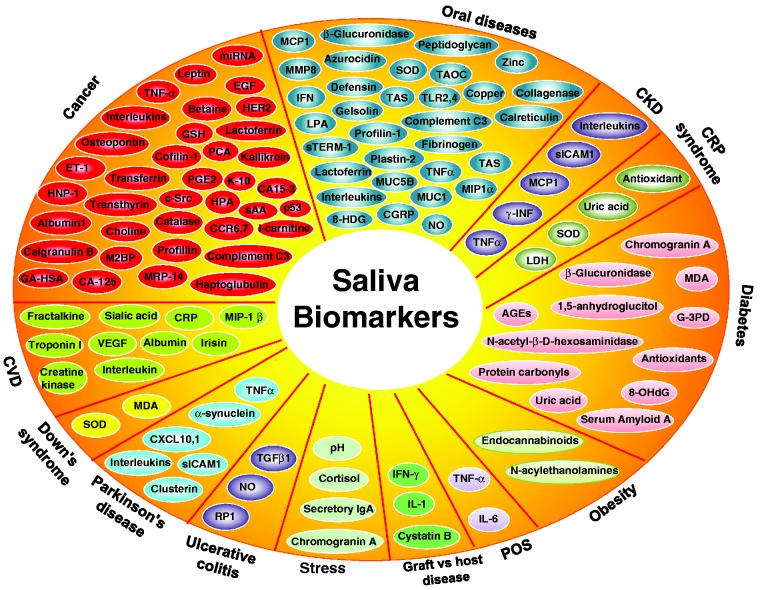
There are several methods, criteria and procedures are used for disease diagnosis. Saliva and urine screening are being used for the diagnosis, prevention, and treatment of numerous diseases. A large number of medically valuable analytes in saliva are gradually unveiled, and some of them represent biomarkers (Figure 1) for diseases including cancer, autoimmune diseases, chronic kidney diseases, diabetes, oral diseases, and cardiovascular diseases23,24 (see Table 1).
Figure 1.
Salivary biomarkers linked with diagnosis, prevention, and treatment of various diseases. (A color version of this figure is available in the online journal.)
Table 1.
Detection of inflammatory biomarkers in saliva of patients with various chronic diseases
| Biomarkers | References |
|---|---|
| Cancer | |
| Oral Squamous Cell Carcinoma | |
| TNF-α, IL-1α, IL-6, IL-8 | (25) |
| IL-1β, Osteopontin | (26) |
| ET-1 | (27) |
| HNP-1 | (28) |
| Albumin | (29) |
| CA-125 | (30) |
| Glutathione | (31) |
| Ig heavy constant, Cofilin-1, Region gamma | (32) |
| Transferrin, Transthyretin, Calgranulin B | (32) |
| M2BP, MRP-14, Profillin, Catalase | (33) |
| p53 antibodies | (34) |
| Haptoglobin, Complement C3 | (35) |
| PGE2 | (36) |
| CCR6, CCR7, c-Src | (37) |
| Sialyl lewis-x | (38) |
| Total antioxidant | (39) |
| IL-10 | (40) |
| HPA, sAA, K-10, GA-HSA | (41) |
| Choline, Betaine, Pipecolinic acid, l-carnitine | (42) |
| Head and neck squamous cell carcinoma | |
| miR-9, miR-134, miR-191 | (43) |
| Breast Cancer | |
| EGF | (44) |
| EGF Receptor, HER2 | (18) |
| CA15-3, EGFR | (45) |
| Solid Tumors | |
| Kallikrein | (46) |
| Parotid Tumors | |
| Leptin | (47) |
| Lung Cancer | |
| Lactoferrin | (48) |
| Ovarian Cancer | |
| CA 125, Glycoprotein complex | (45) |
| Oral Diseases | |
| Periodontal Disease | |
| MIP-1α | (49, 50) |
| MCP-1 | (51) |
| MMP-8 | (52) |
| NO | (53) |
| Lysophosphatidic acid | (54) |
| sTREM-1 | (55) |
| β-Glucuronidase | (56) |
| IL-1β, -6, -8, MMP-8, IFN-α | (57) |
| Lactoferrin | (58) |
| 8-Hydroxydeoxyguanosine | (59) |
| Azurocidin | (60) |
| Collagenase, Profilin-1, Calreticulin, Peptidoglycan | (61) |
| Lactotransferrin, Fibrinogen Alpha Chain, Plastin-2 | (61) |
| Alpha-2- Macroglobulin, Alpha-2-HS-Glycoprotein | (61) |
| Complement C-3, MMP-9, Gelsolin, Defensin | (61) |
| SOD, TAS, IL-1β | (62) |
| TOS, TAOC | (63) |
| Oral Lichen Planus | |
| IL-6, -8, -18, TNF-α | (64) |
| IL-1α, -6, -8 | (25) |
| IFN-γ, IL-4 | (65) |
| TLR-2, TLR-4 | (66) |
| IFN-γ, IL-4 | (67) |
| Dental Caries | |
| TNF-α, IL-6, -8 | (68) |
| sTLR-2 | (69) |
| SOD, Copper, Zinc levels | (70) |
| MUC1, MUC5B | (71) |
| Burning Mouth Syndrome | |
| CGRP | (72) |
| Autoimmune Diseases | |
| Sjorgen’s Syndrome | |
| CXCL10 | (73) |
| CXCL13 | (74) |
| sICAM-1 | (75) |
| IL-17, -22, -23 | (76) |
| IL-4, IL-5, Clusterin | (77) |
| Crohn’s Disease | |
| IL-1β, -6, TNF-α | (78) |
| Atherosclerosis | |
| TNF-α, IL-6, -10 | (79) |
| Parkinson's Disease | |
| α-synuclein | (80) |
| Chronic Kidney Disease | |
| IL-1β, -6, -8, TNF-α, γ-INF, MCP-1, sICAM-1 | (81) |
| Complex Regional Pain Syndrome | |
| SOD, Uric acid, Antioxidant, Albumin, LDH | (82) |
| Ulcerative Colitis | |
| TGF-β1, NO, RP-1 | (83) |
| Diabetes | |
| β-Glucuronidase | (56) |
| G-3PD, Serum amyloid A | (84) |
| 1,5-anhydroglucitol | (85) |
| N-acetyl-β-D-hexosaminidase | (86) |
| 8-OHdG, Protein carbonyls | (87) |
| MDA, Uric acid | (88) |
| Chromogranin A | (89) |
| Antioxidant enzymes | (90) |
| Advanced glycation endproducts | (91) |
| Obesity | |
| Endocannabinoids, N-acylethanolamines | (92) |
| Polycystic Ovary Syndrome | |
| TNF-α, IL-6 | (93) |
| Graft vs. Host Disease | |
| IFN-γ | (94) |
| IL-1, Cystatin B | (95) |
| Sub-acute Thyroiditis | |
| CRP | (96) |
| Down's Syndrome | |
| SOD, Malondialdehyde | (97) |
| Stress | |
| pH | (98) |
| Chromogranin A | (99) |
| Cortisol | (100) |
| Secretory IgA | (101) |
| Cardiovascular Diseases | |
| Myocardial Infarction | |
| Irisin | (102) |
| Fractalkine, IL-17, IL-6, IL-9, | (103) |
| MIP-1 β, CRP, VEGF, IL-5 | (103) |
| Oxidative stress | (104) |
| Ischemia-modified albumin | (105) |
| Creatine kinase MB, Creatine phosphokinase | (106) |
| Free sialic acid | (107) |
| Heart Failure | |
| CRP, Troponin I | (108) |
EGF, Epidermal Growth Factor; CRP, C Reactive Protein; TNF, Tumor Necrosis Factor α: Alpha; IL, Interleukin; ET, Endothelin; HNP, Human alpha-Defensin; CA, Cancer Antigen; Ig: Immunoglobulin; M2BP, Mac-2 Binding Protein; MRP, Myeloid-Related Protein; PGE2, Prostaglandin E2; CCR, Chemokine Receptor; IFN, Interferon; TLR, Toll-Like Receptor; TGF, Transforming Growth Factor; NO, Nitric Oxide; MIP, Macrophage Inflammatory Protein; MCP, Monocyte Chemoattractant Protein; MMP, Matrix Metalloproteinases; s-TREM, soluble-Triggering Receptor Expressed on Myeloid Cells; CXCL: Chemokine Ligand; sICAM, soluble Intercellular Adhesion Molecule; SOD, Superoxide Dismutase; LDH, Lactate Dehydrogenase; RP-1, Recognition Protein-1; G-3PD, Glyceraldehyde-3 P Dehydrogenase; CGRP, Calcitonin gene-related peptide.
Cancer
Evidence from various studies revealed that a number of salivary proteins are altered in oral cancer patients, including Cyfra 21-1, TPS and CA12, various oxidative stress-related salivary parameters, and biochemical and immunological parameters. In a study, concentrations of four potential salivary biomarkers—choline, betaine, pipecolinic acid, and l-carnitine—were present in significantly different concentrations between oral squamous cell carcinoma (OSCC) patients at stages I and II and healthy individuals.42 DNA promoter hypermethylation in saliva of oral cancer patient was also found to be useful for the early diagnosis of oral cancer and potentially can be applied in a clinical setting.109 Salivary biomarker MMP-1 with 100% specificity was also detected in saliva rinse that could be potentially useful for non-invasive diagnosis of HNSCC of the oral cavity or oropharynx.110 Collectively these data are predictive in using saliva for diagnosing some types of cancer.
Autoimmune diseases
In autoimmune diseases such as Sjögren’s syndrome, saliva ferning patterns were used as a diagnostic test for dry mouth in the primary or secondary stage of diseases. Patients with Sjögren’s syndrome showed abnormal salivary smears, usually with a combination of reindeer antler ferning, thick branching ferning, and mucosal squamous.111 Hu et al.112 identified 24 antibodies that can differentiate healthy patients from patients with primary Sjögren’s syndrome and patients with systemic lupus erythematosus. They also evaluated four other antibodies—anti-transglutaminase, anti-histone, anti-Sjögren’s-syndrome-related antigen A (anti-SSA), and anti-Sjögren’s syndrome B—in the saliva of patients, which exhibit as biomarkers. Recently, BP180 and BP230 biomarkers have shown diagnostic tool for the detection of Bullous pemphigoid subepidermal blistering disease.113 Besides these, there is an also increasing interest in using microRNAs (miRNA) as biomarkers in autoimmune diseases.
Infectious diseases
Infectious diseases can be also diagnosed by salivary biomarkers. In fact, saliva is considered the best diagnostic tools for periodontitis. The presence and number of bacterial taxa and other protein markers differentiate the diseases.114 In the diseases caused by flavivirus, nonstructural protein 1 has been clinically accepted as an alternative biomarker and detection of this protein in the saliva, allowing early diagnosis of the disease.115 Detection of Leishmania siamensis DNA in the saliva of an asymptomatic patient by polymerase chain reaction also could be used as a marker to diagnose the disease.116 Besides these, in a cohort study among secondary school students in Tanzania, the presence of HIV antibodies in saliva has been investigated. One percent and 5.5% students at the rural and urban schools, respectively, tested positive for HIV antibodies in saliva.117 Thus, providing HIV knowledge based on this salivary antibody test, the incidence and progression of AIDS can be prevented.
In addition, saliva exhibits antimicrobial and antifungal properties, which manifest its efficacy in the treatment of infectious disease. Saliva was found to be useful in the treatment of the sexually transmitted disease gonorrhea, since it is a powerful and specific inhibitor of Neisseria gonorrhoeae. The alpha-amylase present in saliva was found to be responsible for inhibition of this bacterial growth.118
Oral disease
Within the past few years, the use of saliva as a diagnostic tool has gained considerable attention. Salivary biomarkers are used as early predictors for clinical disease, contribute to the effective prevention and treatment of diseases, and enhance the assessment of potential health risks. In case of dental caries, saliva also plays an important role in the prevention and development of enamel caries. The components present in saliva protect the enamel surface taken by dental biofilm.119 In another study with caries-susceptible and caries-resistant female subjects (20 to 21 years old), it was found that the lipid concentrations in parotid saliva in caries-susceptible subjects were higher than those from caries-resistant ones, and differences in fatty acid composition also were found. Thus, the variations in the lipid levels and fatty acid composition may be associated with those in caries development.120 In addition, saliva contains several types of antimicrobial peptides that play a role in innate immunity. Salivary peptides such as alpha/beta-defensins and human neutrophil defensins or human neutrophil peptide 1 (HNP)-1, -2, and -3 exhibit antimicrobial activity. Thus, these peptides could be useful for the treatment of periodontal disease and for the prevention of caries and periodontitis.121 Another component of saliva, fluoride, can also prevent dental caries by acting very early on remineralization and demineralization processes in enamel surfaces.122
Saliva has been linked with the treatment condition of diseases. In human subjects, salivary chitotriosidase activity was found to be decreased after non-surgical periodontal treatment in patients having periodontitis with or without coronary atherosclerosis. Thus, salivary chitotriosidase can be used as a marker for the evaluation of periodontal treatment and host response.123 Other studies have shown an increase in the levels of salivary antioxidants after non-surgical periodontal treatment. In chronic periodontitis patients, an increase of uric acid, albumin, glutathione peroxidase, and total antioxidative status was detected with a decrease of superoxide dismutase activity after treatment.124 Guentsch et al.125 also showed that non-surgical periodontal treatment leads to a reduction of salivary malondialdehyde, glutathione peroxidase to levels comparable to healthy controls. Salivary proteins including tissue inhibitor of metalloproteinases 1 (TIMP1) also modulated by the treatment of doxycycline in patients of chronic periodontitis. Doxycycline resulted in significant improvement in clinical parameters compared with the conventional periodontal treatment. Although doxycycline did not produce significant reductions in MMP-8 and MMP-9 levels, increases in the TIMP-1 concentration and the MMP-8/TIMP-1 and MMP-9/TIMP-1 ratios in saliva were observed.126 Besides these, the salivary defense factors lactoferrin, chitinase, and eta-N-acetylhexosaminidase are also found to be suitable for monitoring periodontal treatment results. It has been shown that concentrations of these factors decrease after periodontal treatment.127
Other
The role of saliva in the diagnosis, prevention, and treatment of other diseases including peptic ulcer has also been emphasized. Salivary mucus swallowed with food reduces the alkalinity of bile and therefore prevents damage of mucous cells.128 Saliva is also helpful in the diagnosis and prevention of occupational diseases. For example, exposure to the environmental contaminant phthalate results in several diseases. Detection of phthalate metabolites in human saliva indicate incidence of phalate-associated diseases.129 Therefore, by taking necessary preventive measures, disease occurrence can be prevented. Furthermore, in cardiovascular disease, determinations of total serum amylase and salivary amylase activity can be also used as a biomarker.130 Conclusively, such assessments are in the initial stages of development and require considerable further research to determine their clinical utility.
Urine in diagnosis, prevention, and treatment of diseases
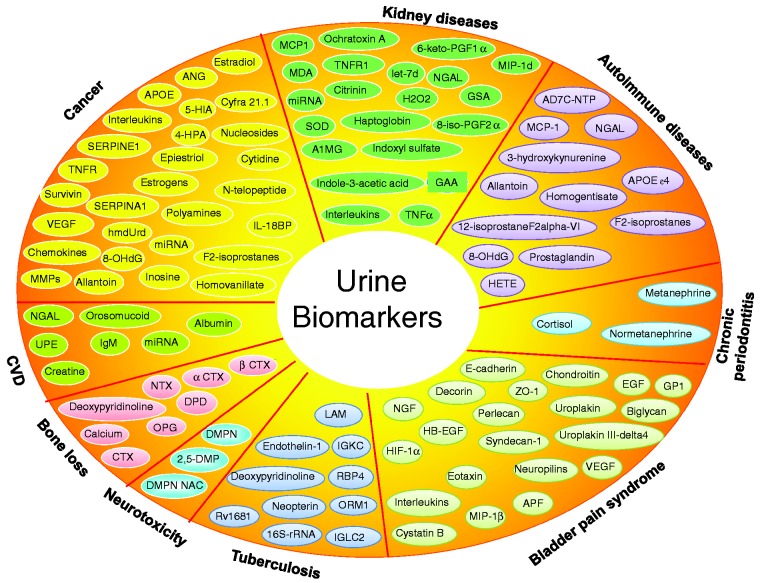
Numerous experimental and clinical studies revealed that urine could be used as tool for the diagnosis, prevention, and treatment of various diseases, e.g. cancer, kidney diseases, infectious diseases, autoimmune diseases, tuberculosis, and cardiovascular diseases (Table 2). Urine contains several molecules that act as biomarkers for the diagnosis, prevention, and treatment of diseases (Figure 2).
Table 2.
Detection of inflammatory biomarkers in urine of patients with various chronic conditions
| Biomarker | Reference |
|---|---|
| Cancer | |
| Bladder Cancer | |
| IL-6, IL-8 | (131) |
| Chemokine 18 | (132) |
| VEGF, IL-8, MMP-9, MMP-7, Survivin, Cyfra 21.1 | (133) |
| MMP-9, MMP-10, SERPINE1, | (134) |
| IL8, APOE, SERPINA1, ANG | (134) |
| Breast Cancer | |
| IL-8, TNF receptor p55 | (135) |
| Allantoin, F2-isoprostanes | (136) |
| Estrogens, metabolites | (137) |
| Estradiol, 16-epiestriol, | (138) |
| 17-epiestriol, 16-ketoestradiol | (138) |
| 5-hydroxymethyl-2-deoxyuridine, | (139) |
| 8-hydroxy-2-deoxyguanosine, | (139) |
| Homovanillate 4-hydroxyphenylacetate | (140) |
| 5-hydroxyindoleacetate, Urea | (140) |
| Nucleosides | (141) |
| Cytidine, methylcytidine, Inosine | (142) |
| Polyamines | (143) |
| IL-1α, -8, VEGF, MMP-9 | (144) |
| Non-Hodgkin’s Lymphoma | |
| IL-8 | (145) |
| Prostate Cancer | |
| IL-18BP | (146) |
| miRNA-483-5p, miRNA-1275, miRNA-1290 | (147) |
| N-telopeptide | (148) |
| miR-16, miR-21, miR-222 | (149) |
| Lung Carcinoma | |
| NNAL | (150) |
| Kidney Disease | |
| MCP-1, TNF-α | (151) |
| MIP-1d, IL-1β | (152) |
| TNFR1 | (153) |
| IL-8 | (154) |
| let-7d, miR-203, miR-320 | (155) |
| Ochratoxin A, Citrinin | (156) |
| NGAL | (157) |
| TNF-α, IL-8, IL-10, SOD, MDA, | (158) |
| 6-keto-PGF1α, 8-iso-PGF2α, H2O2 | (158) |
| Guanidinosuccinic acid | (159) |
| Guanidinoacetic acid, Indoxyl sulfate, | (159) |
| Indole-3-acetic acid | (159) |
| A1MG, Haptoglobin | (160) |
| Autosomal Dominant Polycystic kidney | |
| IL-18 | (161) |
| NGAL | (162) |
| Focal Segmental Glomerulosclerosis | |
| MCP-1 | (163) |
| HIV-associated Nephropathy | |
| NGAL | (164) |
| Neurotoxicity | |
| 2,5-DMP, DMPN, DMPN NAC, | (165) |
| Autoimmune Diseases | |
| Alzheimer's Disease | |
| AD7C-NTP | (166) |
| APOE ε4 | (167) |
| 3-hydroxykynurenine, Homogentisate, Allantoin | (168) |
| 8-Hydroxy-2'-deoxyguanosine | (169) |
| Amyloid beta protein | (170) |
| F2-isoprostanes, Prostaglandin | (171) |
| Parkinson Disease | |
| 12-isoprostaneF2alpha-VI | (172) |
| Dopamine | (173) |
| 8-hydroxy-2'deoxyguanosine | (174) |
| Hydroxyeicosatetraenoic acid | (175) |
| Systemic Lupus Erythematosus | |
| MCP-1 | (176) |
| NGAL | (177) |
| Osteoclastogenesis | |
| DPD, CTX, NTX | (178) |
| αCTX, βCTX | (179) |
| OPG | (180) |
| Calcium | (181) |
| Deoxypyridinoline | (182) |
| Oral Diseases | |
| Chronic Periodontitis | |
| Creatinine-adjusted cortisol, | (183) |
| Metanephrine, Normetanephrine, | (183) |
| Bladder Pain Syndrome | |
| E-cadherin, ZO-1, uroplakin Chondroitin | (184) |
| Epithelial cell growth factors | (185) |
| GP51 | (186) |
| Uroplakin III-delta4 | (187) |
| biglycan, decorin, perlecan, Syndecan-1 | (188) |
| Neuropilins, VEGF | (189) |
| IL-6, IL-8 | (190) |
| NGF | (191) |
| HB-EGF, APF | (192) |
| Tuberculosis | |
| IGKC, RBP4, ORM1, IGLC2, | (193) |
| Lipoarabinomannan | (194) |
| 16S-rRNA | (195) |
| Rv1681 | (196) |
| Deoxypyridinoline | (197) |
| IP-10 | (198) |
| Neopterin | (199) |
| Endothelin-1 | (200) |
| Cardiovascular Disease | |
| NGAL | (201) |
| Urine phosphorus | (202) |
| Creatinine, Albumin | (203) |
| IgM | (204) |
| Orosomucoid | (205) |
| miRNAs | (206) |
| Urine phosphorus | (202) |
| Creatinine, Albumin | (203) |
| IgM | (204) |
| Orosomucoid | (205) |
| miRNAs | (206) |
IL, Interleukin; TNF, Tumor Necrosis Factor; IL-18BP, Interleukin-18 Binding Protein; α: Alpha VGEF, Vascular Endothelial Growth Factor; MMP, Matrix Metalloproteinases; MCP, Monocyte Chemoattractant Protein; MIP, Macrophage Inflammatory Protein; NGAL: Neutrophil Gelatinase-Associated Lipocalin; TNFR1, Tumor Necrosis Factor Receptor-1; PET PIB, positron emission tomography, radiotracer Pittsburgh Compound-B; NNAL, 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol; DHBA, 3, 5-dihydroxy-benzoic acid (DHBA); DHPPA, 3-(3, 5-dihydroxyphenyl)-1-propanoic acid; CTX, carboxy-terminal cross-linking telopeptide of type I collagen; DPD, deoxypyridinoline (lysylpyridinoline); NTX, N-terminal cross-linking telopeptide of type I collagen; IGKC, immunoglobulin kappa chain C; RBP4, retinol binding protein 4; ORM1, α-1-acid glycoprotein 1; IGLC2, immunoglobulin lambda-2 chain C; A1MG, Alpha-1-microglobulin; DMPN, dimethylpyrrole norleucine; DMPN NAC, cysteine-pyrrole conjugate; DMPN GSH, glutathione-pyrrole conjugate; 2,5-DMP, 2,5-dimethylpyrrole; AD7c-NTP, Alzheimer-associated neuronal thread protein.
Figure 2.
Urinary biomarkers linked with diagnosis, prevention, and treatment of various diseases. (A color version of this figure is available in the online journal.)
Cancer
Cancer can also be diagnosed with urine biomarkers. In a study with transitional cell carcinoma (TCC) in dogs, a total of 379 proteins were identified and 96 were unique to the TCC animals. This indicates that these biomarkers can be used for diagnosing cancer such as TCC.207 Methylation of several tumor suppressor genes is also correlated with clinicopathological variables and diagnosis of diseases. The presence of the methylated tumor suppressor genes CCND2, SCGB3A1, BNIP3, ID4, and RUNX3 in the urine of bladder cancer patients represents the usefulness of urine not only for diagnostic assessment but also as independent bladder cancer prognosticators.119 VEGF and endostatin were also found higher in urine of patients with bladder cancer than those in patients with urological disorders and healthy controls. Thus, urine levels of VEGF and endostatin could be a clinically useful aid in the diagnosis of bladder cancer.208
Urine biomarkers are useful as indicators in cancer prevention. The DNA damage caused by N-nitroso compound in red meat-consuming people has been detected in urine. Taking this DNA damage in account, some types of cancer such as colorectal cancer can be prevented by dietary manipulation.209 In high-grade prostatic intraepithelial neoplasia or prostate cancer patients, urinary F2-isoprostane provides a biomarker for the role for oxidative stress in prostate carcinogenesis. Thus, F2-isoprostanes may also serve to target oxidative stress mechanisms in prostate cancer prevention or treatment.210 Besides these, antioxidant status such as glutathione S-transferase,211 urine pH,212 and other biomarkers can play a role in preventing diseases including some types of cancer. Additionally, the presence of tea polyphenol metabolites in tea-consuming individual indicates its significance in cancer prevention, since tea polyphenols are a well-known cancer preventive agent.213
Accumulated evidence suggests that urine biomarkers have important applications in the monitoring of disease treatment including cancer. In a study with cancer patients, a high level of cyclic guanosine 3’,5’ monophosphate (cyclic GMP) urine biomarker has been found. However, successful cancer treatment was found to be accompanied by a dramatic fall in the urine cyclic GMP concentrations, whereas if the treatment was unsuccessful the level did not change.214 Similarly, in bladder cancer patients, the presence of IL-2 in the urine was demonstrated. IL-2 production was found to be directly related to the Bacillus Calmette–Guérin (BCG; a vaccine) administration as samples obtained just before the BCG instillation were always negative and urine became positive after the third or fourth BCG instillation.215 An increase in the number of granulocytes, monocytes/macrophages, and T-lymphocytes in urine after intravesical BCG administration was also demonstrated in bladder cancer patients, indicating a role for urine biomarkers in the determination of local activation of the immune system.216 Recently, the biomarkers cytokeratin 18, M30, and M65 have been investigated in urine to determine the response to BCG therapy of patients with bladder cancer. High levels of both M30 and M65 were found in all patients within 24 h after treatment; however, the return of both M30 and M65 levels in the urine to normal levels within five days or more was also observed as associated with complete remission.217
Neurological disorders
Increased levels of Alzheimer-associated neuronal thread protein (AD7c-NTP) are often detected in urine in the early in the course of Alzheimer’s disease. The level of urinary AD7c-NTP and apolipoprotein E ε4 in patients with mild cognitive impairment was also found higher than in healthy people, which suggests that the level of urinary AD7c-NTP may be an important biomarker for the early diagnosis of mild cognitive impairment and Alzheimer’s disease.167,218 The detection of drugs in urine samples from patients of Parkinson’s disease undergoing therapy with pramipexole, R(−)-apomorphine, (R−)-apocodeine, and R(−)-norapomorphine also indicates the association of urine in neurological diseases.167,219 Another study showed that a higher concentration of 5- and 6-hydroxydopamine in the urine of dopamine treated Parkinson’s patients than the normal controls.220 This further associates urine and disease treatment. Chronic exposure of manganese has also shown to contribute to the development of neurological syndrome. The detection of elevated levels of manganese in urine can be used as a primary marker, which can be helpful in the prevention of neurological diseases.221
Diabetes
It has been found that the amounts of urea and creatinine decreased from normal to low risk and high risk of diabetes, and the amount of glucose increased in the urine of diabetic patients compared to healthy individuals. Thus, it can be concluded that urine provides diagnostic information of possible complications and a better disease prognosis.222 Also, the presence of urine miRNAs,223 haptoglobin levels,224 and several other proteins can be used as diagnostic tools for diabetes.
The American Diabetic Association recommended aspirin therapy as a primary prevention of the disease mellitus. However, it has several limitations. The presence of microalbumin and macroalbumin in urine has reported in the patients of type 2 diabetics treated with aspirin as preventive measure,225 indicating its role in prevention of diseases. Albuminuria in the urine of diabetic patients has also determined for prevention and control of diabetic nephropathy.226 Urine biomarkers are also linked to the treatment of numerous other diseases. In case of diabetes treatment by amiloride, urinary plasminogen and albumin excretions were found to be significantly reduced. Urokinase activity was detectable in macroalbuminuric urine, with a tendency toward reduction in activity after amiloride treatment.227
Renal diseases
The urine marker neutrophil gelatinase-associated lipocalin has been demonstrated to be useful in the early diagnosis of acute kidney injury.228 High urine levels of annexin A1 (ANXA1) protein have been demonstrated as an index for glomerular injury. Thus, ANXA1 could be universal biomarker for the early diagnosis, prediction, and outcome monitoring of glomerular injury.229 Chronic exposure to cadmium causes renal proximal tubular dysfunction, and the level of cadmium in urine is generally regarded as an indicator of cadmium body burden. Therefore, timely determination of urinary cadmium levels and proteinuria can prevent the incidence of diseases caused by cadmium exposure.230
Other
Tight junction breakdown, with loss of the important sealing protein claudin-3, is an early event in the development of intestinal damage. Both experimental and clinical studies showed an increased urine claudin-3 protein, indicating a strong relation between intestinal tight junction loss and urinary claudin-3 levels that is useful in diagnosis.231 These findings suggest that measurement of urinary claudin-3 can be used as non-invasive marker for intestinal tight junction loss. It has been also observed that patients with endometriosis have a unique cluster of peptides in urine, and peptide proteomic profiling provides a novel method for non-invasive diagnosis of endometriosis.232 Sylvester et al.233 identified seven urine proteins capable of providing highly accurate diagnostic and prognostic information for infants with suspected necrotizing enterocolitis, which could be helpful in improving the efficiency and early diagnosis of this disease.
Saliva- and urine-based biosensors for diagnosis
Over the last 20 years, the development of rapid, selective, sensitive, and cost effective sensors have been a major interest in the bioanalytical sciences. Currently, much effort is being invested in the research of new materials toward the development of electrochemical biosensors with low detection limits.234 Because of their unique specificity and detection of low concentrations of specific biomarkers, electrochemical biosensors are attractive for analytical applications.235 Saliva and urine have been used as diagnostic media in recent years. The biomarkers contained in saliva and urine can be detected by biosensors and used for the determination of various specific biochemical parameters to diagnose correlated diseases.
Basically, urine is considered an ideal biofluid for clinical investigation without any harm to patients. The determination of high concentration of the protein cathepsin D in urine can be used as a tumor marker in the diagnosis of bladder cancer. Recently, Gorodkiewicz et al.236 reported that cathepsin D concentration in the urine of bladder cancer patients was very high (1.35–7.14 ng/mL) compare to healthy donors (N = 54) (0.32–0.68 ng/mL). A gas chromatography-sensor device was used for the diagnosis of bladder cancer based on volatile metabolites in urine. Urine samples were taken from 24 patients with urothelial cell carcinoma and 74 controls presenting with urological symptoms, but without a urological malignancy. By using the leave-one-out cross-validation method, 95.8% of cancer cases were correctly predicted with 93.2% of controls.237 Analysis of the volatile metabolites in urine headspace by selected ion flow tube mass spectrometry was used for the profiling of gastro-esophageal cancer. Samples were retrieved from patients with gastro-esophageal cancer, noncancer diseases of the upper gastro-intestinal tract, and a healthy cohort. Seven volatile organic compounds (acetaldehyde, acetone, acetic acid, hexanoic acid, hydrogen sulfide, methanol and phenol) were found to be significantly increased in the cancer cohort compared to positive control and healthy groups.238 High urinary MMP-7 levels revealed the presence of lymph node metastases, and an antibody-based electrical biochip technology was also developed for the quantitative detection of urinary MMP-7.239 In this study, urine samples were acquired from 30 bladder cancer patients and 15 healthy individuals of similar age. The concentration of MMP-7 was significantly higher in patients with metastatic bladder cancer compared to others. Electrochemical sensing of prostate-specific membrane antigens, which is well known as a prostate cancer biomarker in urine, could revolutionize cancer diagnosis and treatment.240
Successful measurement of salivary markers reveals that saliva samples can play diagnostic roles in various diseases. As cancer is caused by the accumulation of mutations in various genes that inactivate tumor suppressor genes and activate proto-oncogenes, tumor-specific genetic markers for cancer cells were studied in patients’ saliva. The p53 gene mutation in HNSCCs was sequenced and used retrospectively as tumor-specific genetic markers in saliva, and determined that tumor-specific mutations in preoperative saliva samples were 71% (5 out of 7 patients).241 Because of constitutive activation and high mutations rate in EGFR, it is very common abnormal expression in non-small cell lung carcinoma (NSCLC), therefore noninvasive, accurate, rapid, user-friendly, inexpensive detection and monitoring of EGFR mutations in NSCLC patients is highly desired. Electric field-induced release and measurement was approved as a saliva-based EGFR mutation detection technique in saliva samples from 40 patients with NSCLC.242 Saliva is used for the detection and quantification of cytokine level to treat various diseases such as OSCC. In a study, the quantification of picomolar IL-8 concentrations in human saliva was determined by using Biacore surface plasmon resonance in a microfluidic channel. IL-8 protein in the saliva of healthy individuals, and patients with OSCC were 30 pmol/L and 86 pmol/L, respectively.243
Generally, a surface-immobilized optical protein sensor is applied to detect oral cancer marker IL-8 with a limit of detection (LOD) at 1 pmol/L in buffer. Confocal optics-based sensor for further reducing the optical noise and extend the LOD of the surface immobilized optical protein sensor has been developed to detect IL-8 protein at 4.0 fmol/L in buffer.244 In this report, saliva samples of 20 oral cancer patients and 20 controls were determined to compare the sensitivity and accuracy of optical protein sensor with traditional enzyme-linked immunosorbent assay values. Nano-biochips (the integration of semiconductor nanoparticle quantum dots into a modular and microfluidic biosensor) were also used for the determinations of cancer biomarkers, carcino-embryonic antigen, cancer antigen 125, and Her-2/Neu in saliva.245
Acknowledgment
The authors thank Claire E Blondeau from the Department of Scientific Publications for carefully proofreading the manuscript. This work was supported by a grant from the Center for Targeted Therapy of The University of Texas MD Anderson Cancer Center and Jarrow Formulas, California. Dr Aggarwal is the Ransom Horne, Jr, Professor of Cancer Research.
Author contributions
SP and AKT participated in collecting data and reviewing all articles cited in the paper. SP wrote the manuscript. BBA developed concept and supervised in structuring the manuscript. All authors read and approved the final manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Yadav VR, Prasad S, Sung B, Kannappan R, Aggarwal BB. Targeting inflammatory pathways by triterpenoids for prevention and treatment of cancer. Toxins 2010; 2: 2428–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res 2009; 15: 425–30. [DOI] [PubMed] [Google Scholar]
- 3.Prasad S, Phromnoi K, Yadav VR, Chaturvedi MM, Aggarwal BB. Targeting inflammatory pathways by flavonoids for prevention and treatment of cancer. Planta Med 2010; 76: 1044–63. [DOI] [PubMed] [Google Scholar]
- 4.Prasad S, Sung B, Aggarwal BB. Age-associated chronic diseases require age-old medicine: role of chronic inflammation. Prev Med 2012; 54: S29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heidland A, Klassen A, Rutkowski P, Bahner U. The contribution of Rudolf Virchow to the concept of inflammation: what is still of importance? J Nephrol 2006; 19: S102–9. [PubMed] [Google Scholar]
- 6.Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochem Pharmacol 2006; 72: 1605–21. [DOI] [PubMed] [Google Scholar]
- 7.Lavrovsky Y, Chatterjee B, Clark RA, Roy AK. Role of redox-regulated transcription factors in inflammation, aging and age-related diseases. Exp Gerontol 2000; 35: 521–32. [DOI] [PubMed] [Google Scholar]
- 8.Rahman I. Oxidative stress, chromatin remodeling and gene transcription in inflammation and chronic lung diseases. J Biochem Mol Biol 2003; 36: 95–109. [DOI] [PubMed] [Google Scholar]
- 9.Aggarwal BB, Prasad S, Reuter S, Kannappan R, Yadev VR, Park B, Kim JH, Gupta SC, Phromnoi K, Sundaram C, Prasad S, Chaturvedi MM, Sung B. Identification of novel anti-inflammatory agents from ayurvedic medicine for prevention of chronic diseases: “reverse pharmacology” and “bedside to bench” approach. Curr Drug Targets 2011; 12: 1595–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aggarwal BB, Gupta SC, Sung B. Curcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. Br J Pharmacol 2013; 169: 1672–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aggarwal BB, Gehlot P. Inflammation and cancer: how friendly is the relationship for cancer patients? Curr Opin Pharmacol 2009; 9: 351–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malamud D. Saliva as a diagnostic fluid. Dent Clin N Am 2011; 55: 159–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rahim MA, Rahim ZH, Ahmad WA, Hashim OH. Can saliva proteins be used to predict the onset of acute myocardial infarction among high-risk patients? Int J Med Sci 2015; 12: 329–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beretov J, Wasinger VC, Graham PH, Millar EK, Kearsley JH, Li Y. Proteomics for breast cancer urine biomarkers. Adv Clin Chem 2014; 63: 123–67. [DOI] [PubMed] [Google Scholar]
- 15.Ceccato F, Barbot M, Zilio M, Ferasin S, Occhi G, Daniele A, Mazzocut S, Iacobone M, Betterle C, Mantero F, Scaroni C. Performance of salivary cortisol in the diagnosis of Cushing’s syndrome, adrenal incidentaloma, and adrenal insufficiency. Eur J Endocrinol 2013; 169: 31–6. [DOI] [PubMed] [Google Scholar]
- 16.Fransen K, Vermoesen T, Beelaert G, Menten J, Hutse V, Wouters K, Platteau T, Florence E. Using conventional HIV tests on oral fluid. J Virol Meth 2013; 194: 46–51. [DOI] [PubMed] [Google Scholar]
- 17.Kefalides NA, Monboisse JC, Bellon G, Ohno N, Ziaie Z, Shahan TA. Suppression of tumor cell growth by type IV collagen and a peptide from the NC1 domain of the alpha 3(IV) chain. Medicina 1999; 59: 553–553. [PubMed] [Google Scholar]
- 18.Streckfus C, Bigler L, Tucci M, Thigpen JT. A preliminary study of CA15-3, c-erbB-2, epidermal growth factor receptor, cathepsin-D, and p53 in saliva among women with breast carcinoma. Cancer Invest 2000; 18: 101–9. [DOI] [PubMed] [Google Scholar]
- 19.Chai RL, Grandis JR. Advances in molecular diagnostics and therapeutics in head and neck cancer. Curr Treat Options Oncol 2006; 7: 3–11. [DOI] [PubMed] [Google Scholar]
- 20.Robins SP. Collagen crosslinks in metabolic bone disease. Acta Orthopaed Scand Suppl 1995; 266: 171–5. [PubMed] [Google Scholar]
- 21.Kamel S, Brazier M, Neri V, Picard C, Samson L, Desmet G, Sebert JL. Multiple molecular forms of pyridinolines cross-links excreted in human urine evaluated by chromatographic and immunoassay methods. J Bone Miner Res 1995; 10: 1385–92. [DOI] [PubMed] [Google Scholar]
- 22.Mlcochova H, Hezova R, Stanik M, Slaby O. Urine microRNAs as potential noninvasive biomarkers in urologic cancers. Urol Oncol 2014; 32: 41 e1–9. [DOI] [PubMed] [Google Scholar]
- 23.Sysi-Aho M, Ermolov A, Gopalacharyulu PV, Tripathi A, Seppanen-Laakso T, Maukonen J, Mattila I, Ruohonen ST, Vähätalo L, Yetukuri L, Härkönen T, Lindfors E, Nikkilä J, Ilonen J, Simell O, Saarela M, Knip M, Kaski S, Savontaus E, Orešič M. Metabolic regulation in progression to autoimmune diabetes. PLoS Comput Biol 2011; 7: e1002257–e1002257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bathe OF, Shaykhutdinov R, Kopciuk K, Weljie AM, McKay A, Sutherland FR, Dixon E, Dunse N, Sotiropoulos D, Vogel HJ. Feasibility of identifying pancreatic cancer based on serum metabolomics. Cancer Epidemiol Biomarkers Prev 2011; 20: 140–7. [DOI] [PubMed] [Google Scholar]
- 25.Rhodus NL, Cheng B, Myers S, Miller L, Ho V, Ondrey F. The feasibility of monitoring NF-kappaB associated cytokines: TNF-alpha, IL-1alpha, IL-6, and IL-8 in whole saliva for the malignant transformation of oral lichen planus. Mol Carcinog 2005; 44: 77–82. [DOI] [PubMed] [Google Scholar]
- 26.Katakura A, Kamiyama I, Takano N, Shibahara T, Muramatsu T, Ishihara K, Takagi R, Shouno T. Comparison of salivary cytokine levels in oral cancer patients and healthy subjects. Bull Tokyo Dent Coll 2007; 48: 199–203. [DOI] [PubMed] [Google Scholar]
- 27.Pickering V, Jordan RC, Schmidt BL. Elevated salivary endothelin levels in oral cancer patients–a pilot study. Oral Oncol 2007; 43: 37–41. [DOI] [PubMed] [Google Scholar]
- 28.Mizukawa N, Sugiyama K, Fukunaga J, Ueno T, Mishima K, Takagi S, Sugahara T. Defensin-1, a peptide detected in the saliva of oral squamous cell carcinoma patients. Anticancer Res 1998; 18: 4645–9. [PubMed] [Google Scholar]
- 29.Metgud R, Patel S. Serum and salivary levels of albumin as diagnostic tools for oral pre-malignancy and oral malignancy. Biotech Histochem 2014; 89: 8–13. [DOI] [PubMed] [Google Scholar]
- 30.Nagler R, Bahar G, Shpitzer T, Feinmesser R. Concomitant analysis of salivary tumor markers–a new diagnostic tool for oral cancer. Clin Cancer Res 2006; 12: 3979–84. [DOI] [PubMed] [Google Scholar]
- 31.Almadori G, Bussu F, Galli J, Limongelli A, Persichilli S, Zappacosta B, Minucci A, Paludetti G, Giardina B. Salivary glutathione and uric acid levels in patients with head and neck squamous cell carcinoma. Head Neck 2007; 29: 648–54. [DOI] [PubMed] [Google Scholar]
- 32.Dowling P, Wormald R, Meleady P, Henry M, Curran A, Clynes M. Analysis of the saliva proteome from patients with head and neck squamous cell carcinoma reveals differences in abundance levels of proteins associated with tumour progression and metastasis. J Proteom 2008; 71: 168–75. [DOI] [PubMed] [Google Scholar]
- 33.Hu S, Arellano M, Boontheung P, Wang J, Zhou H, Jiang J, Elashoff D, Wei R, Loo JA, Wong DT. Salivary proteomics for oral cancer biomarker discovery. Clin Cancer Res 2008; 14: 6246–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Warnakulasuriya S, Soussi T, Maher R, Johnson N, Tavassoli M. Expression of p53 in oral squamous cell carcinoma is associated with the presence of IgG and IgA p53 autoantibodies in sera and saliva of the patients. J Pathol 2000; 192: 52–7. [DOI] [PubMed] [Google Scholar]
- 35.Jessie K, Jayapalan JJ, Ong KC, Abdul Rahim ZH, Zain RM, Wong KT, Hashim OH. Aberrant proteins in the saliva of patients with oral squamous cell carcinoma. Electrophoresis 2013; 34: 2495–502. [DOI] [PubMed] [Google Scholar]
- 36.Yang SF, Chen MK, Hsieh YS, Chung TT, Hsieh YH, Lin CW, Su JL, Tsai MH, Tang CH. Prostaglandin E2/EP1 signaling pathway enhances intercellular adhesion molecule 1 (ICAM-1) expression and cell motility in oral cancer cells. J Biol Chem 2010; 285: 29808–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, Xi L, Gooding W, Godfrey TE, Ferris RL. Chemokine receptors 6 and 7 identify a metastatic expression pattern in squamous cell carcinoma of the head and neck. Adv Otorhinolaryngol 2005; 62: 121–33. [DOI] [PubMed] [Google Scholar]
- 38.Farmer RW, Richtsmeier WJ, Scher RL. Identification of sialyl Lewis-x in squamous cell carcinoma of the head and neck. Head Neck 1998; 20: 726–31. [DOI] [PubMed] [Google Scholar]
- 39.Vlkova B, Stanko P, Minarik G, Tothova L, Szemes T, Banasova L, Novotňáková D, Hodosy J, Celec P. Salivary markers of oxidative stress in patients with oral premalignant lesions. Arch Oral Biol 2012; 57: 1651–6. [DOI] [PubMed] [Google Scholar]
- 40.Goncalves AS, Arantes DA, Bernardes VF, Jaeger F, Silva JM, Silva TA, guiar MC, Batista AC. Immunosuppressive mediators of oral squamous cell carcinoma in tumour samples and saliva. Hum Immunol 2015; 76: 52–8. [DOI] [PubMed] [Google Scholar]
- 41.Mu AK, Chan YS, Kang SS, Azman SN, Zain RB, Chai WL, Chen Y. Detection of host-specific immunogenic proteins in the saliva of patients with oral squamous cell carcinoma. J Immunoassay Immunochem 2014; 35: 183–93. [DOI] [PubMed] [Google Scholar]
- 42.Wang Q, Gao P, Wang X, Duan Y. Investigation and identification of potential biomarkers in human saliva for the early diagnosis of oral squamous cell carcinoma. Clin Chim Acta 2014; 427: 79–85. [DOI] [PubMed] [Google Scholar]
- 43.Salazar C, Nagadia R, Pandit P, Cooper-White J, Banerjee N, Dimitrova N, Coman WB, Punyadeera C. A novel saliva-based microRNA biomarker panel to detect head and neck cancers. Cell Oncol 2014; 37: 331–8. [DOI] [PubMed] [Google Scholar]
- 44.Navarro MA, Mesia R, Diez-Gibert O, Rueda A, Ojeda B, Alonso MC. Epidermal growth factor in plasma and saliva of patients with active breast cancer and breast cancer patients in follow-up compared with healthy women. Breast Cancer Res Treat 1997; 42: 83–6. [DOI] [PubMed] [Google Scholar]
- 45.Pink R, Simek J, Vondrakova J, Faber E, Michl P, Pazdera J, Indrak K. Saliva as a diagnostic medium. Biomedical papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia 2009; 153(2): 103–10. [DOI] [PubMed] [Google Scholar]
- 46.Jenzano JW, Courts NF, Timko DA, Lundblad RL. Levels of glandular kallikrein in whole saliva obtained from patients with solid tumors remote from the oral cavity. J Dent Res 1986; 65: 67–70. [DOI] [PubMed] [Google Scholar]
- 47.Schapher M, Wendler O, Groschl M, Schafer R, Iro H, Zenk J. Salivary leptin as a candidate diagnostic marker in salivary gland tumors. Clin Chem 2009; 55: 914–22. [DOI] [PubMed] [Google Scholar]
- 48.Trubnikov GA, Sukharev AE, Uklistaia TA, Orlova EA. [Clinico-diagnostic role of ferritin and lactoferrin assays in benign and malignant affections of lungs and pleura]. Klin Med 1998; 76: 21–6. [PubMed] [Google Scholar]
- 49.Fine DH, Markowitz K, Furgang D, Fairlie K, Ferrandiz J, Nasri C, McKiernan M, Donnelly R, Gunsolley J. Macrophage inflammatory protein-1alpha: a salivary biomarker of bone loss in a longitudinal cohort study of children at risk for aggressive periodontal disease? J Periodontol 2009; 80: 106–13. [DOI] [PubMed] [Google Scholar]
- 50.Al-Sabbagh M, Alladah A, Lin Y, Kryscio RJ, Thomas MV, Ebersole JL, Miller CS. Bone remodeling-associated salivary biomarker MIP-1alpha distinguishes periodontal disease from health. J Periodontal Res 2012; 47: 389–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gupta M, Chaturvedi R, Jain A. Role of monocyte chemoattractant protein-1 (MCP-1) as an immune-diagnostic biomarker in the pathogenesis of chronic periodontal disease. Cytokine 2013; 61: 892–7. [DOI] [PubMed] [Google Scholar]
- 52.Rai B, Kharb S, Jain R, Anand SC. Biomarkers of periodontitis in oral fluids. J Oral Sci 2008; 50: 53–6. [DOI] [PubMed] [Google Scholar]
- 53.Sundar NM, Krishnan V, Krishnaraj S, Hemalatha VT, Alam MN. Comparison of the salivary and the serum nitric oxide levels in chronic and aggressive periodontitis: a biochemical study. J Clin Diagn Res JCDR 2013; 7: 1223–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bathena SP, Huang J, Nunn ME, Miyamoto T, Parrish LC, Lang MS, McVaney TP, Toews ML, Cerutis DR, Alnouti Y. Quantitative determination of lysophosphatidic acids (LPAs) in human saliva and gingival crevicular fluid (GCF) by LC-MS/MS. J Pharm Biomed Anal 2011; 56: 402–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bostanci N, Ozturk VO, Emingil G, Belibasakis GN. Elevated oral and systemic levels of soluble triggering receptor expressed on myeloid cells-1 (sTREM-1) in periodontitis. J Dent Res 2013; 92: 161–5. [DOI] [PubMed] [Google Scholar]
- 56.Yoon AJ, Cheng B, Philipone E, Turner R, Lamster IB. Inflammatory biomarkers in saliva: assessing the strength of association of diabetes mellitus and periodontal status with the oral inflammatory burden. J Clin Periodontol 2012; 39: 434–40. [DOI] [PubMed] [Google Scholar]
- 57.Ebersole JL, Schuster JL, Stevens J, Dawson D, 3rd, Kryscio RJ, Lin Y, Thomas MV, Miller CS. Patterns of salivary analytes provide diagnostic capacity for distinguishing chronic adult periodontitis from health. J Clin Immunol 2013; 33: 271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Glimvall P, Wickstrom C, Jansson H. Elevated levels of salivary lactoferrin, a marker for chronic periodontitis? J Periodontal Res 2012; 47: 655–60. [DOI] [PubMed] [Google Scholar]
- 59.Sezer ED, Aksu K, Caglayan O, Keser G, Karabulut G, Ercan G. DNA damage and its relationship with other oxidative stress parameters in Behcet’s disease. Rheumatol Int 2012; 32: 217–22. [DOI] [PubMed] [Google Scholar]
- 60.Choi YJ, Heo SH, Lee JM, Cho JY. Identification of azurocidin as a potential periodontitis biomarker by a proteomic analysis of gingival crevicular fluid. Proteome Sci 2011; 9: 42–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Salazar MG, Jehmlich N, Murr A, Dhople VM, Holtfreter B, Hammer E, Völker U, Kocher T. Identification of periodontitis associated changes in the proteome of whole human saliva by mass spectrometric analysis. J Clin Periodontol 2013; 40: 825–32. [DOI] [PubMed] [Google Scholar]
- 62.Mendoza-Nunez VM, Hernandez-Monjaraz B, Santiago-Osorio E, Betancourt-Rule JM, Ruiz-Ramos M. Tai Chi exercise increases SOD activity and total antioxidant status in saliva and is linked to an improvement of periodontal disease in the elderly. Oxid Med Cell Longevity 2014; 2014: 603853–603853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Baltacioglu E, Yuva P, Aydin G, Alver A, Kahraman C, Karabulut E, Akalın FA. Lipid peroxidation levels and total oxidant/antioxidant status in serum and saliva from patients with chronic and aggressive periodontitis. Oxidative stress index: a new biomarker for periodontal disease? J Periodontol 2014; 85: 1432–41. [DOI] [PubMed] [Google Scholar]
- 64.Zhang WY, Liu W, Zhou YM, Shen XM, Wang YF, Tang GY. Altered microRNA expression profile with miR-27b down-regulation correlated with disease activity of oral lichen planus. Oral Dis 2012; 18: 265–70. [DOI] [PubMed] [Google Scholar]
- 65.Liu W, Dan H, Wang Z, Jiang L, Zhou Y, Zhao M, Chen Q, Zeng X. IFN-gamma and IL-4 in saliva of patients with oral lichen planus: a study in an ethnic Chinese population. Inflammation 2009; 32: 176–81. [DOI] [PubMed] [Google Scholar]
- 66.Janardhanam SB, Prakasam S, Swaminathan VT, Kodumudi KN, Zunt SL, Srinivasan M. Differential expression of TLR-2 and TLR-4 in the epithelial cells in oral lichen planus. Arch Oral Biol 2012; 57: 495–502. [DOI] [PubMed] [Google Scholar]
- 67.Liu WZ, He MJ, Long L, Mu DL, Xu MS, Xing X, Zeng X, Liao G, Dan HX, Chen QM. Interferon-gamma and interleukin-4 detected in serum and saliva from patients with oral lichen planus. Int J Oral Sci 2014; 6: 22–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gornowicz A, Bielawska A, Bielawski K, Grabowska SZ, Wojcicka A, Zalewska M, Maciorkowska E. Pro-inflammatory cytokines in saliva of adolescents with dental caries disease. Ann Agric Environ Med AAEM 2012; 19: 711–6. [PubMed] [Google Scholar]
- 69.Zhao A, Blackburn C, Chin J, Srinivasan M. Soluble toll like receptor 2 (TLR-2) is increased in saliva of children with dental caries. BMC Oral Health 2014; 14: 108–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hegde MN, Hegde ND, Ashok A, Shetty S. Biochemical indicators of dental caries in saliva: an in vivo study. Caries Res 2014; 48: 170–3. [DOI] [PubMed] [Google Scholar]
- 71.Gabryel-Porowska H, Gornowicz A, Bielawska A, Wojcicka A, Maciorkowska E, Grabowska SZ, Bielawski K. Mucin levels in saliva of adolescents with dental caries. Med Sci Monit 2014; 20: 72–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zidverc-Trajkovic J, Stanimirovic D, Obrenovic R, Tajti J, Vecsei L, Gardi J, Németh J, Mijajlovic M, Sternic N, Jankovic L. Calcitonin gene-related peptide levels in saliva of patients with burning mouth syndrome. J Oral Pathol Med 2009; 38: 29–33. [DOI] [PubMed] [Google Scholar]
- 73.Hernandez-Molina G, Michel-Peregrina M, Hernandez-Ramirez DF, Sanchez-Guerrero J, Llorente L. Chemokine saliva levels in patients with primary Sjogren’s syndrome, associated Sjogren’s syndrome, pre-clinical Sjogren’s syndrome and systemic autoimmune diseases. Rheumatology 2011; 50: 1288–92. [DOI] [PubMed] [Google Scholar]
- 74.Kramer JM, Klimatcheva E, Rothstein TL. CXCL13 is elevated in Sjogren’s syndrome in mice and humans and is implicated in disease pathogenesis. J Leukoc Biol 2013; 94: 1079–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cuida M, Halse AK, Johannessen AC, Tynning T, Jonsson R. Indicators of salivary gland inflammation in primary Sjogren’s syndrome. Eur J Oral Sci 1997; 105: 228–33. [DOI] [PubMed] [Google Scholar]
- 76.Ciccia F, Guggino G, Rizzo A, Ferrante A, Raimondo S, Giardina A, Dieli F, Campisi G, Alessandro R, Triolo G. Potential involvement of IL-22 and IL-22-producing cells in the inflamed salivary glands of patients with Sjogren’s syndrome. Ann Rheum Dis 2012; 71: 295–301. [DOI] [PubMed] [Google Scholar]
- 77.Delaleu N, Mydel P, Kwee I, Brun JG, Jonsson MV, Jonsson R. High fidelity between saliva proteomics and the biologic state of salivary glands defines biomarker signatures for primary Sjogren’s syndrome. Arthritis Rheumatol 2015; 67: 1084–95. [DOI] [PubMed] [Google Scholar]
- 78.Szczeklik K, Owczarek D, Pytko-Polonczyk J, Kesek B, Mach TH. Proinflammatory cytokines in the saliva of patients with active and non-active Crohn’s disease. Pol Arch Med Wewn 2012; 122: 200–8. [DOI] [PubMed] [Google Scholar]
- 79.DeSantis AS, DiezRoux AV, Hajat A, Aiello AE, Golden SH, Jenny NS, Seeman TE, Shea S. Associations of salivary cortisol levels with inflammatory markers: the Multi-Ethnic Study of Atherosclerosis. Psychoneuroendocrinology 2012; 37: 1009–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Al-Nimer MS, Mshatat SF, Abdulla HI. Saliva alpha-synuclein and a high extinction coefficient protein: a novel approach in assessment biomarkers of Parkinson’s disease. N Am J Med Sci 2014; 6: 633–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Thorman R, Lundahl J, Yucel-Lindberg T, Hylander B. Inflammatory cytokines in saliva: early signs of metabolic disorders in chronic kidney disease. A controlled cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2010; 110: 597–604. [DOI] [PubMed] [Google Scholar]
- 82.Eisenberg E, Shtahl S, Geller R, Reznick AZ, Sharf O, Ravbinovich M, Erenreich A, Nagler RM. Serum and salivary oxidative analysis in complex regional pain syndrome. Pain 2008; 138: 226–32. [DOI] [PubMed] [Google Scholar]
- 83.Rezaie A, Khalaj S, Shabihkhani M, Nikfar S, Zamani MJ, Mohammadirad A, Daryani NE, Abdollahi M. Study on the correlations among disease activity index and salivary transforming growth factor-beta 1 and nitric oxide in ulcerative colitis patients. Ann N Y Acad Sci 2007; 1095: 305–14. [DOI] [PubMed] [Google Scholar]
- 84.Border MB, Schwartz S, Carlson J, Dibble CF, Kohltfarber H, Offenbacher S, Use JB, Bencharit S. Exploring salivary proteomes in edentulous patients with type 2 diabetes. Mol Biosyst 2012; 8: 1304–10. [DOI] [PubMed] [Google Scholar]
- 85.Mook-Kanamori DO, Selim MM, Takiddin AH, Al-Homsi H, Al-Mahmoud KA, Al-Obaidli A, Zirie MA, Rowe J, Yousri NA, Karoly ED, Kocher T, Sekkal Gherbi W, Chidiac OM, Mook-Kanamori MJ, Abdul Kader S, Al Muftah WA, McKeon C, Suhre K. 1,5-Anhydroglucitol in saliva is a noninvasive marker of short-term glycemic control. J Clin Endocrinol Metab 2014; 99: E479–83. [DOI] [PubMed] [Google Scholar]
- 86.Zalewska-Szajda B, Dariusz Szajda S, Waszkiewicz N, Chojnowska S, Goscik E, Lebkowska U, Kępka A, Bossowski A, Zalewska A, Janica J, Zwierz K, Ładny JR, Waszkiel D. Activity of N-acetyl-beta-D-hexosaminidase in the saliva of children with type 1 diabetes. Postepy Hig Med Dosw 2013; 67: 996–9. [DOI] [PubMed] [Google Scholar]
- 87.Su H, Velly AM, Salah MH, Benarroch M, Trifiro M, Schipper HM, Gornitsky M. Altered redox homeostasis in human diabetes saliva. J Oral Pathol Med 2012; 41: 235–41. [DOI] [PubMed] [Google Scholar]
- 88.Al-Rawi NH. Oxidative stress, antioxidant status and lipid profile in the saliva of type 2 diabetics. Diabetes Vasc Dis Res 2011; 8: 22–8. [DOI] [PubMed] [Google Scholar]
- 89.Soell M, Feki A, Hannig M, Sano H, Pinget M, Selimovic D. Chromogranin A detection in saliva of type 2 diabetes patients. Bosnian J Basic Med Sci 2010; 10: 2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arana C, Cutando A, Ferrera MJ, Gomez-Moreno G, Worf CV, Bolanos MJ, Escames G, Acuña-Castroviejo D. Parameters of oxidative stress in saliva from diabetic and parenteral drug addict patients. J Oral Pathol Med 2006; 35: 554–9. [DOI] [PubMed] [Google Scholar]
- 91.Yoon MS, Jankowski V, Montag S, Zidek W, Henning L, Schluter H, Tepel M, Jankowski J. Characterisation of advanced glycation endproducts in saliva from patients with diabetes mellitus. Biochem Biophys Res Commun 2004; 323: 377–81. [DOI] [PubMed] [Google Scholar]
- 92.Matias I, Gatta-Cherifi B, Tabarin A, Clark S, Leste-Lasserre T, Marsicano G, Piazza PV, Cota D. Endocannabinoids measurement in human saliva as potential biomarker of obesity. PloS One 2012; 7: e42399–e42399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ozcaka O, Ceyhan BO, Akcali A, Bicakci N, Lappin DF, Buduneli N. Is there an interaction between polycystic ovary syndrome and gingival inflammation? J Periodontol 2012; 83: 1529–37. [DOI] [PubMed] [Google Scholar]
- 94.Resende RG, Correia-Silva JD, Silva TA, Xavier SG, Bittencourt H, Gomez RS, Abreu MH. Saliva and blood interferon gamma levels and IFNG genotypes in acute graft-versus-host disease. Oral Dis 2012; 18: 816–22. [DOI] [PubMed] [Google Scholar]
- 95.Devic I, Shi M, Schubert MM, Lloid M, Izutsu KT, Pan C, Missaghi M, Morton TH, Mancl LA, Zhang J, Presland RB. Proteomic analysis of saliva from patients with oral chronic graft-versus-host disease. Biol Blood Marrow Transplant 2014; 20: 1048–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Rao NL, Shetty S, Upadhyaya K, Lobo RMP, Kedilaya EC, Prasad HPG. Salivary C-reactive protein in Hashimoto’s thyroiditis and subacute thyroiditis. Int J Inflam 2010; 2010: 514659–514659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.de Sousa RT, Zarate CA, Jr, Zanetti MV, Costa AC, Talib LL, Gattaz WF, Machado-Vieira R. Oxidative stress in early stage bipolar disorder and the association with response to lithium. J Psych Res 2014; 50: 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Cohen M, Khalaila R. Saliva pH as a biomarker of exam stress and a predictor of exam performance. J Psychosom Res 2014; 77: 420–5. [DOI] [PubMed] [Google Scholar]
- 99.Escribano D, Gutierrez AM, Fuentes-Rubio M, Ceron JJ. Saliva chromogranin A in growing pigs: a study of circadian patterns during daytime and stability under different storage conditions. Vet J 2014; 199: 355–9. [DOI] [PubMed] [Google Scholar]
- 100.van Holland BJ, Frings-Dresen MH, Sluiter JK. Measuring short-term and long-term physiological stress effects by cortisol reactivity in saliva and hair. Int Arch Occup Environ Health 2012; 85: 849–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Golshiri P, Pourabdian S, Najimi A, Zadeh HM, Hasheminia J. Job stress and its relationship with the level of secretory IgA in saliva: a comparison between nurses working in emergency wards and hospital clerks. J Pak Med Assoc 2012; 62: S26–30. [PubMed] [Google Scholar]
- 102.Aydin S, Aydin S, Kobat MA, Kalayci M, Eren MN, Yilmaz M, Kuloglu T, Gul E, Secen O, Alatas OD, Baydas A. Decreased saliva/serum irisin concentrations in the acute myocardial infarction promising for being a new candidate biomarker for diagnosis of this pathology. Peptides 2014; 56: 141–5. [DOI] [PubMed] [Google Scholar]
- 103.Phalane KG, Kriel M, Loxton AG, Menezes A, Stanley K, van der Spuy GD, Walzl G, Chegou NN. Differential expression of host biomarkers in saliva and serum samples from individuals with suspected pulmonary tuberculosis. Mediators inflamm 2013; 2013: 981984–981984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rubio MC, Gonzalez PM, Ramos C, Lewin PG, Friedman SM, Puntarulo S, Nicolosi LN. Oxidative stress assessed in saliva from patients with acute myocardial infarction. A preliminary study. Acta Odontol Latinoam 2013; 26: 116–20. [PubMed] [Google Scholar]
- 105.Toker A, Aribas A, Yerlikaya FH, Tasyurek E, Akbuga K. Serum and saliva levels of ischemia-modified albumin in patients with acute myocardial infarction. J Clin Lab Anal 2013; 27: 99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Mirzaii-Dizgah I, Hejazi SF, Riahi E, Salehi MM. Saliva-based creatine kinase MB measurement as a potential point-of-care testing for detection of myocardial infarction. Clin Oral Invest 2012; 16: 775–9. [DOI] [PubMed] [Google Scholar]
- 107.Cavas L, Arpinar P, Yurdakoc K. Possible interactions between antioxidant enzymes and free sialic acids in saliva: a preliminary study on elite judoists. Int J Sports Med 2005; 26: 832–5. [DOI] [PubMed] [Google Scholar]
- 108.Foley JD, 3rd, Sneed JD, Steinhubl SR, Kolasa J, Ebersole JL, Lin Y, Kryscio RJ, McDevitt JT, Campbell CL, Miller CS. Oral fluids that detect cardiovascular disease biomarkers. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114: 207–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Viet CT, Jordan RC, Schmidt BL. DNA promoter hypermethylation in saliva for the early diagnosis of oral cancer. J Calif Dental Assoc 2007; 35: 844–9. [PubMed] [Google Scholar]
- 110.Lallemant B, Evrard A, Combescure C, Chapuis H, Chambon G, Raynal C, Reynaud C, Sabra O, Joubert D, Hollande F, Lallemant JG, Lumbroso S, Brouillet JP. Clinical relevance of nine transcriptional molecular markers for the diagnosis of head and neck squamous cell carcinoma in tissue and saliva rinse. BMC Cancer 2009; 9: 370–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.el-Miedany YM, el-Hady SM, el-Baddin MA. Validity of the saliva ferning test for the diagnosis of dry mouth in Sjogren’s syndrome. Rev Rhumat 1999; 66: 73–8. [PubMed] [Google Scholar]
- 112.Hu S, Vissink A, Arellano M, Roozendaal C, Zhou H, Kallenberg CG, Wong DT. Identification of autoantibody biomarkers for primary Sjogren’s syndrome using protein microarrays. Proteomics 2011; 11: 1499–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Esmaili N, Mortazavi H, Kamyab-Hesari K, Aghazadeh N, Daneshpazhooh M, Khani S, Chams-Davatchi C. Diagnostic accuracy of BP180 NC16a and BP230-C3 ELISA in serum and saliva of patients with bullous pemphigoid. Clin Exp Dermatol 2015; 40: 324–30. [DOI] [PubMed] [Google Scholar]
- 114.Belstrom D, Fiehn NE, Nielsen CH, Kirkby N, Twetman S, Klepac-Ceraj V, Paster BJ, Holmstrup P. Differences in bacterial saliva profile between periodontitis patients and a control cohort. J Clin Periodontol 2014; 41: 104–12. [DOI] [PubMed] [Google Scholar]
- 115.Radzol AR, Lee KY, Mansor W. Nonstructural protein 1 characteristic peak from NS1-saliva mixture with surface-enhanced Raman spectroscopy. In: Conference proceedings: annual international conference of the IEEE engineering in medicine and biology society IEEE engineering in medicine and biology society annual conference. 03--07 July 2013, Osaka, Japan, pp.2396–9. [DOI] [PubMed]
- 116.Phumee A, Kraivichian K, Chusri S, Noppakun N, Vibhagool A, Sanprasert V, Tampanya V, Wilde H, Siriyasatien P. Detection of Leishmania siamensis DNA in saliva by polymerase chain reaction. Am J Trop Med Hyg 2013; 89: 899–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Holm-Hansen C, Nyombi B, Nyindo M. Saliva-based HIV testing among secondary school students in Tanzania using the OraQuick rapid HIV1/2 antibody assay. Ann N Y Acad Sci 2007; 1098: 461–6. [DOI] [PubMed] [Google Scholar]
- 118.Mellersh A, Clark A, Hafiz S. Inhibition of Neisseria gonorrhoeae by normal human saliva. Br J Venereal Dis 1979; 55: 20–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Garcia-Baquero R, Puerta P, Beltran M, Alvarez M, Sacristan R, Alvarez-Ossorio JL, Sánchez-Carbayo M. Methylation of a novel panel of tumor suppressor genes in urine moves forward noninvasive diagnosis and prognosis of bladder cancer: a 2-center prospective study. J Urol 2013; 190: 723–30. [DOI] [PubMed] [Google Scholar]
- 120.Tomita Y, Miyake N, Yamanaka S. Lipids in human parotid saliva with regard to caries experience. J Oleo Sci 2008; 57: 115–21. [DOI] [PubMed] [Google Scholar]
- 121.Abiko Y, Nishimura M, Kaku T. Defensins in saliva and the salivary glands. Med Electron Microsc 2003; 36: 247–52. [DOI] [PubMed] [Google Scholar]
- 122.Woltgens JH, Etty EJ, Gruythuysen RJ, Geraets WG. Influence of fluoride in saliva during the early cariogenic changes in the enamel of boys and girls. ASDC J Dent Child 1995; 62: 192–6. [PubMed] [Google Scholar]
- 123.Bal MV, Olgun A, Abasli D, Ozdemir A, Kursaklioglu H, Goktepe AS, Kurt Í. The effect of nonsurgical periodontal treatment on serum and saliva chitotriosidase activities in patients with periodontitis and coronary artery disease. Ther Clin Risk Manage 2015; 11: 53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Novakovic N, Cakic S, Todorovic T, Raicevic BA, Dozic I, Petrovic V, Perunović N, Gostović SS, Sretenović JK, Colak E. Antioxidative status of saliva before and after non-surgical periodontal treatment. Srp Arh Celok Lek 2013; 141: 163–8. [DOI] [PubMed] [Google Scholar]
- 125.Guentsch A, Preshaw PM, Bremer-Streck S, Klinger G, Glockmann E, Sigusch BW. Lipid peroxidation and antioxidant activity in saliva of periodontitis patients: effect of smoking and periodontal treatment. Clin Oral Invest 2008; 12: 345–52. [DOI] [PubMed] [Google Scholar]
- 126.Gorska R, Nedzi-Gora M. The effects of the initial treatment phase and of adjunctive low-dose doxycycline therapy on clinical parameters and MMP-8, MMP-9, and TIMP-1 levels in the saliva and peripheral blood of patients with chronic periodontitis. Arch Immunol Ther Exp 2006; 54: 419–26. [DOI] [PubMed] [Google Scholar]
- 127.Jentsch H, Sievert Y, Gocke R. Lactoferrin and other markers from gingival crevicular fluid and saliva before and after periodontal treatment. J Clin Periodontol 2004; 31: 511–4. [DOI] [PubMed] [Google Scholar]
- 128.Malhotra SL. New approaches to the pathogenesis of peptic ulcer based on the protective action of saliva with special reference to roughage, vegetable fibre and fermented milk products. Med Hypotheses 1978; 4: 1–14. [DOI] [PubMed] [Google Scholar]
- 129.Silva MJ, Reidy JA, Samandar E, Herbert AR, Needham LL, Calafat AM. Detection of phthalate metabolites in human saliva. Arch Toxicol 2005; 79: 647–52. [DOI] [PubMed] [Google Scholar]
- 130.Adam DJ, Milne AA, Evans SM, Roulston JE, Lee AJ, Ruckley CV, Bradbury AW. Serum amylase isoenzymes in patients undergoing operation for ruptured and non-ruptured abdominal aortic aneurysm. J Vasc Surg 1999; 30: 229–35. [DOI] [PubMed] [Google Scholar]
- 131.Margel D, Pevsner-Fischer M, Baniel J, Yossepowitch O, Cohen IR. Stress proteins and cytokines are urinary biomarkers for diagnosis and staging of bladder cancer. Eur Urol 2011; 59: 113–9. [DOI] [PubMed] [Google Scholar]
- 132.Urquidi V, Kim J, Chang M, Dai Y, Rosser CJ, Goodison S. CCL18 in a multiplex urine-based assay for the detection of bladder cancer. PloS One 2012; 7: e37797–e37797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gogalic S, Sauer U, Doppler S, Preininger C. Bladder cancer biomarker array to detect aberrant levels of proteins in urine. The Analyst 2015; 140: 724–35. [DOI] [PubMed] [Google Scholar]
- 134.Zhang G, Gomes-Giacoia E, Dai Y, Lawton A, Miyake M, Furuya H, Goodison S, Rosser CJ. Validation and clinicopathologic associations of a urine-based bladder cancer biomarker signature. Diagn Pathol 2014; 9: 200–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shichkin VP, Lon AD, Yugrinova LG, Grinevich YA, Belova OB, Berezhnaya NM, Akalovich S, Pashkova O, Voitenok NN. TNF receptor p55 and IL-8(72) and IL-8(77) isoforms: blood and urine levels in breast cancer patients. J Immunotoxicol 2009; 6: 235–42. [DOI] [PubMed] [Google Scholar]
- 136.Il’yasova D, Kennedy K, Spasojevic I, Wang F, Tolun AA, Base K, Young SP, Kelly Marcom P, Marks J, Millington DS, Dewhirst MW. Individual responses to chemotherapy-induced oxidative stress. Breast Cancer Res Treat 2011; 125: 583–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Faupel-Badger JM, Fuhrman BJ, Xu X, Falk RT, Keefer LK, Veenstra TD, Hoover RN, Ziegler RG. Comparison of liquid chromatography-tandem mass spectrometry, RIA, and ELISA methods for measurement of urinary estrogens. Cancer Epidemiol Biomarkers Prev 2010; 19: 292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xu X, Veenstra TD, Fox SD, Roman JM, Issaq HJ, Falk R, Saavedra JE, Keefer LK, Ziegler RG. Measuring fifteen endogenous estrogens simultaneously in human urine by high-performance liquid chromatography-mass spectrometry. Anal Chem 2005; 77: 6646–54. [DOI] [PubMed] [Google Scholar]
- 139.Woo HM, Kim KM, Choi MH, Jung BH, Lee J, Kong G, Nam SJ, Kim S, Bai SW, Chung BC. Mass spectrometry based metabolomic approaches in urinary biomarker study of women’s cancers. Clin Chim Acta 2009; 400: 63–9. [DOI] [PubMed] [Google Scholar]
- 140.Nam H, Chung BC, Kim Y, Lee K, Lee D. Combining tissue transcriptomics and urine metabolomics for breast cancer biomarker identification. Bioinformatics 2009; 25: 3151–7. [DOI] [PubMed] [Google Scholar]
- 141.Cho SH, Jung BH, Lee SH, Lee WY, Kong G, Chung BC. Direct determination of nucleosides in the urine of patients with breast cancer using column-switching liquid chromatography-tandem mass spectrometry. Biomed Chromatogr 2006; 20: 1229–36. [DOI] [PubMed] [Google Scholar]
- 142.Hsu WY, Lin WD, Tsai Y, Lin CT, Wang HC, Jeng LB, Lee CC, Lin YC, Lai CC, Tsai FJ. Analysis of urinary nucleosides as potential tumor markers in human breast cancer by high performance liquid chromatography/electrospray ionization tandem mass spectrometry. Clin Chim Acta 2011; 412: 1861–6. [DOI] [PubMed] [Google Scholar]
- 143.Byun JA, Lee SH, Jung BH, Choi MH, Moon MH, Chung BC. Analysis of polyamines as carbamoyl derivatives in urine and serum by liquid chromatography-tandem mass spectrometry. Biomed Chromatogr 2008; 22: 73–80. [DOI] [PubMed] [Google Scholar]
- 144.Feng C, Wu Z, Guo T, Jiang H, Guan M, Zhang Y, Wen H, Ding Q. BLCA-4 expression is related to MMP-9, VEGF, IL-1alpha and IL-8 in bladder cancer but not to PEDF, TNF-alpha or angiogenesis. Pathol Biol 2012; 60: e36–40. [DOI] [PubMed] [Google Scholar]
- 145.Lee HL, Eom HS, Yun T, Kim HJ, Park WS, Nam BH, Moon-Woo S, Lee DH, Kong SY. Serum and urine levels of interleukin-8 in patients with non-Hodgkin’s lymphoma. Cytokine 2008; 43: 71–5. [DOI] [PubMed] [Google Scholar]
- 146.Fujita K, Ewing CM, Isaacs WB, Pavlovich CP. Immunomodulatory IL-18 binding protein is produced by prostate cancer cells and its levels in urine and serum correlate with tumor status. Int J Cancer 2011; 129: 424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Korzeniewski N, Tosev G, Pahernik S, Hadaschik B, Hohenfellner M, Duensing S. Identification of cell-free microRNAs in the urine of patients with prostate cancer. Urol Oncol 2015; 33: 16 e7–22. [DOI] [PubMed] [Google Scholar]
- 148.Som A, Tu SM, Liu J, Wang X, Qiao W, Logothetis C, Corn PG. Response in bone turnover markers during therapy predicts overall survival in patients with metastatic prostate cancer: analysis of three clinical trials. Br J Cancer 2012; 107: 1547–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Sapre N, Hong MK, Macintyre G, Lewis H, Kowalczyk A, Costello AJ, Corcoran NM, Hovens CM. Curated microRNAs in urine and blood fail to validate as predictive biomarkers for high-risk prostate cancer. PloS One 2014; 9: e91729–e91729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Park SL, Carmella SG, Ming X, Vielguth E, Stram DO, Le Marchand L, Hecht SS. Variation in levels of the lung carcinogen NNAL and its glucuronides in the urine of cigarette smokers from five ethnic groups with differing risks for lung cancer. Cancer Epidemiol Biomarkers Prev 2015; 24: 561–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Liu BC, Zhang L, Lv LL, Wang YL, Liu DG, Zhang XL. Application of antibody array technology in the analysis of urinary cytokine profiles in patients with chronic kidney disease. Am J Nephrol 2006; 26: 483–90. [DOI] [PubMed] [Google Scholar]
- 152.Ni J, Huang HQ, Lu LL, Zheng M, Liu BC. Influence of irbesartan on the urinary excretion of cytokines in patients with chronic kidney disease. Chin Med J 2012; 125: 1147–52. [PubMed] [Google Scholar]
- 153.Idasiak-Piechocka I, Oko A, Pawliczak E, Kaczmarek E, Czekalski S. Urinary excretion of soluble tumour necrosis factor receptor 1 as a marker of increased risk of progressive kidney function deterioration in patients with primary chronic glomerulonephritis. Nephrol Dial Transplant 2010; 25: 3948–56. [DOI] [PubMed] [Google Scholar]
- 154.Suen JL, Liu CC, Lin YS, Tsai YF, Juo SH, Chou YH. Urinary chemokines/cytokines are elevated in patients with urolithiasis. Urol Res 2010; 38: 81–7. [DOI] [PubMed] [Google Scholar]
- 155.Nassirpour R, Mathur S, Gosink MM, Li Y, Shoieb AM, Wood J, O’Neil SP, Homer BL, Whiteley LO. Identification of tubular injury microRNA biomarkers in urine: comparison of next-generation sequencing and qPCR-based profiling platforms. BMC Genomics 2014; 15: 485–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Huybrechts B, Martins JC, Debongnie P, Uhlig S, Callebaut A. Fast and sensitive LC-MS/MS method measuring human mycotoxin exposure using biomarkers in urine. Arch Toxicol 2015; 89: 1993–2005. [DOI] [PubMed] [Google Scholar]
- 157.Sereno J, Nunes S, Rodrigues-Santos P, Vala H, Rocha-Pereira P, Fernandes J, Santos-Silva A, Teixeira F, Reis F. Conversion to sirolimus ameliorates cyclosporine-induced nephropathy in the rat: focus on serum, urine, gene, and protein renal expression biomarkers. BioMed Res Int 2014; 2014: 576929–576929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Liu D, Huang P, Li X, Ge M, Luo G, Hei Z. Using inflammatory and oxidative biomarkers in urine to predict early acute kidney injury in patients undergoing liver transplantation. Biomarkers 2014; 19: 424–9. [DOI] [PubMed] [Google Scholar]
- 159.Gu L, Wang X, Zhang Y, Jiang Y, Lu H, Bi K, Chen X. Determination of 12 potential nephrotoxicity biomarkers in rat serum and urine by liquid chromatography with mass spectrometry and its application to renal failure induced by Semen Strychni. J Separation Sci 2014; 37: 1058–66. [DOI] [PubMed] [Google Scholar]
- 160.Stubendorff B, Finke S, Walter M, Kniemeyer O, von Eggeling F, Gruschwitz T, Steiner T, Ott U, Wolf G, Wunderlich H, Junker K. Urine protein profiling identified alpha-1-microglobulin and haptoglobin as biomarkers for early diagnosis of acute allograft rejection following kidney transplantation. World J Urol 2014; 32: 1619–24. [DOI] [PubMed] [Google Scholar]
- 161.Parikh CR, Dahl NK, Chapman AB, Bost JE, Edelstein CL, Comer DM, eltner R, Tian X, Grantham JJ, Somlo S. Evaluation of urine biomarkers of kidney injury in polycystic kidney disease. Kidney Int 2012; 81: 784–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Meijer E, Boertien WE, Nauta FL, Bakker SJ, van Oeveren W, Rook M, van der Jagt EJ, van Goor H, Peters DJ, Navis G, de Jong PE, Gansevoort RT. Association of urinary biomarkers with disease severity in patients with autosomal dominant polycystic kidney disease: a cross-sectional analysis. Am J Kidney Dis 2010; 56: 883–95. [DOI] [PubMed] [Google Scholar]
- 163.Wasilewska A, Zoch-Zwierz W, Taranta-Janusz K, Kolodziejczyk Z. Urinary monocyte chemoattractant protein-1 excretion in children with glomerular proteinuria. Scand J Urol Nephrol 2011; 45: 52–9. [DOI] [PubMed] [Google Scholar]
- 164.Sola-Del Valle DA, Mohan S, Cheng JT, Paragas NA, Sise ME, D’Agati VD, Barasch J. Urinary NGAL is a useful clinical biomarker of HIV-associated nephropathy. Nephrol Dial Transplant 2011; 26: 2387–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Torres ME, Goncalves LL, Bronze MR, Santos AP, Batoreu MC, Mateus ML. Alternative biomarkers of n-hexane exposure: characterization of aminoderived pyrroles and thiol-pyrrole conjugates in urine of rats exposed to 2,5-hexanedione. Toxicol Lett 2014; 224: 54–63. [PubMed] [Google Scholar]
- 166.Ghanbari H, Ghanbari K, Beheshti I, Munzar M, Vasauskas A, Averback P. Biochemical assay for AD7C-NTP in urine as an Alzheimer’s disease marker. J Clin Lab Analy 1998; 12: 285–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang C, Cui Y, Yang J, Zhang J, Yuan D, Wei Y, Li Y, Duo Y, Li S, Zhu W, Zheng L. Combining serum and urine biomarkers in the early diagnosis of mild cognitive impairment that evolves into Alzheimer’s disease in patients with the apolipoprotein E 4 genotype. Biomarkers 2015; 20: 84–8. [DOI] [PubMed] [Google Scholar]
- 168.Fukuhara K, Ohno A, Ota Y, Senoo Y, Maekawa K, Okuda H, Kurihara M, Okuno A, Niida S, Saito Y, Takikawa O. NMR-based metabolomics of urine in a mouse model of Alzheimer’s disease: identification of oxidative stress biomarkers. J Clin Biochem Nutr 2013; 52: 133–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zhang C, Nestorova G, Rissman RA, Feng J. Detection and quantification of 8-hydroxy-2’-deoxyguanosine in Alzheimer’s transgenic mouse urine using capillary electrophoresis. Electrophoresis 2013; 34: 2268–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Takata M, Nakashima M, Takehara T, Baba H, Machida K, Akitake Y, Ono K, Hosokawa M, Takahashi M. Detection of amyloid beta protein in the urine of Alzheimer’s disease patients and healthy individuals. Neurosci Lett 2008; 435: 126–30. [DOI] [PubMed] [Google Scholar]
- 171.Kim KM, Jung BH, Paeng KJ, Kim I, Chung BC. Increased urinary F(2)-isoprostanes levels in the patients with Alzheimer’s disease. Brain Res Bull 2004; 64: 47–51. [DOI] [PubMed] [Google Scholar]
- 172.Connolly J, Siderowf A, Clark CM, Mu D, Pratico D. F2 isoprostane levels in plasma and urine do not support increased lipid peroxidation in cognitively impaired Parkinson disease patients. Cogn Behav Neurol 2008; 21: 83–6. [DOI] [PubMed] [Google Scholar]
- 173.Nichkova M, Wynveen PM, Marc DT, Huisman H, Kellermann GH. Validation of an ELISA for urinary dopamine: applications in monitoring treatment of dopamine-related disorders. J Neurochem 2013; 125: 724–35. [DOI] [PubMed] [Google Scholar]
- 174.Bolner A, Pilleri M, De Riva V, Nordera GP. Plasma and urinary HPLC-ED determination of the ratio of 8-OHdG/2-dG in Parkinson’s disease. Clin Lab 2011; 57: 859–66. [PubMed] [Google Scholar]
- 175.Lee CY, Seet RC, Huang SH, Long LH, Halliwell B. Different patterns of oxidized lipid products in plasma and urine of dengue fever, stroke, and Parkinson’s disease patients: cautions in the use of biomarkers of oxidative stress. Antioxid Redox Signal 2009; 11: 407–20. [DOI] [PubMed] [Google Scholar]
- 176.Barbado J, Martin D, Vega L, Almansa R, Goncalves L, Nocito M, Jimeno A, Ortiz de Lejarazu R, Bermejo-Martin JF. MCP-1 in urine as biomarker of disease activity in systemic lupus erythematosus. Cytokine 2012; 60: 583–6. [DOI] [PubMed] [Google Scholar]
- 177.Yang CC, Hsieh SC, Li KJ, Wu CH, Lu MC, Tsai CY, Yu CL. Urinary neutrophil gelatinase-associated lipocalin is a potential biomarker for renal damage in patients with systemic lupus erythematosus. J Biomed Biotechnol 2012; 2012: 759313–759313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Jung K, Lein M. Bone turnover markers in serum and urine as diagnostic, prognostic and monitoring biomarkers of bone metastasis. Biochim Biophys Acta 2014; 1846: 425–38. [DOI] [PubMed] [Google Scholar]
- 179.Garnero P, Buchs N, Zekri J, Rizzoli R, Coleman RE, Delmas PD. Markers of bone turnover for the management of patients with bone metastases from prostate cancer. Br J Cancer 2000; 82: 858–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Tavintharan S, Pek LT, Liu JJ, Ng XW, Yeoh LY, Su Chi L, Chee Fang S. Osteoprotegerin is independently associated with metabolic syndrome and microvascular complications in type 2 diabetes mellitus. Diabetes Vasc Dis Res 2014; 11: 359–62. [DOI] [PubMed] [Google Scholar]
- 181.Oh KW, Rhee EJ, Lee WY, Kim SW, Oh ES, Baek KH, Kang MI, Choi MG, Yoo HJ, Park SW. The relationship between circulating osteoprotegerin levels and bone mineral metabolism in healthy women. Clin Endocrinol 2004; 61: 244–9. [DOI] [PubMed] [Google Scholar]
- 182.Watanabe T, Suzuya H, Onishi T, Kanai S, Kaneko M, Watanabe H, Nakagawa R, Kawano Y, Takaue Y, Kuroda Y, Talmadge JE. Effect of granulocyte colony-stimulating factor on bone metabolism during peripheral blood stem cell mobilization. Int J Hematol 2003; 77: 75–81. [DOI] [PubMed] [Google Scholar]
- 183.Mesa F, Magan-Fernandez A, Munoz R, Papay-Ramirez L, Poyatos R, Sanchez-Fernandez E, Galindo-Moreno P, Rodríguez-Barranco M. Catecholamine metabolites in urine, as chronic stress biomarkers, are associated with higher risk of chronic periodontitis in adults. J Periodontol 2014; 85: 1755–62. [DOI] [PubMed] [Google Scholar]
- 184.Slobodov G, Feloney M, Gran C, Kyker KD, Hurst RE, Culkin DJ. Abnormal expression of molecular markers for bladder impermeability and differentiation in the urothelium of patients with interstitial cystitis. J Urol 2004; 171: 1554–8. [DOI] [PubMed] [Google Scholar]
- 185.Keay S, Zhang CO, Kagen DI, Hise MK, Jacobs SC, Hebel JR, Gordon D, Whitmore K, Bodison S, Warren JW. Concentrations of specific epithelial growth factors in the urine of interstitial cystitis patients and controls. J Urol 1997; 158: 1983–8. [DOI] [PubMed] [Google Scholar]
- 186.Byrne DS, Sedor JF, Estojak J, Fitzpatrick KJ, Chiura AN, Mulholland SG. The urinary glycoprotein GP51 as a clinical marker for interstitial cystitis. J Urol 1999; 161: 1786–90. [DOI] [PubMed] [Google Scholar]
- 187.Zeng Y, Wu XX, Homma Y, Yoshimura N, Iwaki H, Kageyama S, Yoshiki T, Kakehi Y. Uroplakin III-delta4 messenger RNA as a promising marker to identify nonulcerative interstitial cystitis. J Urol 2007; 178: 1322–7; discussion 7. [DOI] [PubMed] [Google Scholar]
- 188.Hauser PJ, Dozmorov MG, Bane BL, Slobodov G, Culkin DJ, Hurst RE. Abnormal expression of differentiation related proteins and proteoglycan core proteins in the urothelium of patients with interstitial cystitis. J Urol 2008; 179: 764–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Saban R, Saban MR, Maier J, Fowler B, Tengowski M, Davis CA, Wu XR, Culkin DJ, Hauser P, Backer J, Hurst RE. Urothelial expression of neuropilins and VEGF receptors in control and interstitial cystitis patients. Am J Physiol Ren Physiol 2008; 295: F1613–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lotz M, Villiger P, Hugli T, Koziol J, Zuraw BL. Interleukin-6 and interstitial cystitis. J Urol 1994; 152: 869–73. [DOI] [PubMed] [Google Scholar]
- 191.Jacobs BL, Smaldone MC, Tyagi V, Philips BJ, Jackman SV, Leng WW, Tyagi P. Increased nerve growth factor in neurogenic overactive bladder and interstitial cystitis patients. Can J Urol 2010; 17: 4989–94. [PubMed] [Google Scholar]
- 192.Keay SK, Zhang CO, Shoenfelt J, Erickson DR, Whitmore K, Warren JW, Marvel R, Chai T. Sensitivity and specificity of antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor as urine markers for interstitial cystitis. Urology 2001; 57: 9–14. [DOI] [PubMed] [Google Scholar]
- 193.Young BL, Mlamla Z, Gqamana PP, Smit S, Roberts T, Peter J, Theron G, Govender U, Dheda K, Blackburn J. The identification of tuberculosis biomarkers in human urine samples. Eur Respir J 2014; 43: 1719–29. [DOI] [PubMed] [Google Scholar]
- 194.Wong SY, Cabodi M, Rolland J, Klapperich CM. Evaporative concentration on a paper-based device to concentrate analytes in a biological fluid. Anal Chem 2014; 86: 11981–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Fortun J, Martin-Davila P, Gomez-Mampaso E, Gonzalez-Garcia A, Barbolla I, Gomez-Garcia I, Wikman P, Ortíz J, Navas E, Cuartero C, Gijón D, Moreno S. Extra-pulmonary tuberculosis: differential aspects and role of 16S-rRNA in urine. Int J Tuberc Lung Dis 2014; 18: 478–85. [DOI] [PubMed] [Google Scholar]
- 196.Pollock NR, Macovei L, Kanunfre K, Dhiman R, Restrepo BI, Zarate I, Pino PA, Mora-Guzman F, Fujiwara RT, Michel G, Kashino SS, Campos-Neto A. Validation of Mycobacterium tuberculosis Rv1681 protein as a diagnostic marker of active pulmonary tuberculosis. J Clin Microbiol 2013; 51: 1367–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Shi J, Wang Z, Li H, Yuan H. Diagnostic performance of the urinary deoxypyridinoline in spinal tuberculosis. Orthopedics 2012; 35: e922–6. [DOI] [PubMed] [Google Scholar]
- 198.Cannas A, Calvo L, Chiacchio T, Cuzzi G, Vanini V, Lauria FN, Pucci L, Girardi E, Goletti D. IP-10 detection in urine is associated with lung diseases. BMC Infect Dis 2010; 10: 333–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Horak E, Gassner I, Solder B, Wachter H, Fuchs D. Neopterin levels and pulmonary tuberculosis in infants. Lung 1998; 176: 337–44. [DOI] [PubMed] [Google Scholar]
- 200.Sofia M, Mormile M, Faraone S, Alifano M, Carratu P, Carratu L. Endothelin-1 excretion in urine in active pulmonary sarcoidosis and in other interstitial lung diseases. Sarcoidosis 1995; 12: 118–23. [PubMed] [Google Scholar]
- 201.Liu KD, Yang W, Go AS, Anderson AH, Feldman HI, Fischer MJ, He J, Kallem RR, Kusek JW, Master SR, Miller ER, 3rd, Rosas SE, Steigerwalt S, Tao K, Weir MR, Hsu CY. CRIC Study Investigators. Urine neutrophil gelatinase-associated lipocalin and risk of cardiovascular disease and death in CKD: results from the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 2015; 65: 267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Palomino HL, Rifkin DE, Anderson C, Criqui MH, Whooley MA, Ix JH. 24-hour urine phosphorus excretion and mortality and cardiovascular events. Clin J Am Soc Nephrol 2013; 8: 1202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Carter CE, Gansevoort RT, Scheven L, Heerspink HJ, Shlipak MG, de Jong PE, Ix JH. Influence of urine creatinine on the relationship between the albumin-to-creatinine ratio and cardiovascular events. Clin J Am Soc Nephrol 2012; 7: 595–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Tofik R, Torffvit O, Rippe B, Bakoush O. Increased urine IgM excretion predicts cardiovascular events in patients with type 1 diabetes nephropathy. BMC Med 2009; 7: 39–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Christiansen MS, Hommel E, Magid E, Feldt-Rasmussen B. Orosomucoid in urine is a powerful predictor of cardiovascular mortality in normoalbuminuric patients with type 2 diabetes at five years of follow-up. Diabetologia 2005; 48: 386–93. [DOI] [PubMed] [Google Scholar]
- 206.Osaki M, Kosaka N, Okada F, Ochiya T. Circulating microRNAs in drug safety assessment for hepatic and cardiovascular toxicity: the latest biomarker frontier? Mol Diagn Ther 2014; 18: 121–6. [DOI] [PubMed] [Google Scholar]
- 207.Bracha S, McNamara M, Hilgart I, Milovancev M, Medlock J, Goodall C, Wickramasekara S, Maier CS. A multiplex biomarker approach for the diagnosis of transitional cell carcinoma from canine urine. Anal Biochem 2014; 455: 41–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Cheng D, Liang B, Li Y. Clinical value of vascular endothelial growth factor and endostatin in urine for diagnosis of bladder cancer. Tumori 2012; 98: 762–7. [DOI] [PubMed] [Google Scholar]
- 209.Da Pieve C, Sahgal N, Moore SA, Velasco-Garcia MN. Development of a liquid chromatography/tandem mass spectrometry method to investigate the presence of biomarkers of DNA damage in urine related to red meat consumption and risk of colorectal cancer. Rapid Commun Mass Spectrom 2013; 27: 2493–503. [DOI] [PubMed] [Google Scholar]
- 210.Barocas DA, Motley S, Cookson MS, Chang SS, Penson DF, Dai Q, Milne G, Roberts LJ, 2nd, Morrow J, Concepcion RS, Smith JA, Jr, Fowke JH. Oxidative stress measured by urine F2-isoprostane level is associated with prostate cancer. J Urol 2011; 185: 2102–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Lafuente A, Rodriguez A, Gibanel R, Lafuente MJ, Alonso M, Molina R, Ballesta A, Carretero P. Limitations in the use of glutathione S-transferase P1 in urine as a marker for bladder cancer. Anticancer Res 1998; 18: 3771–2. [PubMed] [Google Scholar]
- 212.Wright ME, Michaud DS, Pietinen P, Taylor PR, Virtamo J, Albanes D. Estimated urine pH and bladder cancer risk in a cohort of male smokers (Finland). Cancer Causes Control 2005; 16: 1117–23. [DOI] [PubMed] [Google Scholar]
- 213.Henning SM, Wang P, Abgaryan N, Vicinanza R, de Oliveira DM, Zhang Y, Lee RP, Carpenter CL, Aronson WJ, Heber D. Phenolic acid concentrations in plasma and urine from men consuming green or black tea and potential chemopreventive properties for colon cancer. Mol Nutr Food Res 2013; 57: 483–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Turner GA, Ellis RD, Guthrie D, Latner AL, Monaghan JM, Ross WM, Skillen AW, Wilson RG. Urine cyclic nucleotide concentrations in cancer and other conditions; cyclic GMP: a potential marker for cancer treatment. J Clin Pathol 1982; 35: 800–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.De Jong WH, De Boer EC, Van der Meijden AP, Vegt P, Steerenberg PA, Debruyne FM, Ruitenberg EJ. Presence of interleukin-2 in urine of superficial bladder cancer patients after intravesical treatment with bacillus Calmette-Guerin. Cancer Immunol Immunother 1990; 31: 182–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.de Boer EC, de Jong WH, van der Meijden AP, Steerenberg PA, Witjes F, Vegt PD, Debruyne FM, Ruitenberg EJ. Leukocytes in the urine after intravesical BCG treatment for superficial bladder cancer. A flow cytofluorometric analysis. Urol Res 1991; 19: 45–50. [DOI] [PubMed] [Google Scholar]
- 217.Benedict WF, Fisher M, Zhang XQ, Yang Z, Munsell MF, Dinney CN. Use of monitoring levels of soluble forms of cytokeratin 18 in the urine of patients with superficial bladder cancer following intravesical Ad-IFNalpha/Syn3 treatment in a phase l study. Cancer Gene Ther 2014; 21: 91–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Ma L, Chen J, Wang R, Han Y, Zhang J, Dong W, Zhang X, Wu Y, Zhao Z. The level of Alzheimer-associated neuronal thread protein in urine may be an important biomarker of mild cognitive impairment. J Clin Neurosci 2015; 22: 649–52. [DOI] [PubMed] [Google Scholar]
- 219.Libert F, Coudore F, Richard D, Durif F, Eschalier A. Development of a gas chromatographic/mass spectrometric method to quantify R(-)-apomorphine, R(-)-apocodeine and R(-)-norapomorphine in human plasma and urine. J Mass Spectrom 2005; 40: 1521–5. [DOI] [PubMed] [Google Scholar]
- 220.Andrew R, Watson DG, Best SA, Midgley JM, Wenlong H, Petty RK. The determination of hydroxydopamines and other trace amines in the urine of parkinsonian patients and normal controls. Neurochem Res 1993; 18: 1175–7. [DOI] [PubMed] [Google Scholar]
- 221.Golasik M, Wodowski G, Gomolka E, Herman M, Piekoszewski W. Urine as a material for evaluation of exposure to manganese in methcathinone users. J Trace Elem Med Biol 2014; 28: 338–43. [DOI] [PubMed] [Google Scholar]
- 222.Bispo JA, de Sousa Vieira EE, Silveira L, Jr, Fernandes AB. Correlating the amount of urea, creatinine, and glucose in urine from patients with diabetes mellitus and hypertension with the risk of developing renal lesions by means of Raman spectroscopy and principal component analysis. J Biomed Opt 2013; 18: 87004–87004. [DOI] [PubMed] [Google Scholar]
- 223.Yang Y, Xiao L, Li J, Kanwar YS, Liu F, Sun L. Urine miRNAs: potential biomarkers for monitoring progression of early stages of diabetic nephropathy. Med Hypotheses 2013; 81: 274–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Bhensdadia NM, Hunt KJ, Lopes-Virella MF, Michael Tucker J, Mataria MR, Alge JL, Neely BA, Janech MG, Arthur JM. Veterans Affairs Diabetes Trial (VADT) study group. Urine haptoglobin levels predict early renal functional decline in patients with type 2 diabetes. Kidney Int 2013; 83: 1136–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Sawanyawisuth K, Limpawattana P, Mahankkanukrauh A, Wongvipaporn C. The rate of checking urine microalbumin and aspirin primary prevention in type 2 DM. J Med Assoc Thai 2006; 89: 626–31. [PubMed] [Google Scholar]
- 226.Schroeder A, Heiderhoff M, Kobberling J. Determination of albuminuria in the urine of diabetics for prevention and control of diabetic nephropathy. GMS Health Technol Assess 2005; 1: Doc04–Doc04. [PMC free article] [PubMed] [Google Scholar]
- 227.Oxlund CS, Buhl KB, Jacobsen IA, Hansen MR, Gram J, Henriksen JE, Schousboe K, Tarnow L, Jensen BL. Amiloride lowers blood pressure and attenuates urine plasminogen activation in patients with treatment-resistant hypertension. J Am Soc Hypertens 2014; 8: 872–81. [DOI] [PubMed] [Google Scholar]
- 228.Matsa R, Ashley E, Sharma V, Walden AP, Keating L. Plasma and urine neutrophil gelatinase-associated lipocalin in the diagnosis of new onset acute kidney injury in critically ill patients. Crit Care 2014; 18: R137–R137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ka SM, Tsai PY, Chao TK, Yang SM, Hung YJ, Chen JS, Shui HA, Chen A. Urine annexin A1 as an index for glomerular injury in patients. Dis Markers 2014; 2014: 854163–854163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Piscator M. The nephropathy of chronic cadmium poisoning. In: Foulkes EC. (ed). Cadmium, New York, NY: Springer-Verlag, 1986, pp. 179–94. [Google Scholar]
- 231.Thuijls G, Derikx JP, de Haan JJ, Grootjans J, de Bruine A, Masclee AA, Heineman E, Buurman WA. Urine-based detection of intestinal tight junction loss. J Clin Gastroenterol 2010; 44: e14–9. [DOI] [PubMed] [Google Scholar]
- 232.Wang L, Liu HY, Shi HH, Lang JH, Sun W. Urine peptide patterns for non-invasive diagnosis of endometriosis: a preliminary prospective study. Eur J Obstet Gynecol Reprod Biol 2014; 177: 23–8. [DOI] [PubMed] [Google Scholar]
- 233.Sylvester KG, Ling XB, Liu GY, Kastenberg ZJ, Ji J, Hu Z, Wu S, Peng S, Abdullah F, Brandt ML, Ehrenkranz RA, Harris MC, Lee TC, Simpson BJ, Bowers C, Moss RL. Urine protein biomarkers for the diagnosis and prognosis of necrotizing enterocolitis in infants. J Pediatr 2014; 164: 607–12 e1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Kimmel DW, LeBlanc G, Meschievitz ME, Cliffel DE. Electrochemical sensors and biosensors. Anal Chem 2012; 84: 685–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Chen A, Chatterjee S. Nanomaterials based electrochemical sensors for biomedical applications. Chem Soc Rev 2013; 42: 5425–38. [DOI] [PubMed] [Google Scholar]
- 236.Gorodkiewicz E, Guszcz T, Roszkowska-Jakimiec W, Kozlowski R. Cathepsin D serum and urine concentration in superficial and invasive transitional bladder cancer as determined by surface plasmon resonance imaging. Oncol Lett 2014; 8: 1323–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Khalid T, White P, De Lacy Costello B, Persad R, Ewen R, Johnson E, Probert CS, Ratcliffe N. A pilot study combining a GC-sensor device with a statistical model for the identification of bladder cancer from urine headspace. PloS One 2013; 8: e69602–e69602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Huang J, Kumar S, Abbassi-Ghadi N, Spanel P, Smith D, Hanna GB. Selected ion flow tube mass spectrometry analysis of volatile metabolites in urine headspace for the profiling of gastro-esophageal cancer. Anal Chem 2013; 85: 3409–16. [DOI] [PubMed] [Google Scholar]
- 239.Jager T, Tschirdewahn S, Vom Dorp F, Piechotta G, Rubben H, Szarvas T. [Siliconchiptechnology-based MMP-7 analysis in urine: an option for preoperative identification of lymph node metastasis in bladder cancer]. Der Urologe Ausg A 2013; 52: 853–8. [DOI] [PubMed] [Google Scholar]
- 240.Mohan K, Donavan KC, Arter JA, Penner RM, Weiss GA. Sub-nanomolar detection of prostate-specific membrane antigen in synthetic urine by synergistic, dual-ligand phage. J Am Chem Soc 2013; 135: 7761–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Boyle JO, Mao L, Brennan JA, Koch WM, Eisele DW, Saunders JR, Sidransky D. Gene mutations in saliva as molecular markers for head and neck squamous cell carcinomas. Am J Surg 1994; 168: 429–32. [DOI] [PubMed] [Google Scholar]
- 242.Wei F, Lin CC, Joon A, Feng Z, Troche G, Lira ME, Chia D, Mao M, Ho CL, Su WC, Wong DT. Noninvasive saliva-based EGFR gene mutation detection in patients with lung cancer. Am J Respir Crit Care Med 2014; 190: 1117–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Yang CY, Brooks E, Li Y, Denny P, Ho CM, Qi F, Shi W, Wolinsky L, Wu B, Wong DT, Montemagno CD. Detection of picomolar levels of interleukin-8 in human saliva by SPR. Lab Chip 2005; 5: 1017–23. [DOI] [PubMed] [Google Scholar]
- 244.Tan W, Sabet L, Li Y, Yu T, Klokkevold PR, Wong DT, Ho CM. Optical protein sensor for detecting cancer markers in saliva. Biosens Bioelectron 2008; 24: 266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Jokerst JV, Raamanathan A, Christodoulides N, Floriano PN, Pollard AA, Simmons GW, Wong J, Gage C, Furmaga WB, Redding SW, McDevitt JT. Nano-bio-chips for high performance multiplexed protein detection: determinations of cancer biomarkers in serum and saliva using quantum dot bioconjugate labels. Biosens Bioelectron 2009; 24: 3622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]