Abstract
Adrenal infarction is a very rare event but occasionally seen in hypercoagulable states. We present a case of a 31-year-old woman at 38 weeks of gestation who developed a severe upper abdominal pain and unilateral adrenal infarction due to thrombosis of the adrenal vein. The only thrombogenic factor found was pregnancy. The case highlights that adrenal infarction may complicate a normal pregnancy and should be included in the differential diagnosis of the acute abdomen in pregnancy.
Keywords: Endocrinology, pregnancy, thrombophilia, adrenal infarction
Case report
A 31-year-old G2P1 contacted her local hospital at 38 weeks of gestation with new onset right upper abdominal pain. Her previous pregnancy had been uneventful and her family history was negative for thromboembolic diseases. Obstetric ultrasound reported a single live fetus. Her blood pressure was normal (125/70 mm Hg) but she had moderate (++) proteinuria on a urine dipstick. Her full blood count, serum C-reactive protein (CRP), electrolytes, creatinine, and alanine aminotransferase were all within normal limits. Her patellar reflexes were clonic and a preliminary diagnosis of pre-eclampsia was made. Abdominal pain was suspected to be a sign of liver distension due to preeclampsia. She was commenced on intravenous magnesium sulphate as an anticonvulsant agent. Her cervix was favourable for labour induction, hence artificial rupture of the membranes was performed. She went on to have a normal vaginal delivery and gave birth to a healthy male infant weighing 3415 g. The placenta was macroscopically normal weighing 535 g. Epidural analgesia during the labour provided complete abdominal pain relief.
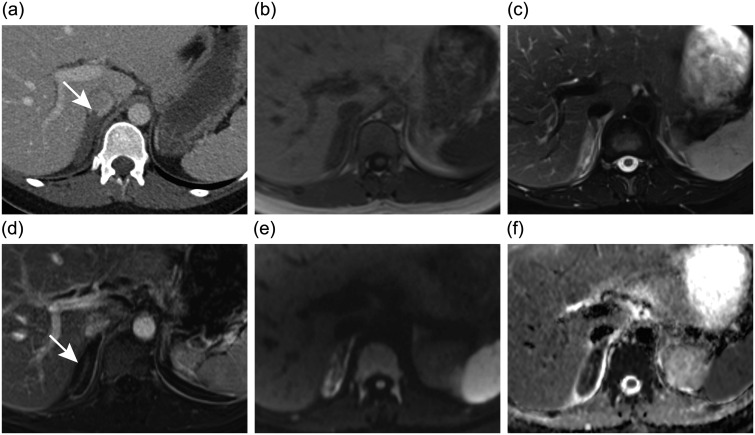
After the labour, the patient had no significant proteinuria in her 24-h urine collection and her blood pressure and reflexes were normal. When the effect of epidural analgesia had ceased, the severe pain reappeared and she again required opioids for pain relief. An abdominal contrast-enhanced computed tomography (CT) scan was obtained which revealed enlargement and oedema of the right adrenal gland (Figure 1a). A small thrombus adjacent to the right adrenal gland in the inferior vena cava was detected. To ascertain the diagnosis, magnetic resonance image (MRI) was obtained the next day (Figure 1b–f). Right adrenal infarction with thrombosis of the adrenal vein was confirmed. There was no evidence of haemorrhage in the gland.
Figure 1.
Axial images at the level of the right adrenal gland. (a) Contrast-enhanced computed tomography image shows enlarged right adrenal gland and mild inflammatory changes in the adjacent fat. The tail of the adrenal vein thrombus (arrow) extending into the inferior vena cava can be seen. (b) T1-weighted magnetic resonance (MR) image shows no sign of adrenal haemorrhage. (c) T2-weighted fat-saturated MR image shows oedema of the right adrenal gland and adjacent fat. The adrenal vein thrombus is also seen. (d) Contrast-enhanced T1-weighted subtraction MR image shows capsular but no parenchymal enhancement of the right adrenal gland (arrow). (e and f) Diffusion-weighted MR imaging and the corresponding apparent diffusion coefficient map demonstrate restricted diffusion of the right adrenal gland consistent with infarction.
The patient developed no signs of adrenal insufficiency. Her serum cortisol was slightly increased to 747 nmol/L (non-pregnant reference range 150–650) on the first day postpartum and 805 on the sixth day but two weeks later within the normal non-pregnant range. Plasma adrenocorticotropic hormone, aldosterone, renin activity, dehydroepiandrosterone sulphate, metanephrine and normetanephrine levels were within normal range. CRP peaked at 183 mg/L, but leucocyte count was normal and the patient had no fever. No antibiotics were administered and CRP decreased spontaneously. Anticoagulation with low-molecular-weight heparin (LMWH), enoxaparin 60 mg subcutaneously twice a day, was initiated to prevent possible further venous thrombosis. The patient was discharged six days after the delivery. The pain subsided entirely in two weeks. Further testing which included factor V Leiden and prothrombin mutation and acquired thrombophilias such as antiphospholipid panel, protein C, protein S, antithrombin III and factor VIII activity revealed no thrombophilias. Plasma homocysteine level was normal excluding clinically significant methylenetetrahydrofolate reductase (MTHFR) gene mutation. LMWH was continued three months after the delivery and aspirin 100 mg × 1 recommended for 1–2 years.
The adrenal glands were imaged with MRI one month and three months later. After one month the thrombosis and oedema had disappeared and three months later atrophy of the entire right adrenal gland was seen.
One year after the infarction the patient was feeling well, had not developed any new thrombotic events and thrombophilia tests including antiphospholipid panel were still negative.
Discussion
Although adrenal infarction is a rare event, it is occasionally seen in antiphospholipid syndrome and has also been described as the initial presentation of this syndrome.1–3 The majority of the published infarctions are bilateral.
The adrenal gland has a unique vasculature that makes it prone to infarction in hypercoagulable states. The arterial supply is rich but venous drainage limited with a single vein, and the localization of the thrombi in the adrenal vein might result in local stasis of blood leading to oedema and necrosis of the gland.4 Adrenal infarction is often accompanied by haemorrhage in the gland, but cases without MRI-detectable haemorrhage have also been reported.1,3,5 However, thrombosis of the adrenal vein seems to be the primary event also in the haemorrhagic infarctions.
Only one case of adrenal infarction in pregnancy has been published in English literature previously.5 The patient presented by Green et al. also had the infarction in the right adrenal gland with no associated haemorrhage. She had a heterozygous C677T mutation of the MTHFR gene as the only finding of thrombophilia; the clinical significance of this remains controversial.6
CT and MRI are considered the golden standard for imaging the adrenal. MRI is more sensitive in detecting the infarction and it may be used to assess the underlying haemorrhage in the adrenal glands if this is not apparent on the CT.1 In pregnancy MRI is the preferred imaging method.7
The need for therapeutic anticoagulation in adrenal infarction is obvious, but the risks need to be carefully considered in case of a haemorrhagic infarction and in the setting of pregnancy due to potential complications with regional anaesthesia and a risk of excessive bleeding during delivery.
Our patient avoided adrenal insufficiency secondary to the contralateral adrenal gland remaining unaffected. Her cortisol levels followed the normal postpartum pattern, with slightly increased levels that soon returned to normal.8 Our patient did not have pre-eclampsia. After the labour she had no proteinuria and we consider it possible that patellar reflexes were hyperactive due to a sudden release of adrenalin from the damaged gland.9 Since the afferent innervation of the adrenal gland originates from the level of T10 and below, an epidural analgesia giving a sensory block from T10 to L1 provided pain relief.
Our case highlights that adrenal infarction may complicate a normal pregnancy without any other recognized thrombophilic factor and should be included in the differential diagnosis of the acute abdomen in pregnancy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Written consent for publication was obtained from the patient.
Guarantor
EKL
Contributorship
All the authors were involved in managing the patient. HSH drafted the manuscript and all the authors reviewed and edited the manuscript and approved the final version.
References
- 1.Espinosa G, Santos E, Cervera R, et al. Adrenal involvement in the antiphospholipid syndrome: clinical and immunologic characteristics of 86 patients. Medicine 2003; 82: 106–118. [DOI] [PubMed] [Google Scholar]
- 2.Marie I, Levesque H, Heron F, et al. Acute adrenal failure secondary to bilateral infarction of the adrenal glands as the first manifestation of primary antiphospholipid antibody syndrome. Ann Rheum Dis 1997; 56: 567–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riddell AM, Khalili K. Sequential adrenal infarction without MRI-detectable hemorrhage in primary antiphospholipid-antibody syndrome. Am J Roentgenol 2004; 183: 220–222. [DOI] [PubMed] [Google Scholar]
- 4.Fox B. Venous infarction of the adrenal glands. J Pathol 1976; 119: 65–89. [DOI] [PubMed] [Google Scholar]
- 5.Green P-AD, Ngai IM, Lee TT, et al. Unilateral adrenal infarction in pregnancy. BMJ. Epub ahead of print 23 August 2013. DOI: 10.1136/bcr-2013-009997. [DOI] [PMC free article] [PubMed]
- 6.Ziakas PD, Poulou LS, Pavlou M, et al. Thrombophilia and venous thromboembolism in pregnancy: a meta-analysis of genetic risk. Eur J Obstet Gynecol Reprod Biol 2015; 6: 106–111. [DOI] [PubMed] [Google Scholar]
- 7.Masselli G, Derchi L, McHugo J, et al. Acute abdominal and pelvic pain in pregnancy: ESUR recommendations. Eur Radiol 2013; 23: 3485–3500. [DOI] [PubMed] [Google Scholar]
- 8.Jung C, Ho JT, Torpy DJ, et al. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab 2011; 96: 1533–1540. [DOI] [PubMed] [Google Scholar]
- 9.Tuttle WW. The effect of adrenalin upon the patellar tendon reflex. Am J Physiol 1924; 69: 446–454. [Google Scholar]