Abstract
Background
The purpose of the present study was to evaluate the results of the Sheffield bone block procedure for anteroinferior bone loss in traumatic shoulder instability. In this modified open technique, the medial half of coracoid process without its soft tissue attachments is used to provide congruent augmentation of the anteroinferior glenoid and secured with two screws.
Methods
In this retrospective consecutive case series (2007–11), all patients having recurrent traumatic instability with glenoid bone loss > 20% and/or a large Hill–Sachs lesion were included. The shoulder function was evaluated clinically and by Oxford Shoulder Instability Score (OSIS; by post/telephone).
Results
There were 84 patients in this series with a large proportion engaged in contact sports. Mean (range) age was 33 years (16 years to 45 years); male : female, 59 : 8; mean (range) follow-up period was 48 months (36 months to 84 months) and the response rate 89% (75/84). Mean postoperative OSIS was 43 (33 to 46) and one patient had re-dislocation (1.3%). No neurovascular complications/hardware failure/non-union/infections were noted. By 6 months, 85% patients had returned to pre-injury sport and 93% had returned to pre-injury work.
Conclusions
The Sheffield bone block procedure provides reliable and satisfactory results in patients having recurrent instability with glenoid bone loss and/or a large Hill–Sachs lesion with minimal complications and an excellent chance of returning to original sport and occupation.
Keywords: anteroinferior, glenoid bone loss, recurrent instability, shoulder
Introduction
Anteroinferior glenoid bone loss associated with recurrent traumatic anterior instability of the shoulder is significant and, if left unaddressed, can affect the outcome following surgical intervention. Clinically and biomechanically, there is good evidence in the literature to support non-anatomic bony transfers in the presence of significant anteroinferior glenoid bone deficieny, or risk factors such as young age, contact sports with high functional demands, and concomitant pathologies such as the Hill–Sachs lesion, for recurrent anterior shoulder instability.1–3 The recurrence rate is very high when only soft tissue reconstructions are performed in these situations.
In these situations, it becomes imperative to restore the ball and socket congruity of the glenohumeral joint for the stabilizing concavity-compression effect to occur.4 Under experimental conditions, the force required for dislocation is low with a Bankart repair in the presence of untreated glenoid bone loss.5,6
Various reconstruction techniques, such as Bristow, Latarjet and Eden–Hybinette procedures, as well as modifications of the Latarjet procedure, have been described in the literature to compensate for this glenoid defect. Latarjet described his shoulder stabilization technique of coracoid transfer in patients with glenoid bone defects.7
In this procedure, the horizontal limb of the coracoid process with the attached coracobrachialis tendon is transferred to the anteroinferior glenoid. Apart from the increase in anteroposterior diameter of the glenoid, Patte2 described the other two effects of this operation. This includes the posterior pull on the humeral head by the inferior third of the subscapularis when the arm is in abduction and external rotation. The other effect is caused by suturing of the coracoacromial ligament to the capsule, resulting in reconstruction of the anteroinferior capsular wall. In the Bristow procedure, only the tip of the coracoid process is transferred, whereas, in the Eden–Hybinette procedure, a free bone graft commonly from the iliac crest is used for this reconstruction. Some of the other modifications of the Latarjet described in the literature include the congruent arc Latarjet.
The literature suggests good results with these bony procedures with high satisfaction rates and low residual apprehension/recurrence rates.8–10 However, these procedures can be associated with complications such as improper positioning of the graft, hardware failure and distortion of local neurovascular structures.11
Materials and Methods
Aim
The purpose of the present study was to evaluate the outcome following the Sheffield bone block modification for antero-inferior bone loss in patients with recurrent traumatic anterior shoulder instability.
Inclusion criteria
Antero-inferior glenoid bone loss > 20% with or without large Hill–Sachs lesion [seen on computed tomography (CT) scan].
Revision following failed Bankart stabilization.
High-risk patients, such as patients who are involved in high-energy contact sports with any glenoid bone loss.
This was a retrospective consecutive case series of all patients from 2007–11 undergoing the Sheffield bone block procedure for anteroinferior glenoid bone loss in traumatic recurrent anterior shoulder instability. Patients were assessed based on history, clinical examination, plain radiographs and CT arthrogram. Glenoid ‘en-face’ views were utilized to assess the degree of antero-inferior glenoid bone loss. All of these cases performed at a single unit were independently reviewed by the first author (SV). The outcome was assessed clinically, through review of notes/X-rays and by Oxford Shoulder Instability Score (OSIS; by post/telephone).
Operative technique
In this open technique, the medial half of the coracoid is identified through the delto-pectoral interval. The conjoint tendon insertion is preserved and the pectoralis minor insertion is elevated subperiosteally from the coracoid (Fig. 1). The medial half of the coracoid is harvested as a free graft with a combination of saw and curved osteotomes (Fig. 2). The pectoralis minor tendon is reattached to the remnant lateral half of the coracoid with soft tissues. The coracoid graft is prepared in vitro on the table by removing all the soft tissues on it. It is rotated through 90° such that the under (inferior surface) of the coracoid becomes the articulating surface of the neoglenoid. Two holes are made in the original coracoid medial surface with K-wires after marking their location on the graft.
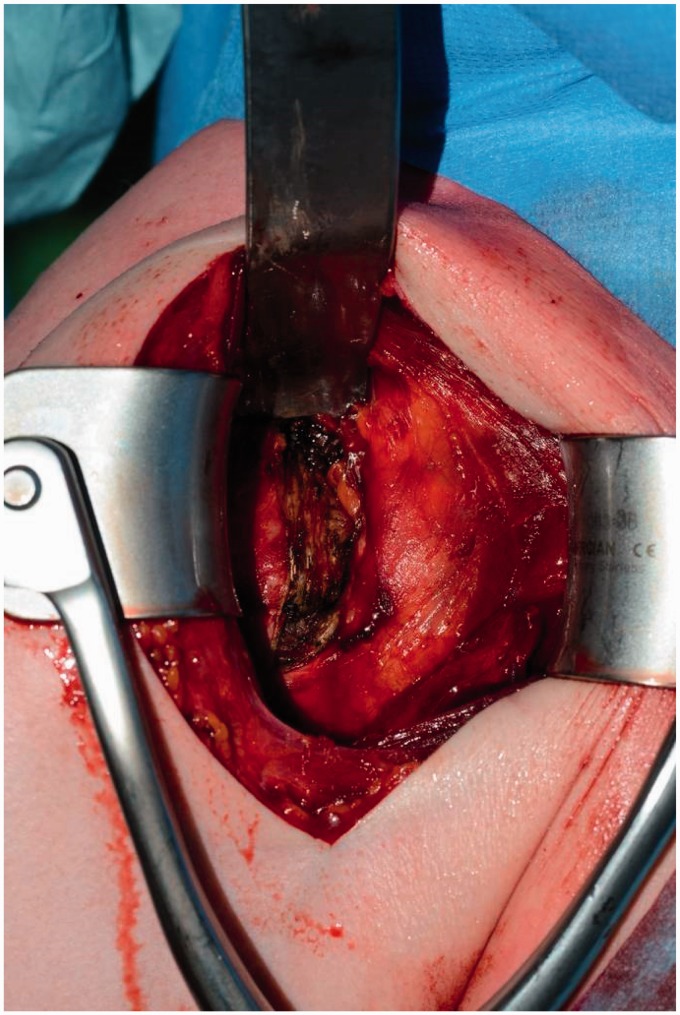
Figure 1.
Conjoint tendon is preserved and pectoralis minor tendon insertion is elevated subperiosteally.
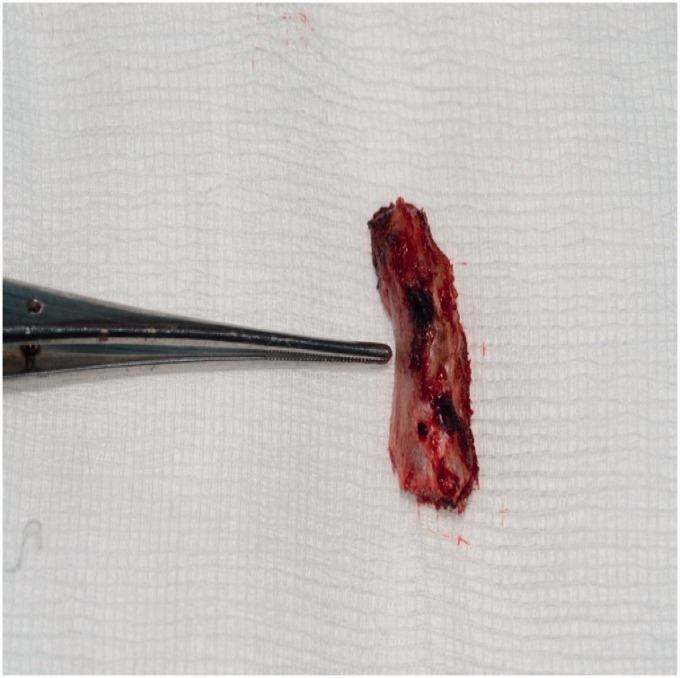
Figure 2.
Medial half of the coracoid is harvested as a free graft with markings for drilling holes in the graft.
A tenotomy is performed through the upper half of subscapularis along with the capsule as a single layer. The antero-inferior aspect of the glenoid is exposed. The capsule is released from this part of the glenoid and the surface of the bone is freshend with nibblers and a bone burr. The free graft is positioned on the glenoid with K-wires acting as joysticks. These holes are utilized to fix the graft to the glenoid with two fully threaded 4.5-mm cortical screws to achieve compression (Fig. 3). The graft is not overdrilled prior to insertion of the screws. The subscapularis tenotomy and capsule are closed over the graft without repair of the inferior capsule. In our technique, the free medial half of the coracoid remains intra-articular and provides congruent augmentation for the anteroinferior bone loss of the glenoid.
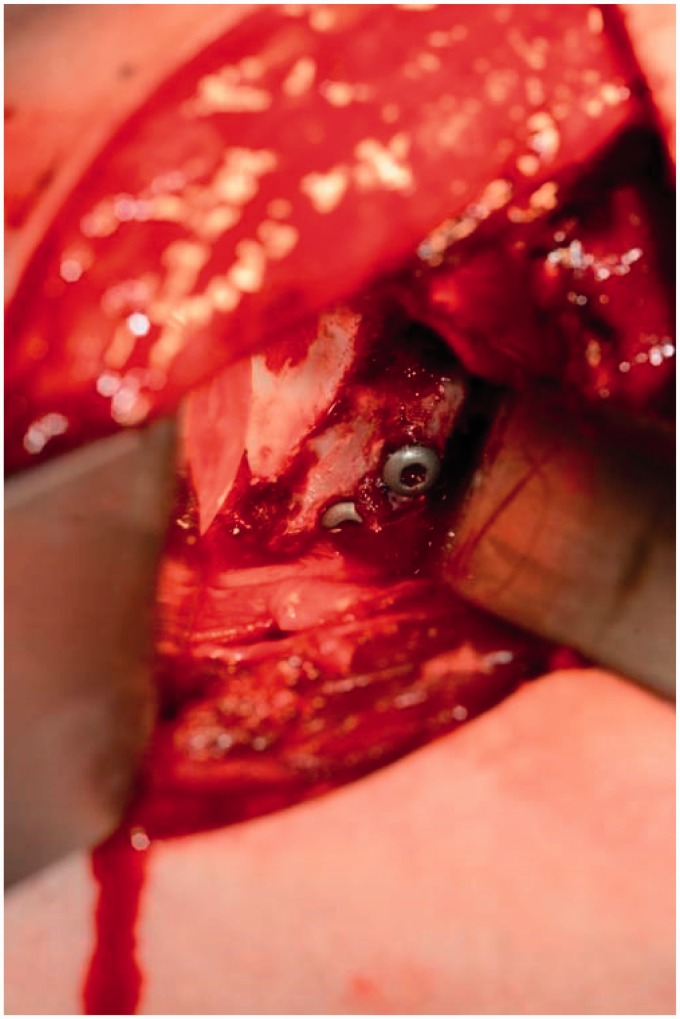
Figure 3.
The free coracoid graft is fixed to the anteroinferior glenoid with two screws.
Postoperatively, the patient follows a standard rehabilitation protocol. They are advised to refrain from contact sports for 4 months and heavy manual work for at least 3 months.
Results
Eighty-four patients fulfilled the inclusion criteria on review of notes. The age range was 16 years to 45 years (mean 33 years) with the majority of the patients being male (male : female, 59 : 8). The follow-up period varied between 36 months and 84 months (mean 48 months). Patients were assessed clinically and radiologically on X-rays during their last clinic visit regarding stability of the shoulder, range of movements, return to work, return to sports and graft healing/incorporation.
The OSIS response rate was 89% (75/84 patients responded to the postal/telephone questionnaire). The mean postoperative OSIS score was 43 (33 to 46) out a maximum score of 48. There were no metalware related complications such as protrusion into glenohumeral joint/failure of screws, neurovascular complications or deep infections. One patient had a superficial infection, which settled with antibiotics, and one patient had a re-dislocation (1.3%). Two patients required removal of metalware as a result of some discomfort in the front of the shoulder but they had no evidence of instability. These screws were removed arthroscopically with resolution of symptoms.
Specific enquiries were made to the patients about the nature of work, time duration to return to work, return to sports and the level/nature of sport in addition to their OSIS.
With regard to work, out of the 75 patients, three were unemployed at the time of the operation. Seventy-five percent (54/72 patients) returned to work by 3 months. Ninety-three percent (67/72 patients) returned to pre-injury work by 6 months. Two patients specifically mentioned having had to change jobs following their operation secondary to their shoulder operation.
Eighty-five percent (56/66 patients) returned to pre-injury sport by 6 months. These were patients involved at various levels (local clubs, college team, county, league, national) in rugby, motocross, cricket, rock climbing, swimming and football. Nine patients did not play any sport. Ten patients did not return to their pre-injury sport because of their shoulder.
Discussion
This technique avoids the donor morbidity associated with harvesting a bone graft from another site, such as the iliac crest. The technique requires a single incision and the graft is harvested locally. Positioning of the graft beomes easier as a result of the reduced bulk of the graft size. The chances of graft breakage when inserting screws are low because the graft is prepared in vitro with pre-drilled holes and the use of K-wires as joysticks. One of the concerns with the Latarjet procedure is that the transferred conjoint tendon can act as a tether to the musculocutaneous nerve. In our modification, there is no distortion of the local anatomy of the conjoint tendon, pectoralis minor tendon, musculocutaneous nerve, axillary nerve and the adjacent neurovascular structures. Revision surgery following a conventional Latarjet becomes even more challenging as a result of the altered local anatomy of the local neurovascular structures. The pectoralis minor tendon is reattached to the coracoid remnant and the conjoint tendon is left undisturbed. The pectoralis minor assists in scapular stability and is an accessory muscle of respiration. The conjoint tendon provides the origin of coraco-brachialis, a weak adductor of the upper arm and the medial half of the biceps muscles, which is a powerful flexor of the elbow and supinator of the forearm. These structures are considered to be functionally important in younger age groups, especially for those who are involved in contact sports such as rugby.
In summary, we consider that our modification of the Latarjet and Eden–Hybinette procedures has the following advantages:
Bone graft is harvested locally without donor morbidity from another site/separate incision.
The conjoint tendon/pectoralis minor, which are considered to be functionally important in this age group, are preserved.
The technique does not distort the local neurovascular/muscular anatomy, making subsequent surgery potentially easier in the future.
The complication/re-dislocation rates compare favourably to the existing literature.
Strengths
The strengths of the present study include that all the patients were independently reviewed. We had a reasonably large cohort of patients with a minimum follow-up of at least 3 years. Our complication rates and re-dislocation rates were low and are comparable to other bone block (Latarjet/Eden–Hybinette/Bristow) series in the literature. The majority of our patients had good outcome scores and a high return to pre-injury work and sports. The operations were performed by different consultants/senior orthopaedic fellows with consistent results, suggesting that this technique is reproducible and relatively easy to perform. This case series includes patients with a minimum glenoid bone loss of 20% on the glenoid ‘en-fosse’ views on CT scans. We have not included patients with no/minimal glenoid bone loss but who demonstrate a high risk of instability, in whom a bony procedure can be recommended to reduce the risk of recurrence. Theoritically, if this technique produces consistent reliable good functional results in patients with bone loss, there is no reason why it should not work in high-risk patients with no bone loss.
Limitations
We acknowledge that this is a retrospective series and nine patients were lost to follow-up. Pre-operative OSIS was not recorded in our patients. Also, residual apprehension might be difficult to assess by postal/telephone OSIS. The patients who were lost to follow-up had their last clinical assessment at approximately 6 months following their operation and were clinically doing well as per the clinic letter with no evidence of residual apprehension. In a case series with a relatively young population, it is likely that some patients will be lost to follow-up because they keep moving from their local area as a result of work/personal circumstances and it becomes difficult to keep track of them. We are unable to provide long-term radiological follow-up for graft union, but X-rays were performed at the last follow-up, which suggest satisfactory graft healing. The external rotation in these patients was not recorded clinically to assess restriction secondary to subscapularis tenotomy. However, the lack of any shoulder instability symptoms at the most recent follow-up/assessment and high return rates to pre-injury active daily living/work/sport suggest that this procedure has a high success rate. Hence, we would infer that subscapularis failure/graft failure/stiffness with restriction of external rotation is not a major problem with this technique. Incidentally, in the two patients who had arthroscopic removal of the screws for discomfort, the graft had healed very well and was indistinguishable from the glenoid articular surface.
We would also caution that, if the anteroinferior glenoid bone loss is very large, then this technique of utilizing 50% of the coracoid may not be sufficient. In these circumstances, the congruent arc Latarjet or techniques that have the ability to provide larger bone graft (iliac crest/allograft) to substitute the bone loss may need to be considered. Another challenging situation could be if the coracoid process is very small, where harvesting 50% may be difficult or the graft cracks during the insertion of the screws. We would recommend that pre-operative/intra-operative planning regarding the size of coracoid, as well as degree of glenoid bone loss, and careful intra-operative positioning of the screws are vital to avoid such complications. We did not come across these complications in our case series.
Acknowledgements
We would like to thank Dr N. Froggatt for her help with the initial collection of data from patients for this study. The study was previously presented as a podium presentation at British Elbow and Shoulder Society Annual Meeting, Nottingham 2014.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000; 16: 677–94. [DOI] [PubMed] [Google Scholar]
- 2.Cerciello S, Edwards TB, Walch G. Chronic anterior glenohumeral instability in soccer players: results for a series of 28 shoulders treated with the Latarjet procedure. J Orthopaed Traumatol 2012; 13: 197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Millett PJ, Clavert P, Warner JP. Open operative treatment for anterior shoulder instability: when and why? J Bone Joint Surg Am 2005; 87: 419–32. [DOI] [PubMed] [Google Scholar]
- 4.Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT II, Matsen FA III. Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder Elbow Surg 1993; 2: 27–35. [DOI] [PubMed] [Google Scholar]
- 5.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop 2002; 400: 65–76. [DOI] [PubMed] [Google Scholar]
- 6.Itoi E, Lee S, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000; 82: 35–46. [DOI] [PubMed] [Google Scholar]
- 7.Latarjet M. Technique of coracoid preglenoid arthroereisis in the treatment of recurrent dislocation of the shoulder. Lyon Chir 1958; 54: 604–7. [PubMed] [Google Scholar]
- 8.Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy 2007; 23: 1033–41. [DOI] [PubMed] [Google Scholar]
- 9.Hovelius L, Sandstrom B, Sundgren K, Saebo M. One hundred eighteen Bristow–Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I – clinical results. J Shoulder Elbow Surg 2004; 13: 509–16. [DOI] [PubMed] [Google Scholar]
- 10.Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am 1998; 80: 841–52. [DOI] [PubMed] [Google Scholar]
- 11.Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, Warner JP. Short-term complications of the Latarjet Procedure. J Bone Joint Surg Am 2012; 94: 495–501. [DOI] [PubMed] [Google Scholar]