Abstract
Acromial and scapular spine fractures after reverse total shoulder arthroplasty occur predominantly as a result of bony insufficiency secondary to patient and intra-operative technical factors. The spectrum of the pathology can range from a stress reaction to an undisplaced or displaced fracture. Prompt diagnosis of these fractures requires a high suspicion in the postoperative patient with a clinical presentation of acute onset of pain along the acromion or scapular spine and/or deterioration of shoulder function. Conventional shoulder radiographs are frequently unreliable in identifying these fractures, especially if they are undisplaced. Computed tomography (CT) and/or single photon emission computed tomography/CT scans are useful imaging modalities for obtaining a definitive diagnosis. Early diagnosis and non-operative treatment of a stress reaction or undisplaced fracture is essential for preventing further displacement and potential disability. The management of displaced fractures is challenging for the orthopaedic surgeon as a result of high rates of mal-union or non-union, decreased functional outcomes, and variable results after open reduction and internal fixation. Strategies for preventing these fractures include optimizing the patient’s bone health, correct glenoid baseplate screw length and position, and avoiding excessive deltoid tension. Further research is required to identify the specific patient and fracture characteristics that will benefit from conservative versus operative management.
Keywords: acromion, periprosthetic fractures, reverse total shoulder arthroplasty, scapula
Introduction
Reverse total shoulder arthroplasty (rTSA) is an effective surgical procedure for rotator cuff arthropathy,1–3 irreparable rotator cuff tears,2–4 fracture sequelae,3,5 and revision shoulder arthroplasty.2,3 Consequently, the utilization of rTSA is increasing, with a reported incidence of 33% in a recent epidemiological study by Schairer et al.6 in primary shoulder arthroplasty. However, the technical challenges of rTSA have resulted in a reported complication rate of 19% to 68%,3,4,7 with the most common complications including scapular notching, glenoid component loosening/failure, infection and instability.2,8
Stress fractures of the shoulder girdle involving the acromion,9–15 scapular spine,16–21 clavicle,22 and coracoid23 after rTSA are less frequent complications and consequently, they have received limited focus within the upper extremity literature. The more common subset of the aforementioned stress fractures occurs in the acromion and scapular spine in 3.1% to 10%9–15,18,19,21 of patients undergoing rTSA and comprises the primary focus of the present review. We consider that this incidence is understated and will increase with improved surgeon awareness of the diagnosis, imaging assessment and expanded utilization of rTSA.
Extensive knowledge of the musculoskeletal and neurovascular anatomy of the shoulder girdle is essential for comprehending the modified biomechanics of the native shoulder after rTSA and for successful implantation of the rTSA, specifically the glenoid component. A comprehensive discussion is beyond the scope of the present review but has been described extensively in the literature.24–29 In Paul Grammont’s original rTSA, the system focused on four key biomechanical principles: (1) a fixed centre of rotation that is distalized and medialized relative to the native level of the glenoid; (2) a deltoid lever arm that must be effective at the start of shoulder movement; (3) the inherent stability of the rTSA; and (4) a semiconstrained articulation created by a large glenosphere and small humeral cup.1,30 The first and second principles highlight the increased stress on the acromion and scapula during post-rTSA shoulder motion.
The deltoid has a broad origin across the lateral third of the clavicle, acromion and scapular spine. It consists of the anterior, middle and posterior heads, which, in the native shoulder, primarily act as a shoulder flexor, abductor and extensor, respectively. After rTSA, the arm is lengthened by approximately 2.5 cm,8,31 which increases the abductor moment arm in all three deltoid heads, thereby converting abduction to their primary function.32 The increased arm length and deltoid tension increases the force between the humeral and glenoid components, therefore improving the stability of the prosthesis.25 However, the modifications made by the orthopaedic surgeon to ensure postoperative stability and deltoid function place an increased stress on the shoulder girdle, which is considered to increase the risk of postoperative fracture.
Acromial and scapular spine fractures after rTSA are a challenge to diagnose and manage for the orthopaedic surgeon and this leads to a decreased functional outcome for the patient. We consider that the bony pathology comprises a spectrum for which the earliest presentation is a stress reaction, which then progresses to an undisplaced fracture and, finally, to a displaced fracture. The present review will discuss the diagnosis, aetiology and management of acromial and scapular spine fractures after rTSA.
Clinical evaluation
A thorough history of the patient’s functional status, postoperative clinical symptoms and onset of pain should be taken. Generally, patients with a postoperative acromial or scapular spine fracture report a period of pain relief from the pre-operative shoulder pathology followed by an acute increase in pain along the acromion or scapular spine. The onset of pain occurs, on average, 2 months to 48 months postoperatively.10,12,16,18,19,33 However, Teusink et al.14 reported a patient with scapular spine fracture 8 years postoperatively. The physiotherapist may report that the patient is progressing slowly with rehabilitation or has deteriorated. A history of a traumatic event is frequently not present, signifying stress fracture. A history of prior shoulder girdle and/or fragility fractures should be explored. In addition, the patient’s past medical history specifically focusing on diseases/conditions that effect bone health (e.g. osteoporosis, cancer, etc.) and current treatment regimens should be assessed.
If the evaluating surgeon did not perform the rTSA, the following information should be obtained: past surgical history of the affected shoulder (e.g. prior acromioplasty), indication for rTSA and operative note (implant system, intra-operative stability and/or complications).
A detailed shoulder examination should be performed with a focus on several key elements. A visible deformity of the acromion or scapula may be present in patients with displaced fractures. However, this may be difficult to determine as a result of the altered appearance of the shoulder contour after rTSA and/or as a result of the patient’s body habitus. The key finding is often point tenderness on palpation over the acromion or scapular spine. Active and passive range of motion (ROM) should be assessed with active elevation and abduction most commonly limited, and pain with resisted antigravity elevation. A thorough examination of the incision for infection, neurovascular status of the upper extremity and stability of the shoulder, as well as other causes of post-rTSA pain and dysfunction, should be undertaken.
Imaging
The position of the rTSA and the presence of periprosthetic fractures should be evaluated on standard shoulder radiographs including anteroposterior, trans-scapular and axillary views. The axillary view is most helpful for assessment of the location of the fracture (e.g. acromion versus scapular spine). This series should be critically compared to pre- and postoperative radiographs to assess any acute change in anatomy or prior bony pathology (i.e. os acromiale or insufficiency fracture) not recognized prior to implantation of the rTSA. Radiographs are often unreliable in the diagnosis of undisplaced acromial or scapular spine fractures, even in the presence of clinical symptoms.9,11,12,14,33 In a series reported by Otto et al.,33 17 of 53 (32.1%) patients presenting with pain initially had negative radiographs but subsequently were found to have displaced fractures. The accuracy of radiographs in their study was only 78.8%. Otto et al.,33 describe that acromial tilt and acromial-to-greater tuberosity distance will increase and decrease respectively on successive radiographs as the fracture displaces. This emphasizes the importance of diagnosing the fractures early before they displace, and treating accordingly. Furthermore, Levy et al.11 showed that interobserver reliability was poor (κ = −0.05) for the diagnosis of a fracture on radiographs at the initial presentation of pain. Therefore, a CT scan of the shoulder including the entire scapula should be ordered when there is a high clinical suspicion and negative radiographs with the aim of making the diagnosis and possibly preventing displacement of the fracture (Figure 1).
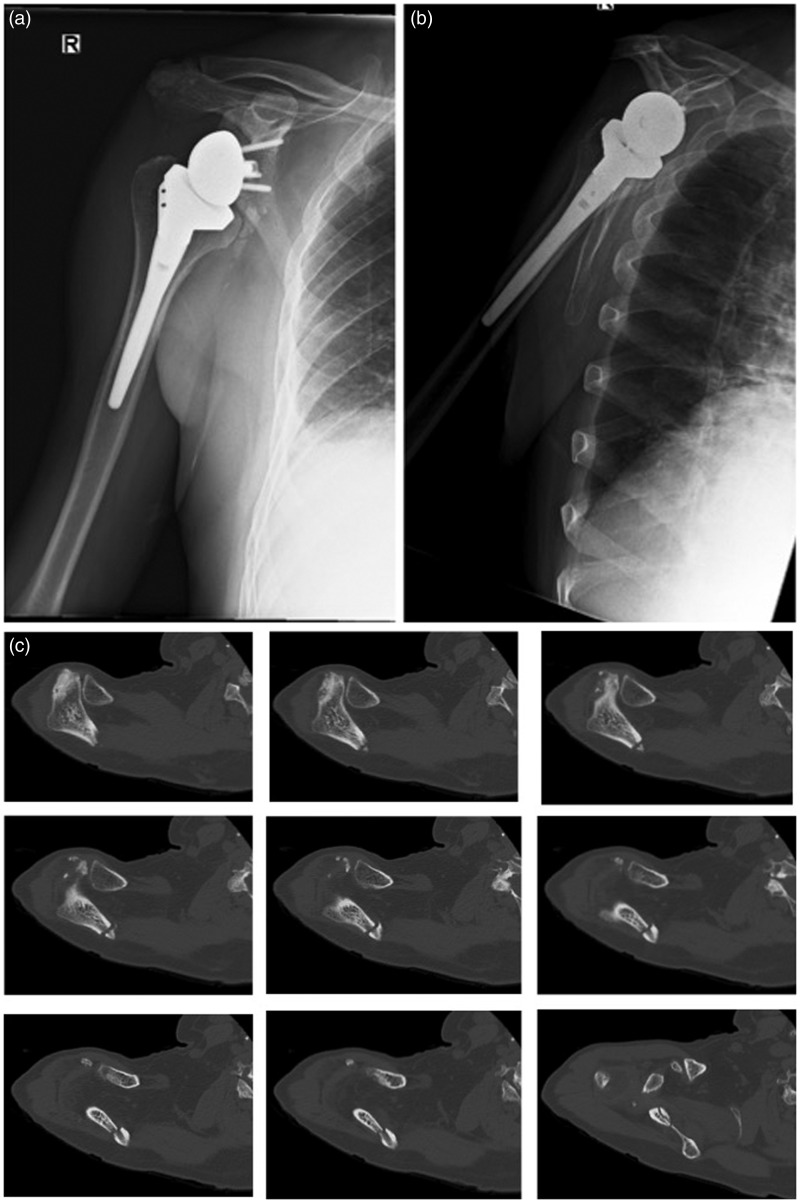
Figure 1.
A 71-year-old patient 16 months after reverse total shoulder arthroplasty with pain along the scapular spine. (a) Anteroposterior and (b) Trans-scapular views did not show a fracture. (c) Axial computed tomography (CT) scan showing a minimally displaced scapular spine fracture 6 weeks after the onset of symptoms.
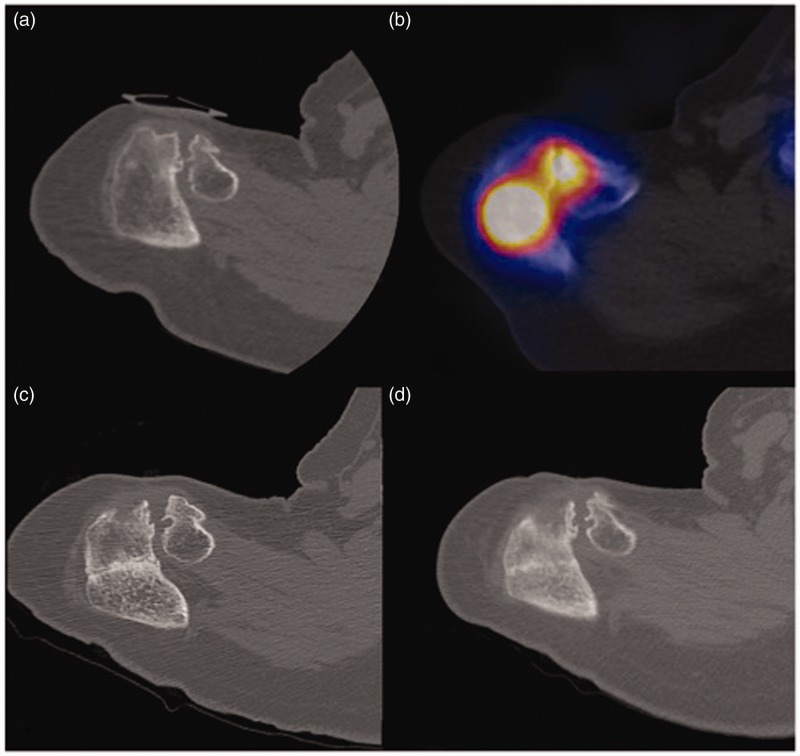
In our experience, single photon emission computed tomography (SPECT)/CT is useful for obtaining a diagnosis of the stress reaction or undisplaced fracture in the symptomatic patient. This relatively new technology fuses both types of imaging, thereby providing a CT image with localization of the pathologic area of radionuclide uptake34 (Figure 2). SPECT/CT imaging has been used for the assessment/diagnosis of pars interarticularis and vertebral compression fractures, multiple foot and ankle pathologies, and postoperative orthopaedic infections.34 The radiation exposure is 80% to 85% less than a standard CT Scan.35 Nicolay et al.36 described the use of SPECT/CT in a patient with bilateral atraumatic scapular spine fractures after rTSA in the radiological literature.
Figure 2.
A 77-year-old patient 4 months after reverse total shoulder arthroplasty. Indicative views of serial computed tomography (CT) and single photon emission computed tomography (SPECT)-CT imaging. (a) CT scan at onset of symptoms did not demonstrate a fracture. (b) SPECT-CT demonstrates areas of increased uptake in acromion and arthritic acromioclavicular joint. (c) CT scan performed 6 weeks after initial presentation demonstrates the acromial fracture in the area identified on SPECT-CT. (d) Repeat CT at 3 months demonstrates sclerosis and callus formation.
Classification
There are two classification systems described in the literature. Crosby et al.9 performed a retrospective review of 22 postoperative fractures and developed a classification system based on fracture location in relation to the acromioclavicular joint on radiographs or CT scans. Type I fractures (n = 8) were located in the anterior acromion. It was hypothesized that this fracture type occurred as a result of acromial wear from prior acromioplasty. Type II fractures (n = 10) involved the acromial body posterior to the acromioclavicular joint. Type III fractures (n = 4) included the scapular spine with the fracture line extending from the tip of the superior metaglene screw. Otto el al.33 found this system to have moderate inter-rater reliability (κ = 0.422).
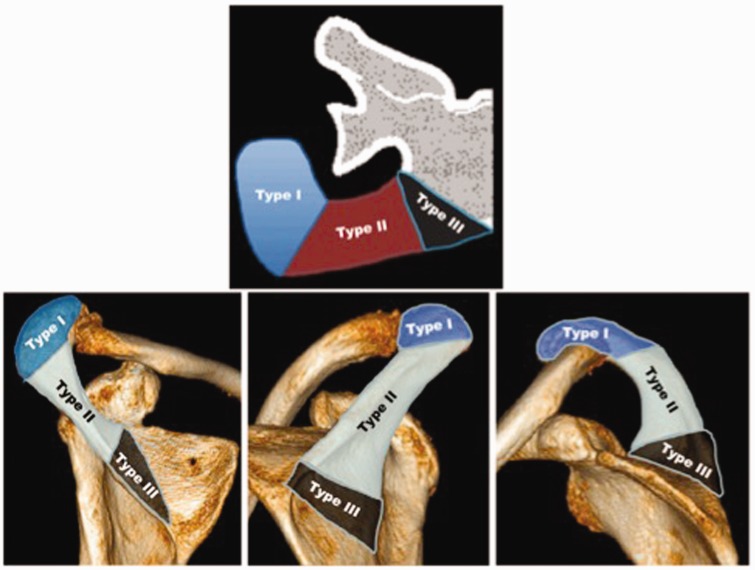
Levy et al.11 developed a classification system after reviewing 18 patients with postoperative acromion or scapular spine pain. In seven (39%) patients, the radiographs were negative and a CT scan was required to obtain the diagnosis of an undisplaced fracture. The fractures were classified into subtypes using the location of the fracture in relation to deltoid origin (Figure 3). All fractures were treated non-operatively. Interobserver reliability (κ = 0.96) and agreement (87.5%) were excellent.11
Figure 3.
Classification of acromial fractures. Courtesy of Levy et al.11
Both classification systems provide a simple outline for the various types of acromial and scapular spine fractures based on location. However, they are limited by small samples sizes, a lack of validation and an inability to provide guidance for the management of the fracture types.
Aetiology
Postoperative acromial and scapular spine fractures are considered to occur as a result of bony insufficiency secondary to patient and/or intra-operative technical factors.
The patient factors examined in the literature include: patient co-morbidities33 and pre-operative acromial insufficiency.21,37 Otto et al.33 examined the clinical risk factors in 53 patients with postoperative scapula fractures. Osteoporosis was present in 30.8% of fracture patients compared to 18.4% of control patients (p < 0.05). It was the only clinical risk factor found to significantly increase the risk of postoperative scapular fractures (odds ratio 1.97; 95% confidence interval 1.00 to 3.91).33 Osteopaenia, endocrine disease, autoimmune disease, excessive alcohol intake, smoking and corticosteroid use were not significant risk factors. However, the study may have been underpowered to identify these risk factors because they are all known to have negative effects on bone density.
Walch et al.21 examined whether pre-operative acromial insufficiency had an effect on the clinical outcome of patients who underwent rTSA. Their series consisted of 41 of 457 (9%) rTSAs with either an os acromiale (n = 23), fatigue fracture (n = 17) or stress fracture non-union (n = 1). There was no difference between rTSAs with and without pre-operative acromial pathology with respect to Constant score, active elevation and subjective satisfaction.21 Implantation of the rTSA resulted in a progression of inferior acromial tilt in 62.5% (n = 20) of patients who had pre-operative tilt. An increase in acromial tilt did not correlate with decreased functional outcomes or shoulder ROM. We have, however, seen multiple patients with increased acromial tilt over time, which correlated with a major deterioration of function. Four (0.8%) patients who did not have any pre-operative acromial pathology sustained a postoperative scapular spine fracture. This group had worse outcomes compared to the other groups. Walch et al.21 hypothesized that the broad deltoid insertion to scapula and clavicle in addition to unaffected scapulothoracic ROM accounted for the similar outcomes between groups. Mottier et al.37 described similar outcomes between patients with and without pre-operative acromial pathology. There is no evidence in the literature for pre-operative acromial pathology being associated with postoperative acromial and scapular spine fractures. We have not had a similar experience with pre-operative acromial pathology and have observed that postoperative clinical outcomes and ROM are more variable.
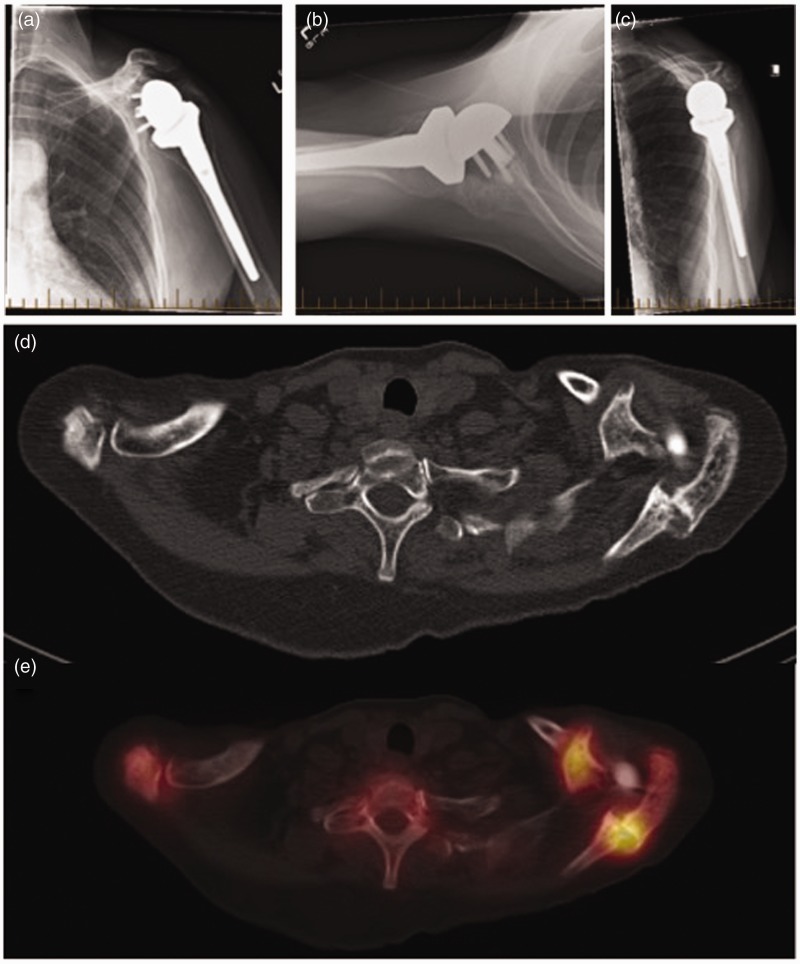
In our experience, a post-rTSA acromial or scapular spine fracture places the patient at an increased risk for other stress fractures in the ipsilateral shoulder girdle. We consider that this occurs as a result of the increased stress on the surrounding bony and ligamentous anatomy (e.g. coracoid, clavicle, acromioclavicular joint) during fracture healing and/or if a mal- or non-union occurs. A case example is shown in Figure 4.
Figure 4.
A 61-year-old female patient who complained of anterior shoulder pain 12 months after a left reverse total shoulder arthroplasty (rTSA) for rheumatoid arthritis. At 3 months post-rTSA, she was diagnosed with a scapular spine stress fracture. This was treated conservatively and complete union occurred at 6 months. (a) Anteroposterior, (b) axillary and (c) trans-scapular views of the left shoulder 1 year after rTSA. (d) An axial computed tomography (CT) scan did not show a coracoid fracture. (e) A single photon emission computed tomography/CT scan showed increased uptake in the previous scapular spine fracture and base of the coracoid, consistent with an undisplaced coracoid stress fracture. This was treated conservatively and symptoms resolved after 3 months.
The intra-operative technical factors include: glenoid baseplate screw position/length9,20,33 and excessive deltoid tension secondary to arm lengthening.2,8,10,11,33 No association has been found between primary or revision rTSA and these fractures.
Glenoid baseplate fixation has recently been a focus in the literature regarding number, length and position of screws. Otto et al.33 observed that 14 of 16 post-rTSA scapular spine fractures were associated with a screw: seven long (26 mm or 30 mm) posterior–superior peripheral screws, four short (14 mm or 18 mm) posterior–superior peripheral screws ending at the spinoglenoid notch and three anteverted central screws. Further analysis of the surgical technique (e.g. baseplate orientation, screw length and distance from screw tip to edge of bone) between groups did not yield any statistically significant findings. Otto et al.33 consider that the fracture occurred around the screw and not because of the screw and therefore did not alter their surgical technique. Conversely, Crosby et al.9 described three patients who had scapular spine fractures associated with the superior metaglene fixation screw in the Delta III rTSA (DePuy, Warsaw, IN, USA). It was hypothesized that the superior metaglene screw acted as a stress riser in this prosthesis and thus Crosby et al.9 have modified their surgical technique by not inserting it routinely. Decreasing the number of screws placed in the glenoid is supported by the biomechanical study by James et al.38 showing that there was no significant difference in the average peak displacements of glenoid baseplates with two versus four screws (p = 0.338).
The variability in glenoid base plate designs and screw diameter, number and location amongst the orthopaedic implant manufacturers makes it challenging to provide a consensus on optimal screw position. The optimal bone for screw fixation is found within the base of the coracoid, scapular spine and scapular pillar.24,26 The malposition of the superior (12 o’clock position) and posterior (9 o’clock position right and 3 o’clock position left shoulder) screws has been proposed to be associated with scapular spine stress fractures.9 Therefore, several recommendations can be provided based on extensive operative experience and the the available literature.
We advocate for the superior screw to be ≤24 mm in length and angled anterior and superior into the base of the coracoid. This screw trajectory and length optimizes fixation and prevents breaching the suprascapular notch and injuring the suprascapular nerve. Longer screw lengths (e.g. >30 mm) have been associated with an increased risk of nerve injury and extraosseous placement.24,28
The posterior screw has traditionally been described to use the scapula spine for additional fixation.39 However, we agree with Crosby et al.9 that this screw is a potential risk for creating a stress riser in the scapular spine. In addition, the posterior screw has a high risk of breaching the spinoglenoid notch and injuring the suprascapular nerve/artery.26,28 Therefore, we avoid placing this screw into the scapular spine by using a short posterior screw (≤20 mm). Further research is required to adequately assess the association between glenoid base plate screws and scapular spine fractures.
Increased deltoid tension secondary to over lengthening the arm is a proposed technical risk factor.2,8,10,11,33,40 However, there is no evidence in the current literature directly linking this relationship. As a result of the initial concern for postoperative instability, we consider that there has been a trend for rTSAs to be inserted with undue tension on the deltoid. Intra-operative assessment of deltoid tension and rTSA stability is based on numerous subjective recommendations5,40 that we consider to be influenced by surgeon experience and patient characteristics (e.g. muscle relaxation, revision surgery, etc.). Ladermann et al.31 developed a standardized pre-operative radiographic technique to assess deltoid tension. There was a significant association between inadequate deltoid tension and postoperative instability (p < 0.0001). Two postoperative scapula fractures were observed, although there was no association with excessive deltoid tension (p = 0.830). However, the study population was small and underpowered to adequately determine an association. Although postoperative rTSA instability is a dreaded complication, the surgeon should be cognizant of inserting the rTSA with excessive deltoid tension.
Management
The management of postoperative acromial and scapular spine fractures is challenging for the orthopaedic surgeon because of the high rates of mal- or non-union,10,12,14,18–20 decreased functional outcomes10–12,14,15,18–21 and variable results after open reduction and internal fixation (ORIF).9,13,15,16,21 Hamid et al.10 surveyed 54 members of the American Shoulder and Elbow Surgeons and found that 61.5% had encountered this complication, with 75% treating the fracture conservatively, 22% with ORIF and 3% with revision rTSA. A literature review of the management of these fractures is provided in Table 1.
Table 1.
Literature review of the treatment of acromial and scapular spine fractures after reverse total shoulder arthroplasty
| Article | Number of fractures | Incidence (%) | Fracture location | Treatment | Follow-up (months) | Fracture union | Clinical outcome (mean) |
|---|---|---|---|---|---|---|---|
| Camarada et al.16 | 1 | NA | Scapular spine | ORIF (mesh plate + TBW + ICBG) | 12 | 52 weeks | AE 100°, Abd 100° ASES 52, DASH 48 |
| Crosby et al.9 | 22 | 5.5 | Type I: 8 Type II: 10 Type III: 4 | Type 1: Conservative Type 2: 3 Conservative, 3 acromioclavicular joint resection, 4 ORIF Type 3: 4 ORIF | 3 to 54 | Not mentioned | Type I: symptom resolution Type II: symptom resolution Type III: 1 revision ORIF, 1 hardware removal. Symptom resolution |
| Familiari et al.17 | 1 | NA | Scapular spine | Sling immobilization | 11 | Non-union | No pain |
| Hamid et al.10 | 8 | 4.9 | 4 acromion base, 3 mid-acromion, 1 anterior acromion | Abduction pillow | 35 | 6 Non-unions 2 Mal-unions | AE 71° ASES 70 |
| Hattrup18 | 9 | 7.2 | 3 acromion, 6 scapular spine | Sling immobilization | 12 | 1 Union 8 Non-unions | AE 97°, Abd 90° ASES 44.5 |
| Levy et al.12 | 1 | NA | Acromion base | Shoulder immobilization Revision rTSA (after second fall and subsequent instability) | 29 | Mal-union, subsequent revision rTSA | AE 70°, Abd 55° ASES 13.3 |
| Levy et al.11 | 16 | 10 | Type I: 2 Type II: 8 Type III: 6 | Sling immobilization | 25 | Not mentioned | AE 77°, Abd 64° ASES 44 |
| Lopiz et al.19 | 4 | 3.3 | Scapula spine | Sling immobilization | 39.6 | Union: 50% | AE: 39°, Abd 34° Constant Score 66.5 |
| Rouleau et al.13 | 1 | NA | Acromion base | ORIF (90-90 plate) | 18 | Not mentioned | AE 160°, Abd 125° Constant Score 69 |
| Stevens et al.20 | 2 (1 patient) | NA | Right: acromion base Left: scapular spine | Sling immobilization | Right: 6 years Left: 4 years | Bilateral non-union | Right: AE 37°, ASES 50°, Constant score 32 Left: AE 55°, ASES 42°, Constant score 31 |
| Teusink et al.14 | 25 | 3.1 | 17 Acromion 8 Scapular spine | Sling immobilization | 50 | Acromion Union: 57% Scapular spine Union: 50% | ROM All fractures: AE 90°, Abd 80° Controls: AE 135°, Abd 130° ASES Acromion: 59.9 Scapular spine: 53.8 Controls: 74.2 |
| Wahlquist et al.15 | 5 | NA | Acromion base | 2 Abduction pillow 3 ORIF (2 plate, 1 TBW) | 13-26 | Non-op: 11, 29 weeks ORIF: 7.5 weeks to 42 weeks | Non-Op: AE 95° to 150° Neer functional outcome: 56 to 76 ORIF: AE 40° to 125° Neer functional outcome: 77 |
| Walch et al.21 | 4 | 0.8 | Scapular spine | 3 Abduction pillow 1 ORIF (TBW) + hardware removal | 24-36 | Non-Op: 1 Non-union, 2-Union (24 months) ORIF 1 Non-union | AE: 81° Constant score: 35 |
Abd, abduction; AE, active elevation; ASES, American Shoulder & Elbow Surgeons; DASH, Disabilities of the Arm, Shoulder and Hand; ICBG, iliac crest bone graft; NA, not available; ORIF, open reduction and internal fixation; rTSA, reverse total shoulder arthroplasty; TBW, tension band wiring.
Non-operative management of acromial and scapular spine fractures includes temporary cessation of the physiotherapy programme and immobilization of the affected shoulder with either a sling or abduction pillow for at least 6 weeks (Table 1).10,11,12,14,18,19,20 No difference between the types of immobilization has been demonstrated. This management is particularly important in the early stages of a stress reaction or undisplaced fracture with respect to preventing it progressing to a displaced fracture. We use an abduction pillow for a period of 6 weeks or until the symptoms subside. Overall, the union rate is approximately 50% and the final clinical outcomes are significantly decreased compared to non-fracture post-rTSA patients.14,18 However, the fracture patients do have clinical improvement compared to their pre-operative status.14,18 In our experience, an early diagnosis of a fracture is essential prior to displacement, which we consider to be related to worse outcomes. Additionally, we consider that acromial fractures (Levy et al.11: Types 1 and 2) should be treated conservatively because surgical fixation is difficult and often unsuccessful.
Surgical management specifically of acromial base and scapular spine fractures has been described in the literature.9,13,15,16,21 With this fracture type, an increased amount of deltoid origin is involved and therefore may be defunctioned with a mal- or non-union. The goal of the fixation construct is to apply compression at the fracture site and neutralize the distraction forces of the deltoid. The main challenge in the surgical management is obtaining adequate fixation in osteopaenic/osteoporotic bone. Tension band fixation has inconsistent results, including hardware failure and non-union.15,21 This construct neutralizes forces parallel to the tension band axis. However, the broad insertion of the deltoid creates forces in multiple directions, thereby theoretically increasing the failure of this construct. Rigid plate fixation has been proposed to improve the fixation and stability of the construct.9,13,15 Camarada et al.16 and Rouleau et al.13 described the use of a mesh plate and ‘90-90’ small fragment locking plate configurations, respectively, for the treatment of displaced scapular spine fractures with good clinical results and fracture union. Complications associated with rigid fixation include hardware failure and prominence.15 However, despite the proposed benefits of ORIF, there is no substantial evidence showing a clinically significant decrease in time to union or improved clinical outcomes compared to non-operative treatment.
Conclusions
Acromial and scapular spine fractures after rTSA are challenging complications to manage. The orthopaedic surgeon should have a high clinical suspicion in the patient with progressive pain along the acromion or scapular spine and/or an acute decrease in shoulder function. Standard shoulder radiographs and/or CT Scans should be scrutinized for a fracture. SPECT/CT scans may provide additional diagnostic information, particularly in cases with a suspected stress reaction or undisplaced fracture. Prompt diagnosis and appropriate early treatment is essential for preventing further displacement of the fracture, which we consider to be associated with worse outcomes.
Prevention of this complication in our opinion is the best method of treatment. This includes optimizing bone health in at-risk patients in conjunction with a medical specialist. Intra-operative technical factors include optimal superior and posterior screw length and position and the avoidance of over-tensioning the deltoid. The current literature on non-operative versus operative treatment for these fractures consists of small retrospective case reports and series and therefore precludes the development of a defined treatment algorithm. Further research is needed to determine the optimal treatment for specific types of patients (e.g. osteopaenia/osteoporotic) and fracture location (e.g. acromion versus scapular spine).
Acknowledgements
The authors thank Mr Gregory Bain for providing Figure 2 and Dr Jonathan C. Levy for permission to use Figure 3.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Boileau P, Gonzalez JF, Chuinard C, et al. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009; 18: 600–6. [DOI] [PubMed] [Google Scholar]
- 2.Matsen FA, III, Boileau P, Walch G, et al. The reverse total shoulder arthroplasty. J Bone Joint Surg Am 2007; 89: 660–7. [DOI] [PubMed] [Google Scholar]
- 3.Wall B, Nové-Josserand L, O’Connor DP, et al. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am 2007; 89: 1476–85. [DOI] [PubMed] [Google Scholar]
- 4.Rittmeister M, Kersch-Baumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and non reconstructable rotator cuff lesions. J Shoulder Elbow Surg 2001; 10: 17–22. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 2005; 14: 147S–61S. [DOI] [PubMed] [Google Scholar]
- 6.Schairer WW, Nwachukwu BU, Lyman S, et al. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2015; 24: 91–7. [DOI] [PubMed] [Google Scholar]
- 7.Saltzman BM, Chalmers PN, Gupta AK, et al. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: 1647–54. [DOI] [PubMed] [Google Scholar]
- 8.Farshad M, Gerber C. Reverse total shoulder arthroplasty – from the most to the least common complication. Int Orthop 2010; 34: 1075–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crosby LA, Hamilton A, Twiss T. Scapula fractures after reverse total shoulder arthroplasty: Classification and treatment. Clin Orthop 2011; 469: 2544–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamid N, Connor PM, Fleischli JF, et al. Acromial fracture after reverse shoulder arthroplasty. Am J Orthop 2011; 40: E125–9. [PubMed] [Google Scholar]
- 11.Levy JC, Anderson C, Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am 2013; 95: E104–E104. [DOI] [PubMed] [Google Scholar]
- 12.Levy JC, Blum S. Postoperative acromion base fracture resulting in subsequent instability of reverse shoulder replacement. J Shoulder Elbow Surg 2012; 21: E14–8. [DOI] [PubMed] [Google Scholar]
- 13.Rouleau DM, Gaudelli C. Successful treatment of fractures of the base of the acromion after reverse shoulder arthroplasty: case report and review of the literature. Int J Shoulder Surg 2013; 7: 149–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Teusink MJ, Otto RJ, Cottrell BJ, et al. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg 2014; 23: 782–90. [DOI] [PubMed] [Google Scholar]
- 15.Wahlquist TC, Hunt AF, Braman JP. Acromial base fractures after reverse total shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg 2011; 20: 1178–83. [DOI] [PubMed] [Google Scholar]
- 16.Camarada L, Phadnis J, Clitherow HD, et al. Mesh plates for scapula fixation. Tech Should Surg 2015; 16: 79–84. [Google Scholar]
- 17.Familiari F, Huri G, Gonzalez-Zapata A, et al. Scapula fracture and os acromiale after reverse total shoulder arthroplasty. Orthopedics 2014; 37: 492–5. [DOI] [PubMed] [Google Scholar]
- 18.Hattrup SJ. The influence of postoperative acromial and scapular spine fractures on the results of reverse shoulder arthroplasty. Orthopedics 2010; 33 . doi: 10.3928/01477447-20100329-04. [DOI] [PubMed] [Google Scholar]
- 19.Lópiz Y, Rodríguez-González A, García-Fernández C, et al. Scapula insufficiency fractures after reverse total shoulder arthroplasty in rotator cuff arthropathy: what is their functional impact? Rev Esp Cir Ortop Traumatol 2015; 59: 318–25. [DOI] [PubMed] [Google Scholar]
- 20.Stevens CG, Murphy MR, Stevens TD, et al. Bilateral scapular fractures after reverse shoulder arthroplasties. J Shoulder Elbow Surg 2015; 24: E50–5. [DOI] [PubMed] [Google Scholar]
- 21.Walch G, Mottier F, Wall B, et al. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg 2009; 18: 495–502. [DOI] [PubMed] [Google Scholar]
- 22.Anakwenze OA, Pifer MA, Singh A. Clavicle stress fracture after reverse shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: E170–2. [DOI] [PubMed] [Google Scholar]
- 23.Anakwenze OA, Kancherla VK, Carolan GF, et al. Coracoid fracture after reverse total shoulder arthroplasty: a report of 2 cases. Am J Orthop 2015; 44: E469–72. [PubMed] [Google Scholar]
- 24.DiStefano JG, Park AY, Nguyen TQ, et al. Optimal screw placement for base plate fixation in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2011; 20: 467–76. [DOI] [PubMed] [Google Scholar]
- 25.Gagey O, Hue E. Mechanics of the deltoid muscle. A new approach. Clin Orthop 2000; 375: 250–7. [DOI] [PubMed] [Google Scholar]
- 26.Hart ND, Clark JC, Wade Krause FR, et al. Glenoid screw position in the encore reverse prosthesis: an anatomic dissection study of screw relationship to surrounding structures. J Shoulder Elbow Surg 2013; 22: 814–20. [DOI] [PubMed] [Google Scholar]
- 27.Karelse A, Kegels L, De Wilde L. The pillars of the scapula. Clin Anat 2007; 20: 392–9. [DOI] [PubMed] [Google Scholar]
- 28.Molony DC, Cassar Gheiti AJ, Kennedy J, et al. A cadaveric model for suprascapular nerve injury during glenoid component screw insertion in reverse-geometry shoulder arthroplasty. J Shoulder Elbow Surg 2011; 20: 1323–7. [DOI] [PubMed] [Google Scholar]
- 29.Von Schroeder HP, Kuiper SD, Botte MJ. Osseous anatomy of the scapula. Clin Orthop 2001; Feb: 131–9. [DOI] [PubMed] [Google Scholar]
- 30.Grammont P, Trouilloud P, Laffay J, et al. Etude et realisation d’une nouvelle prothese d’epaule. Rheumatologie 1987; 39: 407–18. [Google Scholar]
- 31.Lädermann A, Williams MD, Melis B, et al. Objective evaluation of lengthening in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2009; 18: 588–95. [DOI] [PubMed] [Google Scholar]
- 32.Berliner JL, Regalado-Magdos A, Ma CB, et al. Biomechanics of reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2015; 24: 150–60. [DOI] [PubMed] [Google Scholar]
- 33.Otto RJ, Virani NA, Levy JC, et al. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg 2013; 22: 1514–21. [DOI] [PubMed] [Google Scholar]
- 34.Scharf S. SPECT/CT imaging in general orthopedic practice. Semin Nucl Med 2009; 39: 293–307. [DOI] [PubMed] [Google Scholar]
- 35.Montes C, Tamayo P, Hernandez J, et al. Estimation of the total effective dose from low-dose CT scans and radiopharmaceutical administrations delivered to patients undergoing SPECT/CT explorations. Ann Nucl Med 2013; 27: 610–7. [DOI] [PubMed] [Google Scholar]
- 36.Nicolay S, De Beuckeleer L, Stoffelen D, et al. Atraumatic bilateral scapular spine fracture several months after bilateral reverse total shoulder arthroplasty. Skeletal Radiol 2014; 43: 699–702. [DOI] [PubMed] [Google Scholar]
- 37.Mottier F, Wall B, Nove-Josserand L, et al. Reverse prosthesis and os acromiale or acromion stress fracture. Rev Chir Orthop Reparatrice Appar Mot 2007; 93: 133–41. [DOI] [PubMed] [Google Scholar]
- 38.James J, Allison MA, Werner FW, et al. Reverse shoulder arthroplasty glenoid fixation: is there a benefit in using four instead of two screws? J Shoulder Elbow Surg 2013; 22: 1030–6. [DOI] [PubMed] [Google Scholar]
- 39.Hoenig MP, Loeffler B, Brown S, et al. Reverse glenoid component fixation: is a posterior screw necessary? J Shoulder Elbow Surg 2010; 19: 544–9. [DOI] [PubMed] [Google Scholar]
- 40.Lädermann A, Edwards TB, Walch G. Arm lengthening after reverse shoulder arthroplasty: a review. Int Orthop 2014; 38: 991–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]