Abstract
Immunogenic cell death (ICD) is characterized by the early surface exposure of calreticulin (CRT). As a specific signaling molecule, CRT on the surface of apoptotic tumor cells mediates the recognition and phagocytosis of tumor cells by antigen presenting cells. To date, only a small quantity of anti-cancer chemicals have been found to induce ICD, therefore it is clinically important to identify novel chemicals that may induce ICD. The purpose of the present study is to explore the function of capsaicin in inducing ICD. In the current study, MTT assays were used to examine the growth inhibiting effects of MG-63 cells when they were treated with capsaicin or cisplatin. Mitochondrial membrane potential and western blot analysis were used to investigate capsaicin- and cisplatin-induced apoptosis. In addition, the effects of capsaicin and cisplatin were evaluated for their abilities in inducing calreticulin membrane translocation and mediating ICD in human osteosarcoma cells (MG-63). The results demonstrated that capsaicin and cisplatin can induce the apoptosis of MG-63 cells. However, only capsaicin induced a rapid translocation of CRT from the intracellular space to the cell surface. Treatment with capsaicin increased phagocytosis of MG-63 cells by dendritic cells (DCs), and these MG-63-loaded DCs could efficiently stimulate the secretion of IFN-γ by lymphocytes. These results identify capsaicin as an anti-cancer agent capable of inducing ICD in human osteosarcoma cells in vitro.
Keywords: capsaicin, immunogenic cell death, calreticulin, osteosarcoma, tumor specific immune response, dendritic cells, phagocytosis assays
Introduction
Osteosarcoma (OS) is the most common primary malignant bone tumor in children and adolescents (1). OS arises predominantly in the long bone metaphysis, particularly in the distal femur, proximal tibia and proximal humerus (2). Previously, the majority of patients with OS were treated by amputation; however, the 5-year survival rate was <20%, primarily due to lung metastases (3). With the introduction of chemotherapy into multi-modal treatment for OS, its prognosis has improved (2). In the past 20 years, although numerous international research groups have conducted a large quantity of research on OS, its survival rate remains unchanged (4–6).
The concept of immunogenic cell death (ICD) of tumor cells has emerged in recent years, which is a cell death modality that is able to stimulate an immune response against homologous tumor cells (7,8). This concept was first proposed in the context of anticancer chemotherapy, and was based on animal experiments that indicated that tumor specific immune responses could determine the efficacy of anticancer therapies (9). ICD is characterized by the early surface exposure of calreticulin (CRT) (10).
To date, only a small number of conventional cytotoxic anticancer therapeutics are able to induce ICD (11); therefore it is of clinical significance to identify novel chemicals that can induce ICD. Capsaicin, a homovanillic acid derivative and the spicy component of chili pepper, has been shown to have cytotoxicity towards cancer cells and immunomodulatory functions, suggesting its potential application in tumor therapy (12). It has been reported that intratumoral administration of capsaicin elicits a T cell-mediated antitumor immune response, resulting in the regression of advanced preexisting solid tumors (12). In addition, research by D'Eliseo et al (13) indicates that capsaicin can stimulate anticancer immunity.
In the present study, the effects of capsaicin were evaluated for its abilities in inducing CRT membrane translocation and mediating ICD in a human MG-63 OS cell line. As it has been reported that cisplatin could not induce ICD in tumor cells, the present study used cisplatin as a control. The present results indicated that capsaicin induced a rapid membrane translocation of CRT. Furthermore, apoptotic MG-63 cells induced by capsaicin could be engulfed more efficiently by phagocytes and these phagocytes loaded with apoptotic MG-63 cells had the stronger ability in activating tumor-specific T-cells which could secrete IFN-γ. These data demonstrate that capsaicin can induce ICD in human OS cells.
Materials and methods
Cell line
The human OS cell line MG-63 was purchased from the Cell Bank of China (Wuhan, China). The cells were maintained at 37°C in 5% CO2 and Dulbecco's modified Eagle medium (DMEM), which contains 10% heat-inactivated fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA), 100 µg/ml streptomycin and 100 units/ml penicillin.
Materials
Capsaicin, DMEM, 3,3′-dihexyloxacarbocyanine iodide (DiOC6)(3) and MTT were purchased from Sigma-Aldrich (St. Louis, MO, USA). Rabbit-anti-human CRT polyclonal antibody was purchased from Stressgen (Victoria, BC, Canada; cat. no. SPC-122B). Mouse anti-human phycoerythrin (PE)-conjugated CD11c monoclonal antibody was purchased from eBioscience (San Diego, CA, USA; cat. no. 12-0116-42). Rabbit anti-B-cell lymphoma 2 (Bcl-2) and rabbit anti-Bcl-2-associated X protein (Bax) monoclonal antibodies, and horseradish peroxidase (HRP)-conjugated anti-rabbit IgG, were purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX, USA; cat. nos. sc-492, sc-6236 and sc-516087, respectively). PE-conjugated goat anti-rabbit IgG polyclonal antibody was obtained from R&D Systems, Inc. (Minneapolis, MN, USA; cat. no. IC108P). Recombinant human interleukin (IL)-2, IL-4 and granulocyte-macrophage colony-stimulating factor (GM-CSF) were purchased from PeproTech (Rocky Hill, NJ, USA). Lymphocyte separation medium was purchased from Tianjin Haoyang Biological Manufacture, Co., Ltd. (Tianjin, China). IL-4 and IFN-γ enzyme-linked immunosorbent assay (ELISA) kits were purchased from Wuhan Boster Biological Technology, Ltd. (Wuhan, China).
MTT assay
MG-63 cells were seeded onto 96-well tissue culture plates at a density of 2×103 cells/100 µl per well, and incubated for 24 h at 37°C. The next day, the media were replaced with 100 µl fresh complete medium containing capsaicin (0, 12.5, 25, 50, 100, 200 and 400 µM) and cisplatin (0, 4, 8, 16, 32, 64 and 128 µg/ml). The cells treated with equal quantities of normal medium or solvent, instead of drugs, served as the control. After 24 h incubation, 100 µl MTT solution (0.5 mg/ml) in DMEM without fetal bovine serum was added to each well and cultured for 4 h at 37°C in a humidified atmosphere. The medium was removed and 150 µl DMSO was added into each well to dissolve the purple crystals, then the absorbance (A) at 570 nm was recorded. The cell proliferation inhibition rate was calculated according to the following formula: Cell proliferation inhibition rate = (Acontrol - Adrug)/Acontrol × 100%.
Mitochondrial membrane potential (MMP)
The lipophilic fluorescence dye DiOC6 (3) (40 nM) was used to assay the mitochondrial membrane permeabilization. MG-63 cells (2×106) treated with 200 µM capsaicin or 32 µg/ml cisplatin were stained with DiOC6 (3) for 15 min at 37°C and analyzed immediately by flow cytometry (FCM) equipped with a standard 15 mW argon-ion laser (488 nm) to excite DiOC6 (3). Then, a narrow band filter was used to collect emissions between 515 and 545 nm. A minimum of 10,000 cells were analyzed by FCM for each data point.
Western blot analysis
MG-63 cells (2×106) were cultured in DMEM medium containing 200 µM capsaicin or 32 µg/ml cisplatin for 12 or 24 h and harvested. Cells were then lysed with cell lysis buffer (Tris 50 mM, NaCl 150 mM, SDS 0.1%, Sodium Deoxycholate 0.5% and 1% Triton X-100) for 20 min on ice. The protein concentrations were determined using the Pierce BCA Protein Assay kit (Thermo Fisher Scientific, Inc.), after which the proteins in the lysate (45 µg) were separated by 10% SDS-PAGE and transferred onto a PVDF membranes. The membranes were blocked with fat-free milk solution (5%, w/v) for 12 h and then incubated with rabbit anti-Bcl-2 and anti-Bax monoclonal antibodies (1:1,000) or anti-CRT polyclonal antibody (1:1,000) at 4°C for 12 h. After washing 3 times with TBST, the membrane was incubated with an HRP-conjugated anti-rabbit IgG antibody (1:4,000) at room temperature for 1 h and developed using electrochemiluminescence.
Detection of CRT on the cell surface by FCM
MG-63 cells were cultured in DMEM medium containing 200 µM capsaicin or 32 µg/ml cisplatin for 12 h and harvested. After washing once with phosphate-buffered saline (PBS), the cells were incubated with rabbit anti-CRT polyclonal antibody (1:1,000) at room temperature for 1 h, following by washing and incubation with PE-conjugated goat anti-rabbit IgG polyclonal antibody (1:500) at room temperature for 2 h (avoiding light). After washing with PBS, the cells were analyzed by FCM to identify CRT on the cell surface.
In vitro phagocytosis assays
Peripheral blood mononuclear cells (PBMCs) were isolated from human blood using lymphocyte separation medium (density, 1.077 g/ml) according to the manufacturer's instructions. Following the last wash, PBMCs (5×106) were resuspended in RPMI-1640 and plated in 6-well culture plates. After 3 h incubation, the monocytes were purified by removing the non-adherent cells in the supernatant. Purified monocytes were cultured in a medium supplemented with 30 ng/ml recombinant human GM-CSF and 10 ng/ml recombinant human IL-4 in 6-well plates (1×106 cells/well). After 7 days, the non-adherent and loosely adherent cells were harvested as the dendritic cells (DCs) and were used as the effector cells for the phagocytosis assay. The MG-63 cells (1×106) incubated with 200 µM capsaicin or 32 µg/ml cisplatin for 12 h were labeled with the green dye carboxyfluorescein diacetate succinimidyl ester (1 µM) for 10 min and were used as the target cells. The effector and target cells were co-cultured at 37°C for 2 h at a 1:1 effector/target ratio. After 3 washes, anti-human CD11c PE was added to the cell mixture for 30 min at room temperature (in the dark) to label the effector cells. The cells were washed with PBS and analyzed by FCM. The phagocytotic efficiency was represented by the cell ratio of the double-positive cell number over the total cell number.
IFN-γ and IL-4 expression level analysis
PBMCs were isolated as described above. Following the last wash, PBMCs (5×106) were resuspended in RPMI-1640 and plated in 6-well culture plates. After 3 h incubation, the non-adherent cells were harvested as lymphocytes, and DCs were induced as described above. The DCs loaded with drug-treated MG-63 cells were co-cultured with lymphocytes at a ratio of 1:4. A volume of 200 U/ml IL-2 was added into the cell mixture during the culture period. After 24 h, the supernatant was collected, and the IFN-γ and IL-4 expression levels in the supernatant were measured by ELISA, according to the manufacturer's instructions.
Statistical analysis
Data are presented as the mean ± standard deviation of three independent experiments. Student's t-tests were performed for the comparison of results between different groups. All of the tests were performed using SPSS software, version 17.0 (SPSS, Inc., Chicago, IL, USA). P<0.05 was considered to indicate a statistically significant difference.
Results
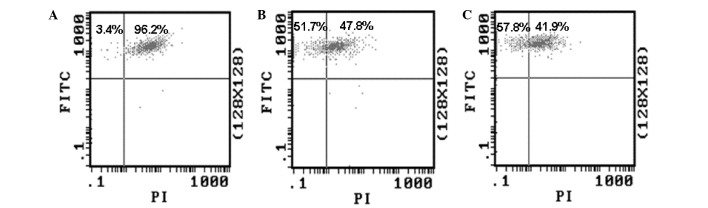
Growth inhibition of MG-63 cells by capsaicin or cisplatin
An MTT assay was used to examine the growth inhibiting effects of capsaicin and cisplatin on MG-63 cells. The result showed that capsaicin and cisplatin significantly inhibit the growth of MG-63 cells in a dose-dependent manner (Fig. 1). After 24 h treatment, the inhibition percentage was 48.5% for 200 µM capsaicin and 58.3% for 32 µg/ml cisplatin. Since these drug concentrations were close to median lethal doses (capsaicin, 165.7 µM; cisplatin, 16.76 µg/ml), these concentrations were used to treat cells in the following experiments.
Figure 1.
Growth inhibition of capsaicin and cisplatin on MG-63 cells at 24 h. (A) MG-63 cells treated with capsaicin. (B) MG-63 cells treated with cisplatin. n=4. **P<0.01 vs. control cells.
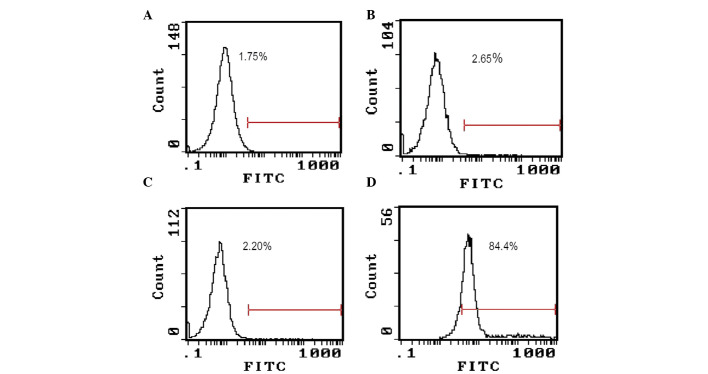
Alteration of MMP induced by capsaicin and cisplatin
Decreased MMP is a feature of apoptotic cells. In order to determine whether capsaicin and cisplatin can induce apoptosis of MG-63 cells, the effect of the drugs on the MMP was evaluated by FCM. The cells treated by 200 µM capsaicin or 32 µg/ml cisplatin were stained with DiOC6 (3), and the MMP was detected by FCM. The results showed that treatment with both drugs could decrease the ratio of cells with green fluorescence (Fig. 2). This result suggests that capsaicin and cisplatin can induce the alteration of MMP in MG-63 cells, and then initiate endogenous apoptosis.
Figure 2.
Capsaicin and cisplatin affect the mitochondrial membrane potential of MG-63 cells. (A) MG-63 cells; G-63 cells treated with (B) capsaicin and (C) cisplatin. FITC, fluorescein; PI, propidium iodide.
Effects of capsaicin and cisplatin on the expression of apoptosis-related proteins
To investigate the molecular mechanism underlying capsaicin- and cisplatin-induced apoptosis in human MG-63 OS cells, the expression levels of apoptosis-related proteins Bax and Bcl-2 were investigated using western blot analysis. As shown in Fig. 3, the expression level of Bax was markedly upregulated, and anti-apoptotic Bcl-2 was markedly downregulated, when the cells were treated with 200 µM capsaicin or 32 µg/ml cisplatin for 24 h. This suggests that Bcl-2 and Bax proteins are involved in capsaicin- and cisplatin-induced apoptosis.
Figure 3.
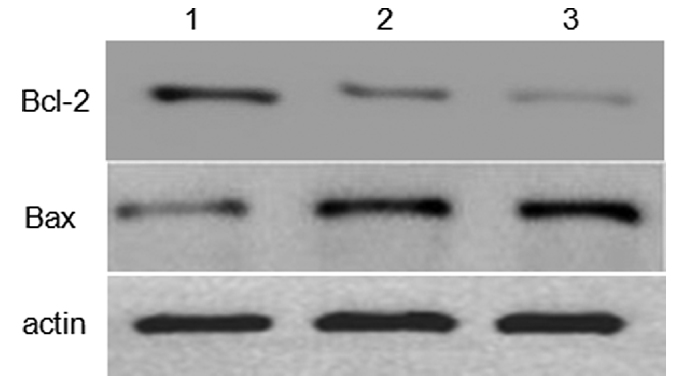
Western blot analysis was used to identify the expression of Bcl-2 and Bax in MG-63 cells. (1) MG-63 control cells; MG-63 cells treated with (2) cisplatin and (3) capsaicin. Bcl-2, B-cell lymphoma 2; Bax, Bcl-2-associated X protein.
Effect of capsaicin and cisplatin on the total expression levels of CRT in MG-63 cells
To validate whether capsaicin and cisplatin could affect CRT expression in MG-63 cells, a western blot assay was used to analyze CRT protein expression in whole cell lysates. The result showed that treating cells with capsaicin or cisplatin for 12 h did not change the total cellular CRT expression level (Fig. 4).
Figure 4.
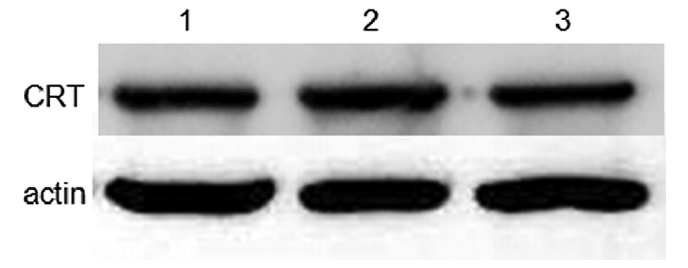
Western blot analysis was used to identify the expression of CRT in MG-63 cells. (1) MG-63 control cells; MG-63 cells treated with (2) cisplatin and (3) capsaicin. CRT, calreticulin.
Capsaicin and cisplatin promoted the translocation of CRT onto the surface of MG-63 cells
To validate whether capsaicin and cisplatin could affect CRT subcellular localization, MG-63 cells were treated with 200 µM capsaicin or 32 µg/ml cisplatin, and FCM was used to assay CRT expression on the cell surface. The result (Fig. 5) showed that capsaicin treatment for 12 h significantly increased the expression of CRT on the cell surface, but no such effect was observed when the cells were treated with cisplatin. In this experiment, MG-63 cells have been dyed with fluorescence- labeled secondary antibody alone as a control, to exclude non-specific fluorescence binding to cells (Fig. 5).
Figure 5.
Flow cytometry was used to detect the expression of calreticulin on the surface of MG-63 cells. (A) MG-63 control cells; (B) MG-63 cells without a primary antibody; MG-63 cells treated with (C) cisplatin and (D) capsaicin. FITC, fluorescein.
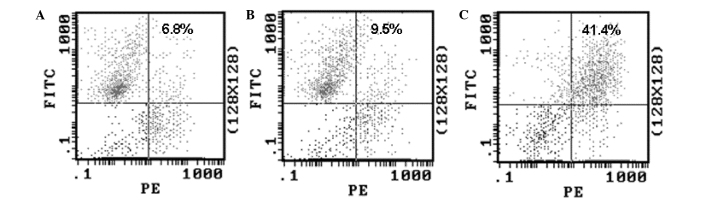
Capsaicin treatment enhanced the phagocytosis of MG-63 cells by DCs in vitro
In view of the established role of CRT as an ‘eat me’ signal, and the results from the experiments described above, the difference of phagocytotic rates among the two drug-treated MG-63 cells by DCs was investigated. The DCs (effector cells) and drug-treated MG-63 cells (target cells) were co-cultured for 2 h in a 1:1 effector/target ratio, and the phagocytotic rate was determined by FCM. The results (Fig. 6) showed that MG-63 cells treated with capsaicin were phagocytosed at a higher rate than the MG-63 cells treated with cisplatin, indicating that CRT on the cell surface enhanced the phagocytosis of the human OS cells by DCs.
Figure 6.
Treatment with capsaicin and calreticulin enhanced the phagocytosis of MG-63 cells by dendritic cells (DCs) in vitro. (A) MG-63 control cells were used as target cells; (B) Cisplatin- and (C) capsaicin-treated MG-63 cells were used as target cells. FITC, fluorescein; PI, propidium iodide.
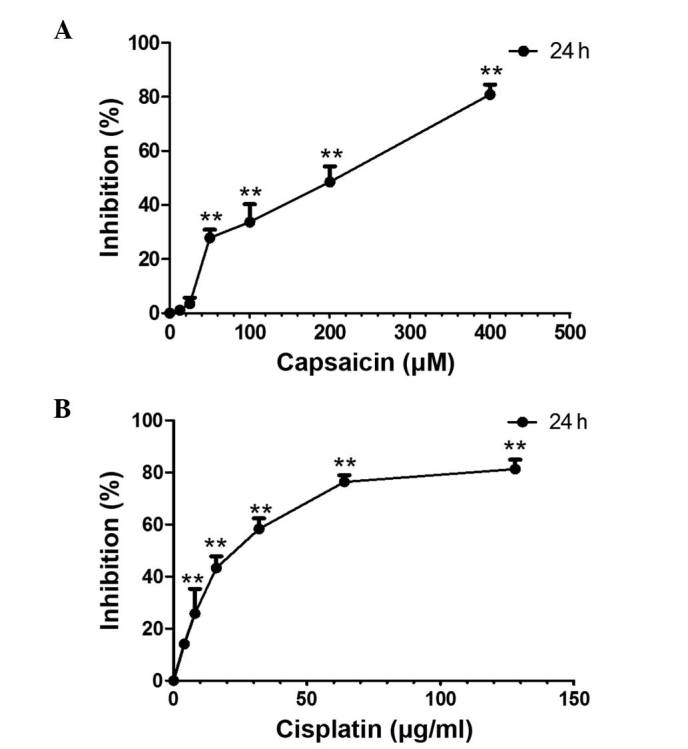
Activation of lymphocytes by DCs loaded with capsaicin-treated MG-63 cells in vitro
To investigate whether MG-63 cells with high CRT expression levels on the cell surface can induce antitumor immunity, the ability of DCs loaded with MG-63 cells to activate tumor cell-specific T-cell responses was investigated. The drug-treated MG-63 cells (target cells) were co-cultured with DCs (effector cells), then MG-63-loaded DCs were further co-cultured with lymphocytes for 24 h. The IFN-γ and IL-4 expression levels in the supernatant were then analyzed by ELISA. The result (Fig. 7) showed that, compared with MG-63 cells treated with cisplatin, capsaicin-treated MG-63 cells expressed a higher level of IFN-γ (P<0.01) in the supernatant, but no significant change was observed in the IL-4 expression level.
Figure 7.
Apoptotic MG-63 cells induced by capsaicin increased the secretion of IFN-γ by lyphocytes. ELISA was used to assay the level of (A) IFN-γ and (B) interleukin-4. **P<0.01 vs. MG-63 cells. IFN-γ, interferon-γ.
Discussion
The role of the immune system in anticancer therapy has been long neglected, as chemo- and radiotherapy-induced cell death frequently occurs through apoptosis, a cell death modality that was widely considered as immunologically silent, if not tolerogenic (14–16). In addition, cytotoxic chemotherapeutics are typically considered to be immunosuppressive (17,18). Moreover, chemotherapy- induced nausea is often treated with high dose corticoids, which also induce an unwarranted immunosuppressive side effects (19).
In recent years, increasing evidence has demonstrated that a number of chemotherapeutics can induce ICD (20). Exploring effective ways and routes that can induce ICD have already become the hot spot of tumor prevention and therapy (21).
In the process of tumor cell apoptosis induced by various physical and chemical factors, CRT within endoplasmic reticulum (ER) is rapidly translocated to the cell surface (22). In homeostatic conditions, CRT is localized to the ER, where it functions as a molecular chaperone and modulates calcium homeostasis (23). However, small quantities of CRT can be detected in other intracellular compartments, including the cytosol and nucleus (24,25).
CRT on the cell surface has numerous functions, including the modulation of cell adhesion and migration (26), and mediating the phagocytosis of apoptotic tumor cells by professional and non-professional phagocytes (11,27–29). During the process of tumor cell apoptosis induced by special stimulus, CRT is rapidly translocated from the ER to the cell surface and serves as an ‘eat me’ signal that can be recognized by phagocytes within hours after the initiation of ICD (11,28,29). Subsequently, the tumor cells undergoing apoptosis downregulate the expression of ‘do not eat me’ signals, such as surface CD47, to facilitate the recognition and engulfment of the tumor cells by phagocytes, then to induce the anticancer immune response (30).
Only a small quantity of conventional cytotoxic anticancer therapeutics can induce ICD (11,29); therefore it is clinically significant to explore novel chemicals that can induce ICD. In the current study capsaicin and cisplatin were tested for their ability to induce ICD. Human MG-63 OS cells were treated with capsaicin or cisplatin, and flow cytometry assay analysis was used to determine the changes in CRT expression levels on the cell surface. The result showed that capsaicin and cisplatin can induce apoptosis of MG-63 cells; however, only capsaicin treatment increased the expression level of CRT on the cell surface. Since the total CRT expression levels did not significantly change in MG-63 cells treated with capsaicin and cisplatin compared with the control, CRT appearing on the surface of capsaicin-treated MG-63 cells may be derived from the membrane translocation of CRT from the ER.
DCs serve important roles in processing and presenting of antigens, thus the recognition and phagocytosis of tumour cells by DCs is crucial in ICD (29). In order to evaluate the effect of capsaicin and cisplatin on the phagocytosis of MG-63 cells by DCs, the labeled MG-63 cells treated with capsaicin and cisplatin (the target cells) were co-cultured with the DCs (the effector cells), and FCM analysis was used to determine the phagocytic rate. The results showed that capsaicin-treated MG-63 cells were phagocytosed at a higher rate than MG-63 cells treated with cisplatin, indicating that CRT on the cell surface can enhance the phagocytosis of human OC cells by DCs.
Based on the above results, it can be suggested that capsaicin-treated MG-63 cells can activate lymphocytes through DCs using their phagocytosis and antigen presenting properties. To confirm this conjecture, in the current study MG-63 cells treated with capsaicin were co-cultured with DCs, and these MG-63-loaded DCs were co-cultured with lymphocytes for 24 h. The IFN-γ concentration in the supernatant was then analyzed by ELISA. The result showed that, compared with cisplatin-treated MG-63 cells, the capsaicin-treated MG-63 cells induced a higher production and release of IFN-γ from lymphocytes into the culture medium.
In conclusion, the results from the present study demonstrate that capsaicin can induce the translocation of a large quantity of CRT from intracellular compartments to the cell surface in human OS cells. In addition, CRT on the human OS cell surface can be used as specific signaling molecules to promote the phagocytosis of tumor cells, thereby mediating tumor cell immunogenic death. This may be one of the underlying molecular mechanisms of capsaicin's anti-tumor cytotoxicity. These results indicate that capsaicin can be explored as a novel drug to treat OS.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant no. 81402557).
References
- 1.Messerschmitt PJ, Garcia RM, Abdul-Karim FW, Greenfield EM, Getty PJ. Osteosarcoma. J Am Acad Orthop Surg. 2009;17:515–527. doi: 10.5435/00124635-200908000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Anderson ME. Update on Survival in Osteosarcoma. Orthop Clin North Am. 2016;47:283–292. doi: 10.1016/j.ocl.2015.08.022. [DOI] [PubMed] [Google Scholar]
- 3.Chou AJ, Geller DS, Gorlick R. Therapy for osteosarcoma: Where do we go from here? Paediatr Drugs. 2008;10:315–327. doi: 10.2165/00148581-200810050-00005. [DOI] [PubMed] [Google Scholar]
- 4.Siclari VA, Qin L. Targeting the osteosarcoma cancer stem cell. J Orthop Surg Res. 2010;5:78. doi: 10.1186/1749-799X-5-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuijjer ML, Hogendoorn PC, Cleton-Jansen AM. Genome-wide analyses on high-grade osteosarcoma: Making sense of a genomically most unstable tumor. Int J Cancer. 2013;133:2512–2521. doi: 10.1002/ijc.28124. [DOI] [PubMed] [Google Scholar]
- 6.Anninga JK, Gelderblom H, Fiocco M, Kroep JR, Taminiau AH, Hogendoorn PC, Egeler RM. Chemotherapeutic adjuvant treatment for osteosarcoma: Where do we stand? Eur J Cancer. 2011;47:2431–2445. doi: 10.1016/j.ejca.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 7.Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic cell death in cancer therapy. Annu Rev Immunol. 2013;31:51–72. doi: 10.1146/annurev-immunol-032712-100008. [DOI] [PubMed] [Google Scholar]
- 8.Krysko DV, Garg AD, Kaczmarek A, Krysko O, Agostinis P, Vandenabeele P. Immunogenic cell death and DAMPs in cancer therapy. Nat Rev Cancer. 2012;12:860–875. doi: 10.1038/nrc3380. [DOI] [PubMed] [Google Scholar]
- 9.Casares N, Pequignot MO, Tesniere A, Ghiringhelli F, Roux S, Chaput N, Schmitt E, Hamai A, Hervas-Stubbs S, Obeid M, et al. Caspase-dependent immunogenicity of doxorubicin-induced tumor cell death. J Exp Med. 2005;202:1691–1701. doi: 10.1084/jem.20050915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Obeid M, Tesniere A, Ghiringhelli F, Fimia GM, Apetoh L, Perfettini JL, Castedo M, Mignot G, Panaretakis T, Casares N, et al. Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med. 2007;13:54–61. doi: 10.1038/nm1523. [DOI] [PubMed] [Google Scholar]
- 11.Pol J, Vacchelli E, Aranda F, Castoldi F, Eggermont A, Cremer I, Sautès-Fridman C, Fucikova J, Galon J, Spisek R, et al. Trial Watch: Immunogenic cell death inducers for anticancer chemotherapy. Oncoimmunology. 2015;4:e1008866. doi: 10.1080/2162402X.2015.1008866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beltran J, Ghosh AK, Basu S. Immunotherapy of tumors with neuroimmune ligand capsaicin. J Immunol. 2007;178:3260–3264. doi: 10.4049/jimmunol.178.5.3260. [DOI] [PubMed] [Google Scholar]
- 13.D'Eliseo D, Manzi L, Velotti F. Capsaicin as an inducer of damage-associated molecular patterns (DAMPs) of immunogenic cell death (ICD) in human bladder cancer cells. Cell Stress Chaperones. 2013;18:801–808. doi: 10.1007/s12192-013-0422-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Savill J, Fadok V. Corpse clearance defines the meaning of cell death. Nature. 2000;407:784–788. doi: 10.1038/35037722. [DOI] [PubMed] [Google Scholar]
- 15.Matzinger P. The danger model: A renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 16.Kroemer G, Galluzzi L, Vandenabeele P, Abrams J, Alnemri S, Baehrecke EH, Blagosklonny MV, El-Deiry WS, Golstein P, Green DR, et al. Nomenclature Committee on Cell Death 2009: Classification of cell death: Recommendations of the Nomenclature Committee on Cell Death 2009. Cell Death Differ. 2009;16:3–11. doi: 10.1038/cdd.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zou W. Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol. 2006;6:295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 18.Zitvogel L, Apetoh L, Ghiringhelli F, André F, Tesniere A, Kroemer G. The anticancer immune response: Indispensable for therapeutic success? J Clin Invest. 2008;118:1991–2001. doi: 10.1172/JCI35180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han HS, Shim YK, Kim JE, Jeon HJ, Lim SN, Oh TK, Lee KH, Kim ST. A pilot study of adrenal suppression after dexamethasone therapy as an antiemetic in cancer patients. Support Care Cancer. 2012;20:1565–1572. doi: 10.1007/s00520-011-1248-z. [DOI] [PubMed] [Google Scholar]
- 20.Garg AD, Agostinis P. Editorial: Immunogenic Cell Death in Cancer: From Benchside Research to Bedside Reality. Front Immunol. 2016;7:110. doi: 10.3389/fimmu.2016.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song KH, Jung SY, Kang SM, Kim MH, Ahn J, Hwang SG, Lee JH, Lim DS, Nam SY, Song JY. Induction of immunogenic cell death by radiation-upregulated karyopherin alpha 2 in vitro. Eur J Cell Biol. 2016 Apr 11; doi: 10.1016/j.ejcb.2016.04.002. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 22.Fučíková J, Bartůňková J, Špíšek R. The Concept of Immunogenic Cell Death in Antitumor Immunity. Klin Onkol. 2015;4:4S48–4S55. doi: 10.14735/amko20154S48. (In Czech) [DOI] [PubMed] [Google Scholar]
- 23.Krause KH, Michalak M. Calreticulin. Cell. 1997;88:439–443. doi: 10.1016/S0092-8674(00)81884-X. [DOI] [PubMed] [Google Scholar]
- 24.Johnson S, Michalak M, Opas M, Eggleton P. The ins and outs of calreticulin: From the ER lumen to the extracellular space. Trends Cell Biol. 2001;11:122–129. doi: 10.1016/S0962-8924(01)01926-2. [DOI] [PubMed] [Google Scholar]
- 25.Bedard K, Szabo E, Michalak M, Opas M. Cellular functions of endoplasmic reticulum chaperones calreticulin, calnexin, and ERp57. Int Rev Cytol. 2005;245:91–121. doi: 10.1016/S0074-7696(05)45004-4. [DOI] [PubMed] [Google Scholar]
- 26.Gold LI, Eggleton P, Sweetwyne MT, Van Duyn LB, Greives MR, Naylor SM, Michalak M, Murphy-Ullrich JE. Calreticulin: Non-endoplasmic reticulum functions in physiology and disease. FASEB J. 2010;24:665–683. doi: 10.1096/fj.09-145482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu H, Han Y, Qin Y, Cao C, Xia Y, Liu C, Wang Y. Whole-cell vaccine coated with recombinant calreticulin enhances activation of dendritic cells and inducestumour-specific immune responses. Oncol Rep. 2013;2:529–534. doi: 10.3892/or.2012.2142. [DOI] [PubMed] [Google Scholar]
- 28.Tesniere A, Panaretakis T, Kepp O, Apetoh L, Ghiringhelli F, Zitvogel L, Kroemer G. Molecular characteristics of immunogenic cancer cell death. Cell Death Differ. 2008;1:3–12. doi: 10.1038/sj.cdd.4402269. [DOI] [PubMed] [Google Scholar]
- 29.Son KJ, Choi KR, Lee SJ, Lee H. Immunogenic Cell Death Induced by Ginsenoside Rg3: Significance in Dendritic Cell-based Anti-tumor Immunotherapy. Immune Netw. 2016;1:75–84. doi: 10.4110/in.2016.16.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chao MP, Jaiswal S, Weissman-Tsukamoto R, Alizadeh AA, Gentles AJ, Volkmer J, Weiskopf K, Willingham SB, Raveh T, Park CY, Majeti R, Weissman IL. Calreticulin is the dominant pro-phagocytic signal on multiple human cancers and is counterbalanced by CD47. Sci Transl Med. 2010;2:63ra94. doi: 10.1126/scitranslmed.3001375. [DOI] [PMC free article] [PubMed] [Google Scholar]