Abstract
Introduction
The Shanghai Aging Study is a community-based study aiming to investigate the incidence and progression of cognitive decline in Chinese elderly, with the operational procedures and diagnostic criteria similar to cohort studies in developed countries.
Methods
We prospectively evaluated 362 individuals with mild cognitive impairment (MCI) diagnosed at baseline through a clinical and neuropsychological interview. Diagnoses of dementia and MCI were made using standard criteria via consensus diagnosis.
Results
The conversion rate to dementia was 6.0 per 100 person-years, while the reversion rate to cognitive normal was 7.8 per 100 person-years. Amnestic MCI multiple domains was the most risky type for dementia (conversion rate: 14.2 per 100 person-years). Older age (hazard ratio [HR] = 1.09), apolipoprotein E (APOE ε4) (HR = 2.15), and low MMSE score (HR = 1.18) were predictors for dementia.
Discussion
Approximately 6% of elderly with MCI progress to dementia annually. Prospective studies are needed to further examine risk and protective predictors and to seek proper interventions for cognitive decline.
Keywords: Mild cognitive impairment, Progression, Dementia, Conversion, prospective study, Aging, Risk factor
1. Introduction
Mild cognitive impairment (MCI) is an intermediate state between dementia and normal cognitive aging. The definition was later expanded to include other cognitive domains, with the expectation that the initial pattern of impairment predicted various diagnostic outcomes. MCI could provide important information about the population at risk for becoming demented. It is also a stage at which intervention could be effective in reducing conversion to dementia [1], [2], [3].
Over the last 20 years, most published data of MCI progression are from Caucasians. A review of cohort studies published before 2002 estimated the annualized conversion rate at approximately 10%, whereas a lower estimate of 7% was reported in a review of selected studies published before October 2008 [4], [5]. A recent systematic review summarized published estimates for conversion from MCI or amnestic MCI (aMCI) to Alzheimer's dementia (AD) and indicated that annual conversion rates ranged from 7.5% to 16.5% per person-year for hospital-based studies and from 5.4% to 11.5% per person-year for community samples [6]. The Alzheimer's Disease Neuroimaging Initiative study reported that patients with MCI progressed to AD at a rate of 16.5% per year and regressed to normal at a rate of 8% across a 12-month period [7]. Data from the Asian population have just been reported in recent 2 years in very limited studies, including two studies in Chinese and one study in Arabic population, with the data varying between 4% and 23% of the annual conversion rate of MCI to dementia [8], [9], [10]. The substantial variation in the data of MCI progression has been considered to be due to differences in detection procedures, implementation of MCI diagnostic criteria, and demographic characteristics of the source populations. Fewer community-based studies reported the progression for MCI subtypes [11], [12], [13], [14].
China's population accounts for 21% of the world population and 1/3 of the Asian population. The number of people aged 60 years or more reached 212 million at the end of 2014, which made up 15.5% of the total population [15]. Older population in China will likely swell to 330 million or a quarter of its total population by 2050 [16]. Identifying the MCI progression in Chinese population is crucial for assessments of potential disease burden and therefore the need for interventions to prevent or slow progression of decline to dementia. Additionally, the data can be used to fill the gap of the data shortage in the Asian region.
In 2011, we established a community-based study: the Shanghai Aging Study, to investigate the prevalence, incidence, and progression of cognitive decline in Chinese elderly. Its baseline survey detected the prevalence of MCI with clinical and neuropsychological evaluations of all individuals aged 60 years or older residing in a geographically defined urban community of Shanghai [17], [18]. As its second wave, this study aimed to explore the progression and predictors of MCI and its subtypes, through a prospective follow-up in this community-based cohort.
2. Methods
2.1. Ethics statement
The present study was approved by the Medical Ethics Committee of Huashan Hospital, Fudan University, Shanghai, China. All participants or their legally acceptable representative have provided their written informed consent.
2.2. Study cohort with MCI
From January 1, 2010 through Sep 30, 2011, we conducted in-person interviews and clinical examinations for 3141 registered residents aged 60 years or older in Jingansi community in downtown Shanghai, China. We diagnosed 601 individuals with MCI among 2985 nondemented individuals and demonstrated the MCI prevalence of 20% [17]. In the later 3 months, we continued the clinical interview and diagnosed additional 54 individuals with MCI. Thus, we established a cohort with 655 individuals with MCI in the Shanghai Aging Study.
2.3. Baseline characteristics of MCI cohort
At the baseline, demographic, lifestyle characteristics, and medical histories of the participants were collected via an interviewer-administered questionnaire, consisting of the following measures: birth date, gender, education year and level, cigarette smoking, alcohol consumption, physician-diagnosed hypertension, diabetes, stroke, and heart disease. Apolipoprotein E (APOE) genotyping was conducted by the TaqMan SNP method. The presence of at least one ε4 allele was treated as being APOE ε4 positive. Detailed clinical and neuropsychological assessments and diagnosis procedures were described in the previous report of MCI prevalence [17].
2.4. Follow-up procedure
From March 1, 2014 to Sep 30, 2015, we conducted a follow-up study for this MCI cohort as the second wave of the Shanghai Aging Study. A research coordinator contacted all the individuals with MCI based on their contact information recorded at the baseline survey. Individuals were considered ineligible if they (1) were deceased; (2) had moved from the original resident place; and (3) were suffering with severe mental disorder, impairment of vision, hearing or speaking and were not able to cooperate with clinical interview and neuropsychological tests. For those eligible individuals, an appointment for a clinical interview (either at Huashan Hospital, or at their homes) was made after they agreed to participate. Participants were reminded of the evaluation by a telephone call 1 day before it was scheduled. For those deceased individuals, the cause and date of death were provided by their family members via the telephone call and confirmed by the death certificates from the Center of Disease Control.
2.5. Interview at the follow-up
At the face-to-face interview, participants were firstly asked for their cognitive complaints, which they, their proxy, or a nurse or physician indicated that they had problems with memory or thinking. Also, the time and hospital name were recorded if the individual was diagnosed as dementia by neurologists at other hospitals. Participants were measured the Lawton and Brody Activity of Daily Living (ADL) scale, to elicit physical self-maintenance and instrumental activities of daily living. Functionally intact were considered for whose ADL score was over 16 [19]. Participants who suffered with newly onset of hypertension, diabetes mellitus, stroke, and heart disease were examined and confirmed from the medical records.
Cognitive function of participants was evaluated by using the neuropsychological batteries which were used at the baseline survey. For participants with 6 or more years of formal education, the battery comprised the Mini-Mental State Examination (MMSE), Conflicting Instructions Task, Stick Test, Modified Common Objects Sorting Test, Auditory Verbal Learning Test, and Trail-making Test. For participants with <6 years of education, the battery comprised the MMSE, Conflicting Instructions Task, Stick Test, Modified Common Objects Sorting Test, modified Fuld Object Memory Evaluation, and Renminbi Test. The battery was administered in Chinese by certified study psychometrists within 90 minutes. Detailed neuropsychological tests and domains were described elsewhere [17].
2.6. Consensus diagnosis
Neurologists and neuropsychologists in our study group (D.D., Q.Z., Q.G., and Z.H.) reviewed the medical and neuropsychological data and reached a consensus regarding the presence or absence of dementia using DSM-IV criteria [20]. Only those who were not diagnosed with dementia were considered for a diagnosis of MCI, which was defined according to Petersen's criteria [21]: (1) cognitive concern or complaint by the subject, informant, nurse, or physician, with CDR = 0.5; (2) objective impairment in at least one cognitive domain based on performance 1.5 standard deviation (SD) below the mean using the norms obtained in the pilot study; (3) essentially normal functional activities (determined from the CDR and the ADL evaluations); and (4) absence of dementia (DSM-IV).
Based on cognitive test scores, participants diagnosed with MCI were placed into different groups characterizing their cognitive deficits: (1) amnestic MCI single domain (aMCI-SD: a deficit on at least 1 of the memory tests was required with no deficit in other domains); (2) amnestic MCI multiple domains (aMCI-MD: at least 1 deficit in memory plus at least 1 additional deficit in another domain was required); (3) nonamnestic MCI single domain (naMCI-SD: a deficit in verbal fluency, language, visuospatial skills, speed of mental processing, or executive function was required without a memory deficit); (4) nonamnestic MCI multiple domains (naMCI-MD: deficits in 2 or more domains other than memory were required) [3].
2.7. Statistical analysis
Continuous variables were expressed as mean and SD, and categorical variables as frequencies. The student t test or one-way analysis of variance was used for comparisons for continuous variables. The Chi-square test was used for comparisons of categorical variables.
Annual conversion rate to dementia or reversion rate to cognitive normal was calculated as the number of incident dementia or cognitive normal cases occurring during the follow-up period divided by the cumulative follow-up period of all participants and described as “per 100 person-years.” Kaplan–Meier survival analysis was used to estimate the cumulative conversion rate to dementia, or the cumulative reversion rate to cognitive normal by the follow-up period. The log-rank test was used to compare rate estimates within different subgroups.
We used the Cox proportional hazards regression model of multivariate analysis to explore the predictors for the progression from MCI to dementia or cognitive normal during the follow-up period. The covariates of multivariate analysis were age, gender, education, APOE ε4, and baseline MMSE score. The individuals remained at a risk as long as they were free from the outcome during the follow-up period. Adjusted hazard ratio (HR) along with 95% confidence interval (CI) was used as the risk or protective measurement for the outcome of dementia or cognitive normal.
All P values and 95% CIs were estimated in a two-tailed fashion. Differences were considered to be statistically significant at P < .05. Data were analyzed using SPSS 16.0 (SPSS Inc., IL).
3. Results
3.1. Baseline characteristics of study participants
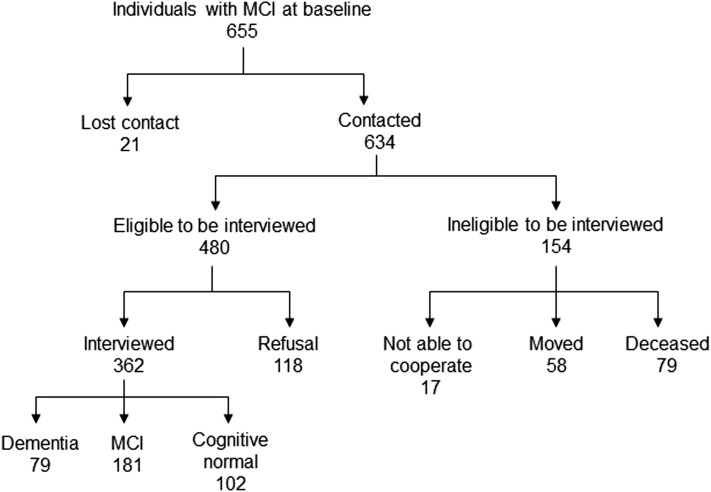
We tried to contact 655 individuals with MCI diagnosed at the baseline, and only 21 were lost contact. Despite 154 ineligible individuals (79 deceased, 58 moved, and 17 were not able to cooperate), 480 were eligible for the follow-up study. We successfully conducted the interview for 362 (75%) individuals with MCI diagnosed at the baseline (Fig. 1).
Fig. 1.
Flow chart of the follow-up study for individuals with mild cognitive impairment diagnosed at the baseline. Abbreviations: MCI, mild cognitive impairment; aMCI, amnestic mild cognitive impairment; naMCI, nonamnestic mild cognitive impairment.
The baseline characteristics of 655 individuals with MCI were showed in Table 1. Among them, 289 (44.1%) were men. Their average age was 74.9 (SD 8.5) years, and 74.8% of them had education background of middle school or above. The prevalence rates of hypertension, diabetes mellitus, stroke, and heart disease were 60.0%, 17.9%, 17.9%, and 38.6%, respectively. Smoking and drinking habits were reported in 11.8% and 7.5%, and APOE ε4 positive were found in nearly 20% individuals with MCI. At the baseline, the mean MMSE score was 26.4 (SD, 2.9). The proportions of MCI subtypes: aMCI-SD, aMCI-MD, naMCI-SD, and naMCI-MD were 41.5%, 25.2%, 24.3%, and 9.0%, respectively.
Table 1.
Baseline characteristics of individuals with MCI, interviewed and not interviewed at the follow-up
| Baseline characteristics | All individuals with MCI (n = 655) | Interviewed, (n = 362) | Not interviewed, (n = 293) | P value |
|---|---|---|---|---|
| Gender | ||||
| Women, n (%) | 366 (55.9) | 206 (56.9) | 160 (54.6) | .556 |
| Age, mean ± SD | 74.9 ± 8.5 | 74.4 ± 7.8 | 75.5 ± 9.2 | .104 |
| Education level | ||||
| Less than primary school | 52 (7.9) | 24 (6.6) | 28 (9.6) | .287 |
| Primary school | 113 (17.3) | 55 (15.2) | 58 (19.8) | |
| Middle school | 162 (24.7) | 94 (26.0) | 68 (23.2) | |
| High school | 168 (25.6) | 96 (26.5) | 72 (24.6) | |
| College and above | 160 (24.4) | 93 (25.7) | 67 (22.9) | |
| Medical history | ||||
| Hypertension, n (%) | 393 (60.0) | 214 (59.1) | 179 (61.1) | .608 |
| Diabetes mellitus, n (%) | 117 (17.9) | 60 (16.6) | 57 (19.5) | .339 |
| Stroke, n (%) | 117 (17.9) | 64 (17.7) | 53 (18.1) | .892 |
| Heart disease, n (%) | 253 (38.6) | 136 (37.6) | 117 (39.9) | .537 |
| Life habits | ||||
| Smoking, n (%) | 77 (11.8) | 41 (11.3) | 36 (12.3) | .704 |
| Drinking, n (%) | 49 (7.5) | 28 (7.7) | 21 (7.2) | .784 |
| APOE ε4 positive, n (%) | 115 (19.9)∗ | 63 (19.4)† | 52 (20.5)‡ | .759 |
| MMSE, mean ± SD | 26.4 ± 2.9 | 26.7 ± 2.8 | 26.1 ± 3.0 | .009 |
| MCI type | ||||
| aMCI-SD, n (%) | 272 (41.5) | 156 (43.1) | 116 (39.6) | .422 |
| aMCI-MD, n (%) | 165 (25.2) | 82 (22.7) | 83 (28.3) | |
| naMCI-SD, n (%) | 159 (24.3) | 91 (25.1) | 68 (23.2) | |
| naMCI-MD, n (%) | 59 (9.0) | 33 (9.1) | 26 (8.9) | |
Abbreviations: MCI, mild cognitive impairment; aMCI-SD, amnestic mild cognitive impairment single domain; aMCI-MD, amnestic mild cognitive impairment multiple domains; naMCI-SD, non-amnestic mild cognitive impairment single domain; naMCI-MD, non-amnestic mild cognitive impairment multiple domains; MMSE, mini-mental state examination; APOE, apolipoprotein.
115/578.
63/324.
52/254.
Table 1 also compared the baseline characteristics of individuals with MCI we interviewed and not interviewed (including ineligible and refusal individuals). The mean baseline MMSE score was the only characteristic with significant difference between these two groups [interviewed vs. not interviewed: 26.7 (SD 2.8) vs. 26.1 (SD 3.0), P = .009]. There was no significant difference between these two groups by gender, age, education level, medical history, life habits, APOE ε4, and MCI subtypes at the baseline.
3.2. Progression of MCI
After the average 3.6 years (1314.2 person-years) of the follow-up, we diagnosed 79 (21.8%) individuals with dementia and 102 (28.2%) individuals with cognitive normal. Half of the individuals were still keeping the status with MCI (Fig. 1).
Table 2 showed that, the conversion rate to dementia was 6.0 (95% CI: 4.7–7.3) per 100 person-years, whereas the reversion rate to cognitive normal was 7.8 (95% CI: 6.3–9.2) per 100 person-years. The highest and the second highest conversion rates were found in individuals with aMCI-MD [14.2 (95% CI: 10.2–18.2) per 100 person-years] and in individuals with naMCI-MD [8.7 (95% CI: 3.8–13.7) per 100 person-years] at the baseline. The highest and the second highest reversion rates were found in individuals with aMCI-SD [12.6 (95% CI: 9.9–15.3) per 100 person-years] and in individuals with naMCI-SD [7.3 (95% CI: 4.5–10.1) per 100 person-years] at the baseline.
Table 2.
Annual conversion rate from MCI to dementia and annual reversion rate from MCI to cognitive normal
| Type | Baseline |
Follow-up |
||||
|---|---|---|---|---|---|---|
| Dementia |
Cognitive normal |
|||||
| n | Person-years | n | Rate, per 100 person-years (95%CI) | n | Rate, per 100 person-years (95%CI) | |
| MCI | 362 | 1314.2 | 79 | 6.0 (4.7–7.3) | 102 | 7.8 (6.3–9.2) |
| aMCI | 238 | 859.7 | 59 | 6.9 (5.2–8.6) | 77 | 9.0 (7.1–10.9) |
| aMCI-SD | 156 | 564.1 | 17 | 3.0 (1.6–4.4) | 71 | 12.6 (9.9–15.3) |
| aMCI-MD | 82 | 295.6 | 42 | 14.2 (10.2–18.2) | 6 | 2.0 (0.4–3.6) |
| naMCI | 124 | 454.5 | 20 | 4.4 (2.5–6.3) | 25 | 5.5 (3.4–7.6) |
| naMCI-SD | 91 | 328.4 | 9 | 2.7 (1.0–4.5) | 24 | 7.3 (4.5–10.1) |
| naMCI-MD | 33 | 126.1 | 11 | 8.7 (3.8–13.7) | 1 | 0.8 (−0.8 to 2.3) |
Abbreviations: MCI, mild cognitive impairment; aMCI-SD, amnestic mild cognitive impairment single domain; aMCI-MD, amnestic mild cognitive impairment multiple domains; naMCI-SD, non-amnestic mild cognitive impairment single domain; naMCI-MD, non-amnestic mild cognitive impairment multiple domains.
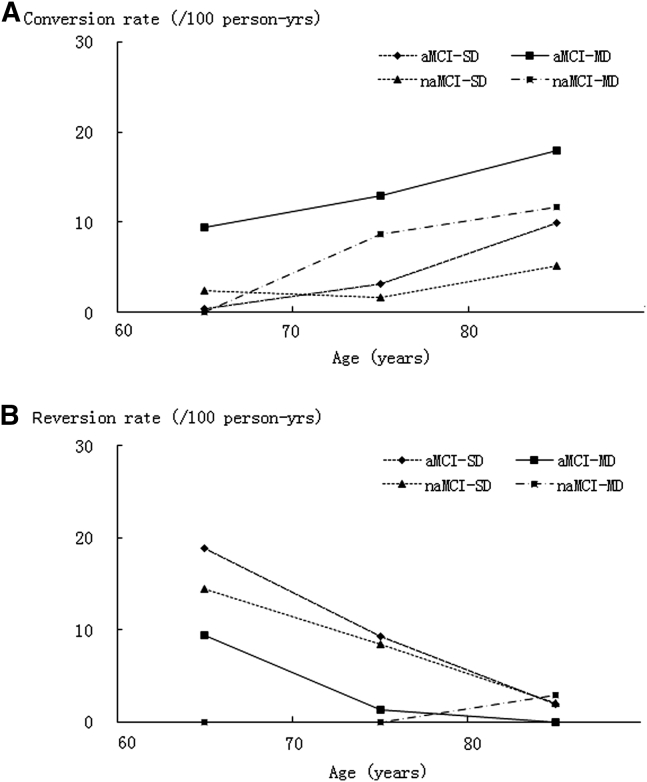
Age-specific conversion rates to dementia were showed in Fig. 2A. The increasing trend of conversion rates by increasing age were demonstrated in individuals with four different MCI subtypes, among which aMCI-MD group demonstrated the highest conversion rates, from 9.5 per 100 person-years in individuals with 60–69 years old to 18.0 per 100 person-years in individuals aged ≥80 years old. Fig. 2B showed negative correlation between the increasing age and the age-specific reversion rates to cognitive normal in individuals with 4 different MCI subtypes. The reversion rates decreased more dramatically in individuals with aMCI-SD at the baseline, from 18.9 per 100 person-years in individuals with 60–69 years old to 2.0 per 100 person-years in individuals aged ≥80 years old.
Fig. 2.
Annual conversion rate from MCI to dementia (A) and reversion rate from MCI to cognitive normal (B) in individuals with different age groups. Abbreviations: MCI, mild cognitive impairment; aMCI-SD, amnestic mild cognitive impairment single domain; aMCI-MD, amnestic mild cognitive impairment multiple domains; naMCI-SD, nonamnestic mild cognitive impairment single domain; naMCI-MD, nonamnestic mild cognitive impairment multiple domains.
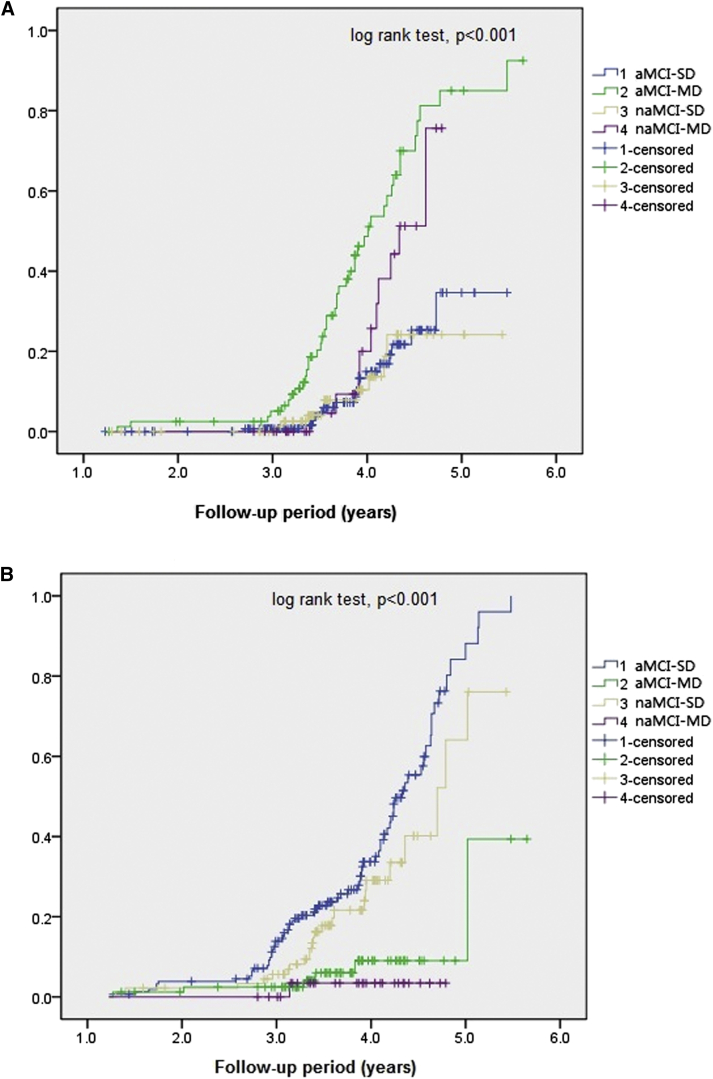
Fig. 3A showed the Kaplan-Meier curves of accumulative conversion rate to dementia in individuals with 4 MCI subtypes by follow-up time. The accumulative conversion rate of individuals with aMCI-MD increased the most dramatically, second with that of individuals with naMCI-MD, than that of individuals with other 2 MCI subtypes (Log-rank test P < .001). The accumulative reversion rate to cognitive normal of individuals with aMCI-SD increased most dramatically, second with that of individuals with naMCI-SD, than that of individuals with other 2 MCI subtypes by follow-up time (log-rank test, P < .001; Fig. 3B).
Fig. 3.
Cumulative conversion rate from MCI to dementia (A) and cumulative reversion rate from MCI to cognitive normal (B) in individuals with 4 MCI subtypes. Abbreviations: MCI, mild cognitive impairment; aMCI-SD, amnestic mild cognitive impairment single domain; aMCI-MD, amnestic mild cognitive impairment multiple domains; naMCI-SD, nonamnestic mild cognitive impairment single domain; naMCI-MD, nonamnestic mild cognitive impairment multiple domains.
3.3. Predictors of the MCI progression
Cox multivariate regression model indicated that older age (HR = 1.09, 95% CI: 1.05–1.14, P < .001) and the lower MMSE score (HR = 1.18, 95% CI: 1.06–1.28, P = .001) at baseline were the independent risk predictors to dementia. Individuals with APOE ε4 positive had more than a 2-fold greater risk of dementia than did individuals with APOE ε4 negative (HR = 2.15, 95% CI: 1.21–3.81, P = .009). Individuals with older age (HR = 0.91, 95% CI: 0.88–0.95, P < .001) and lower MMSE score (HR = 0.79, 95% CI: 0.69–0.92, P = .002) at baseline were less likely to reverse to cognitive normal (Table 3).
Table 3.
Predictors and hazard ratios for MCI progressed to dementia or cognitive normal by Cox regression model
| Dementia as the outcome |
Cognitive normal as the outcome |
|||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Gender (women) | 0.94 (0.54–1.63) | .823 | 0.75 (0.48–1.17) | .206 |
| Baseline age (increasing) | 1.09 (1.05–1.14) | <.001 | 0.91 (0.88–0.95) | <.001 |
| Education year (increasing) | 1.06 (0.99–1.13) | .090 | 1.00 (0.93–1.07) | .913 |
| Baseline MMSE (decreasing) | 1.18 (1.06–1.28) | .001 | 0.79 (0.69–0.92) | .002 |
| APOE ε4 positive | 2.15 (1.21–3.81) | .009 | 1.16 (0.67–1.98) | .602 |
Abbreviations: MCI, mild cognitive impairment; MMSE, mini-mental state examination; APOE, apolipoprotein; HR, hazard ratio.
4. Discussion
As the second wave of the Shanghai Aging Study, we clinically and neuropsychologically evaluated 362 individuals with MCI diagnosed at the baseline, after the average follow-up time of 3.6 years. The present study demonstrated that the conversion rate to dementia was 6.0 per 100 person-years, whereas the reversion rate to cognitive normal was 7.8 per 100 person-years. Individuals with aMCI-MD were the most risky ones for dementia. Older age, APOE ε4 positive, and lower MMSE score at baseline were the independent risk predictors to dementia.
Previous epidemiologic studies of MCI progression in Asia have been rarely reported. A study in Hongkong recruited 321 community-dwelling Chinese older persons aged 60 years or older with MCI. At the end of 2-year follow-up, 51 (15.9%) developed to dementia [8]. A study in Tianjin, China followed 634 participants (aged 65 years or older) with type 2 diabetes mellitus (T2DM-MCI) and 585 participants without diabetes for 5 years. The conversion rate of T2DM-MCI and MCI without diabetes to dementia were 8.43 (95% CI: 7.96–8.92) per 100 person-years and 3.86 (95% CI: 2.18–5.56) per 100 person-years [9]. Another study surveyed elderly aged 65 years or older in an Arab community in Israel. Of the 231 subjects with MCI that were re-examined after 1 year, 68 (23%) converted to dementia, including 65 AD cases [10]. These studies, however, were either with short follow-up period or with vague diagnosis based on insufficient neuropsychological tests (e.g., MMSE only). Additionally, none of these studies investigated the progression of different MCI subtypes.
The Shanghai Aging Study was an epidemiologic study conducted in China with a study design, operational procedures, and MCI diagnostic criteria similar to most cohort studies in developed countries, most of which established 20 years ago. It is also the largest study in which all participants were evaluated by comprehensive in-person assessments. The progression data of MCI and its four subtypes from the current prospective follow-up can be compared with those from existing population-based cohort studies in developed countries.
The follow-up survey of the Italian Longitudinal Study on Aging found a progression rate of 3.8 (95% CI: 2.3–6.2) per 100 person-years among 139 individuals (65 to 84 years old) with MCI at baseline, with a 3.5-year follow-up [22]. The Monongahela Valley Independent Elders Survey found 27% of 40 persons with MCI at the first assessment developed to dementia over the next 10 years. Over each 2-year interval, MCI persons showed increased risk of dementia with OR = 3.9 [23]. Different MCI subtypes likely differ in etiology and eventual outcome [21]. Studies reporting progression of MCI subtypes are still few. The Leipzig Longitudinal Study of the Aged in Germany examined a community sample of 980 dementia-free individuals aged 75 years or older. After 6 years of observation, 66 (40.2%) participants with MCI at baseline converted to dementia. The proportions of participants with aMCI-SD, aMCI-MD, naMCI-SD, and naMCI-MD at baseline who converted to dementia were 43.6%, 53.2%, 33.9%, and 21.1, respectively [11]. Among community-dwelling residents aged ≥65 years residing in Northern Manhattan, after a mean duration of follow-up of 4.7 years, the conversion rate from aMCI to AD was 7.4 (95% CI: 5.7–9.2) per 100 person-years, and from naMCI to AD was 4.1 (3.1–5.1) per 100 person-years. Participants with aMCI-MD had a higher relative risk (RR) for incident AD than those with aMCI-SD (RR = 4.3 versus 3.2) [12]. The Monongahela-Youghiogheny Healthy Aging Team study reported the 1-year outcomes of MCI among individuals aged 65 years or more. Progression to severe cognitive impairment ranged from 1.1% for naMCI-SD to 19.8% for aMCI-MD. Reversion to cognitively normal ranged from 6.3% for aMCI-MD to 53.4% for naMCI-SD [13]. The Sydney Memory and Ageing Study reported that at 2-year follow-up, 4.8% of 320 participants with baseline MCI (aged 70 to 90 years) progressed to dementia. The 2-year rate of progression from MCI at baseline to dementia was 4.8%, being highest for aMCI-MD (9.1%) [14]. Neuropsychological characterization of elderly persons without dementia provides valuable information about prognosis. Knopman et al quantitated risk of progression to dementia over the following 6 years in elderly persons without dementia from the Framingham Heart Study and Mayo Clinic Study of Aging, aged 70 to 89 years at enrollment. Baseline cognitive status was defined by performance in 4 domains derived from batteries of neuropsychological tests. Dementia risks were higher for amnestic profiles than for nonamnestic profiles and for multidomain compared with single-domain profiles [24]. Our data are consistent with those from the above-mentioned studies, indicating that memory impairments and impairments in multiple domains lead to greater progression and less improvement of cognitive function.
Previous community-based studies also reported the predictors of MCI progression, e.g., older age, shorter years of school, depression, with history of diabetes or stroke, African Americans and Hispanic, and baseline MMSE score [8], [11], [12], [13], [14], [22], [23], [24]. Other predictors were reported mostly from hospital-based studies, such as female gender [25], APOE genotype [26], white matter hyperintensities [27], lifestyle-related disease (hypertension, type II diabetes mellitus, and lipid abnormality) [28], high plasma C-reactive protein level [29], orthostatic blood pressure behavior [30], and unstable body mass index [31]. Our study explored the older age, APOE ε4 allele positive and low MMSE score at baseline, but not the gender and education years, were the independent risk predictors to dementia. We also found that participants with older age and lower MMSE score were less likely to revert to cognitive normal. Other factors may potentially impact the results but need further investigation.
There are some limitations in the present study. First, although the interviewed subjects were participants with MCI diagnosed from the original community cohort, and there were no statistically difference between interviewed and not interviewed groups for most of the baseline characteristics, the selection bias still could not be avoided. Participants without interview had lower MMSE score at the baseline and more could convert to dementia since lower MMSE score was a risk predictor for later dementia. Thus, the conversion rate in our study may be underestimated. A large part of individuals became ineligible to the follow-up study because of death and moving to nursing homes or institutions, and this also might have led to the underestimation of the conversion rate. Second, we could not distinguish subtypes of dementia because most of the dementia cases did not take the CT/MRI examination. Documented stroke history could be useful but not sufficient for the accurate diagnosis of the dementia subtype. Third, considering the related small sample size and the goodness of fit for the statistical analysis model, we could not put other factors, such as mood, chronic diseases, and life habits, as potential confounders into the multivariate Cox regression model, although these data have been collected at the baseline. Finally, results from the present study cannot be generalized to the whole Chinese population, because our study cohort has higher educational attainment than that in the general population in China (50% vs. 26%, ≥ high school) [32], and our findings may underestimate the conversion rate in China as a whole.
Currently in China, conservatively estimated based on our previous and present study results, there are at least 42,400,000 elderly aged 60 years or older living with MCI; and 2,500,000 of them progress to dementia every year, which brings the great burden to the family and society. Further prospective studies with larger sample size and longer follow-up period are urgently needed in China to examine other risk and protective predictors to seek proper interventions for cognitive decline in the increasing aging population.
Research in context.
-
1.
Systematic review: We searched PubMed for literature studies reporting the progression of mild cognitive impairment (MCI) in different ethnic populations over the last 20 years. Previous data from Chinese population can hardly be compared to those from Western studies due to differences in design, operational procedures, and diagnostic criteria.
-
2.
Interpretation: This is the first community-based prospective study conducted in China that used comparable diagnostic procedures and MCI definitions to most cohort studies in developed countries. We documented the progression of MCI and its four subtypes by clinically and neuropsychologically evaluating individuals with MCI diagnosed at the baseline.
-
3.
Future directions: Community-based prospective studies with larger sample size and longer follow-up in China are urgently needed to: (A) examine other risk and protective predictors; (B) explore the synergetic of various factors; and (C) seek proper interventions for cognitive decline in the increasing aging population.
Acknowledgments
This project was funded by the Science & Technology Committee, Shanghai, China (09DZ1950400), the National Science Foundation of China (81200835), the National 973 Project of China (2013CB530900, 2013CB530904), and the National Key Technology Project of China (2011ZX09307-001). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the article. The authors thank Zhaolan Ding, Meihua Jin, Meirong Chen, Meiling Huang, Zhiwen Shen, Yaozhen Pei, and Jianping Sun for their efforts to the study coordination and data entry, and all the participants for their cooperation.
Author contributions: This work was conceptualized by Z.H. and D.D., and all approved the protocol. Data collection was done by D.D., Q.Z., Q.G., L.Y., L.Z., and Y.Z. Statistical analysis was undertaken by D.D., X.L., and J.L. D.D., Q.Z., Q.G., and Z.H. prepared the article. Z.H. is the guarantor of this article.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Petersen R.C., Smith G.E., Waring S.C., Ivnik R.J., Tangalos E.G., Kokmen E. Mild cognitive impairment. Arch Neurol. 1999;56:303–308. doi: 10.1001/archneur.56.3.303. [DOI] [PubMed] [Google Scholar]
- 2.Petersen R.C., Stevens J.C., Ganguli M., Tangalos E.G., Cummings J.L., DeKosky S.T. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence- based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–1142. doi: 10.1212/wnl.56.9.1133. [DOI] [PubMed] [Google Scholar]
- 3.Winblad B., Palmer K., Kivipelto M., Jelic V., Fratiglioni L., Wahlund L.O. Mild cognitive impairment-beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J Intern Med. 2004;256:240–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 4.Bruscoli M., Lovestone S. Is MCI really just early dementia? A systematic review of conversion studies. Int Psychogeriatr. 2004;16:129–140. doi: 10.1017/s1041610204000092. [DOI] [PubMed] [Google Scholar]
- 5.Mitchell A.J., Shiri-Feshki M. Rate of progression of mild cognitive impairment to dementia - meta-analysis of 41 robust inception cohort studies. Acta Psychiatr Scand. 2009;119:252–265. doi: 10.1111/j.1600-0447.2008.01326.x. [DOI] [PubMed] [Google Scholar]
- 6.Ward A., Tardiff S., Dye C., Arrighi H.M. Rate of Conversion from Prodromal Alzheimer's Disease to Alzheimer's Dementia: A Systematic Review of the Literature. Dement Geriatr Cogn Dis Extra. 2013;3:320–332. doi: 10.1159/000354370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peterson R.C., Aisen P.S., Beckett L.A., Donohue M.C., Gamst A.C., Harvey D.J. Alzheimer's Disease Neruoimaging Initiative (ADNI): clinical characterization. Neurology. 2010;74:201–209. doi: 10.1212/WNL.0b013e3181cb3e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan W.C., Lam L.C., Tam C.W., Lui V.W., Leung G.T., Lee A.T. Neuropsychiatric symptoms are associated with increased risks of progression to dementia: a 2-year prospective study of 321 Chinese older persons with mild cognitive impairment. Age Ageing. 2011;40:30–35. doi: 10.1093/ageing/afq151. [DOI] [PubMed] [Google Scholar]
- 9.Ma F., Wu T., Miao R., Xiao Y., Zhang W., Huang G. Conversion of mild cognitive impairment to dementia among subjects with diabetes: a population-based study of incidence and risk factors with five years of follow-up. J Alzheimers Dis. 2015;43:1441–1449. doi: 10.3233/JAD-141566. [DOI] [PubMed] [Google Scholar]
- 10.Inselberg R., Massarwa M., Schechtman E., Strugatsky R., Farrer L.A., Friedland R.P. Estimating the risk for conversion from mild cognitive impairment to Alzheimer's disease in an elderly Arab community. J Alzheimers Dis. 2015;45:865–871. doi: 10.3233/JAD-142871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Busse A., Hensel A., Guhne U., Angermeyer M.C., Riedel-Heller S.G. Mild cognitive impairment: long-term course of four clinical subtypes. Neurology. 2006;67:2176–2185. doi: 10.1212/01.wnl.0000249117.23318.e1. [DOI] [PubMed] [Google Scholar]
- 12.Manly J.J., Tang M.X., Schupf N., Stern Y., Vonsattel J.P., Mayeux R. Frequency and course of mild cognitive impairment in a multiethnic community. Ann Neurol. 2008;63:494–506. doi: 10.1002/ana.21326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ganguli M., Snitz B.E., Saxton J.A., Chang C.H., Lee C.W., Bilt J.V. Outcomes of mild cognitive impairment by definition, a population study. Arch Neurol. 2011;68:761–767. doi: 10.1001/archneurol.2011.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brodaty H., Heffernan M., Kochan N.A., Draper B., Trollor J.N., Reppermund S. Mild cognitive impairment in a community sample: the Sydney Memory and Ageing Study. Alzheimers Dement. 2013;9:310–317. doi: 10.1016/j.jalz.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Population of over-60-yr-olds reaches 212 million. 2015. http://www.newsgd.com/news/2015-06/15/content_126401545.htm Available at: Accessed January 13, 2016. [Google Scholar]
- 16.More measures sought for aiding elderly population, China daily. 2012. http://usa.chinadaily.com.cn/china/2012-03/06/content_14763044.htm Available at: Accessed February 10, 2014. [Google Scholar]
- 17.Ding D., Zhao Q., Guo Q., Meng H., Wang B., Luo J. Prevalence of mild cognitive impairment in an urban community in China: a cross-sectional analysis of the Shanghai Aging Study. Alzheimers Dement. 2015;11:300–309. doi: 10.1016/j.jalz.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Ding D., Zhao Q., Guo Q., Meng H., Wang B., Luo J. The Shanghai Aging Study: study design, baseline characteristics, and prevalence of dementia. Neuroepidemiology. 2014;43:114–122. doi: 10.1159/000366163. [DOI] [PubMed] [Google Scholar]
- 19.Lawton M.P., Brody E.M. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 20.American Psychiatric Association . 4th ed. American Psychiatric Association; Washington: 1994. Diagnostic and Statistical Manual of Mental Disorders; pp. 143–147. [Google Scholar]
- 21.Petersen R.C. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;25:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 22.Solfrizzi V., Panza F., Colacicco A.M., D'Introno A., Capurso C., Torres F., for the Italian Longitudinal Study on Aging Working Group Vascular risk factors, incidence of MCI, and rates of progression to dementia. Neurology. 2004;63:1882–1891. doi: 10.1212/01.wnl.0000144281.38555.e3. [DOI] [PubMed] [Google Scholar]
- 23.Ganguli M., Dodge H.H., Shen C., DeKosky S.T. Mild cognitive impairment, amnestic type: an epidemiologic study. Neurology. 2004;63:115–121. doi: 10.1212/01.wnl.0000132523.27540.81. [DOI] [PubMed] [Google Scholar]
- 24.Knopman D.S., Beiser A., Machulda M.M., Fields J., Roberts R.O., Pankratz V.S. Spectrum of cognition short of dementia. Framingham Heart Study and Mayo Clinic Study of Aging. Neurology. 2015;85:1712–1721. doi: 10.1212/WNL.0000000000002100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin K.A., Choudhury K.R., Rathakrishnan B.G., Marks D.M., Petrella J.R., Doraiswamy P.M., for the Alzheimer's Disease Neuroimaging Initiative Marked gender differences in progression of mild cognitive impairment over 8 years. Alzheimers Dement. 2015;1:103–110. doi: 10.1016/j.trci.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang P.N., Lirng J.F., Lin K.N., Chang F.C., Liu H.C. Prediction of Alzheimer's disease in mild cognitive impairment: A prospective study in Taiwan. Neurobiol Aging. 2006;27:1797–1806. doi: 10.1016/j.neurobiolaging.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 27.Nolze-Charron G., Mouiha A., Duchesne S., Bocti C., for the Alzheimer's Disease Neuroimaging Initiative1 White matter hyperintensities in mild cognitive impairment and lower risk of cognitive decline. J Alzheimers Dis. 2015;46:855–862. doi: 10.3233/JAD-140618. [DOI] [PubMed] [Google Scholar]
- 28.Osone A., Arai R., Hakamada R., Shimoda K. Impact of lifestyle-related disease on conversion and reversion in patients with mild cognitive impairment: after 12 months of follow-up. Int J Geriatr Psychiatry. 2015;14:639–653. doi: 10.1002/gps.4386. [DOI] [PubMed] [Google Scholar]
- 29.Xu G., Zhou Z., Zhu W., Fan X., Liu X. Plasma C-reactive protein is related to cognitive deterioration and dementia in patients with mild cognitive impairment. J Neurol Sci. 2009;284:77–80. doi: 10.1016/j.jns.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 30.Hayakawa T., McGarrigle C.A., Coen R.F., Soraghan C.J., Foran T., Lawlor B.A. Orthostatic blood pressure behavior in people with mild cognitive impairment predicts conversion to dementia. J Am Geriatr Soc. 2015;63:1868–1873. doi: 10.1111/jgs.13596. [DOI] [PubMed] [Google Scholar]
- 31.Ye B.S., Jang E.Y., Kim S.Y., Kim E., Park S.A., Lee Y. Unstable body mass index and progression to probable Alzheimer's disease dementia in patients with amnestic mild cognitive impairment. J Alzheimers Dis. 2016;49:483–491. doi: 10.3233/JAD-150556. [DOI] [PubMed] [Google Scholar]
- 32.Comparison of population with various education attainments per 100,000 persons by region. China Statistical Yearbook 2011. Available at: http://www.stats.gov.cn/tjsj/ndsj/2011/html/D0310e.htm. Accessed February 10, 2014.