Abstract
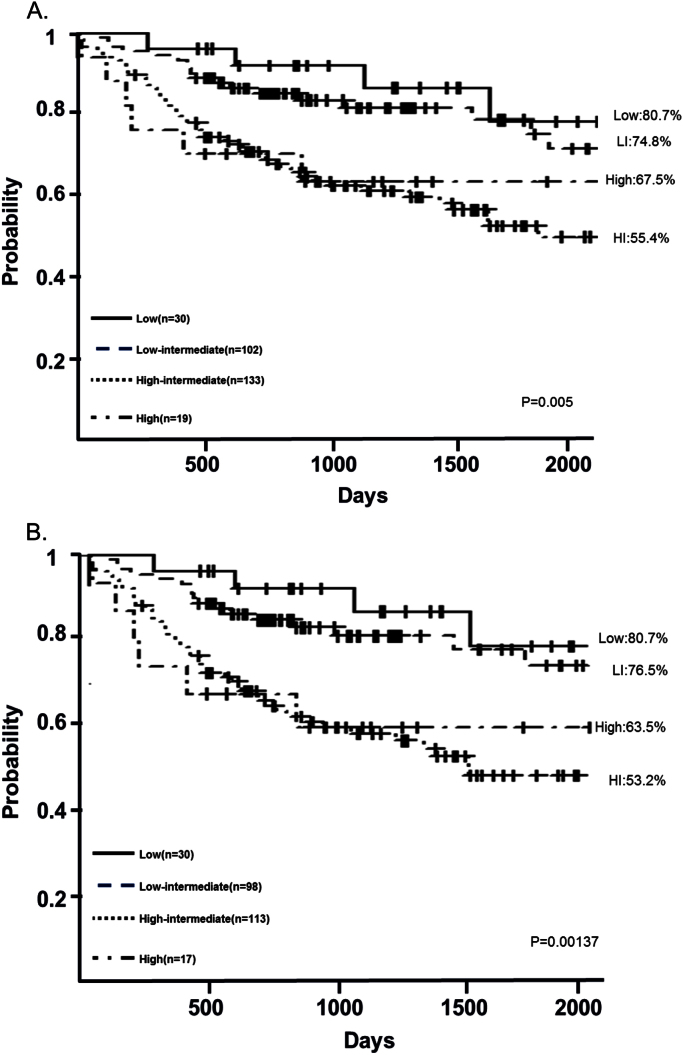
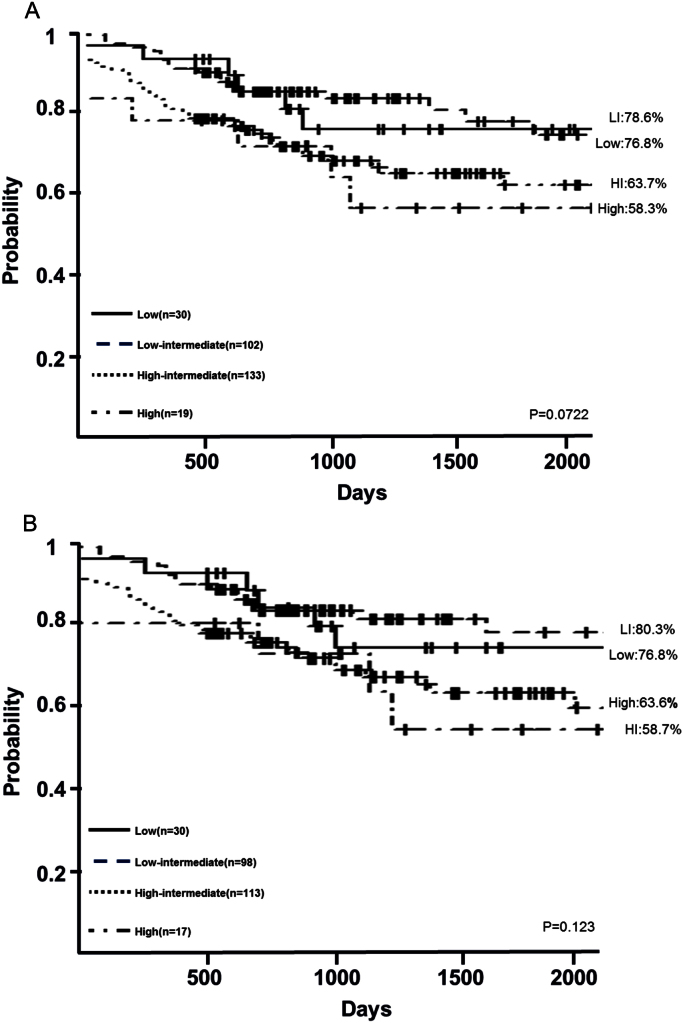
To evaluate the National Comprehensive Cancer Network (NCCN) International Prognostic Index (IPI), we analyzed 284 patients treated with the combination of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in our institution in Japan. Their 5-year overall survival (OS) by risk level was 80.7%, 74.8%, 55.4% and 67.5% (P=0.005); and their 5-year progression-free survival (PFS) was 76.8%, 78.6%, 63.7% and 58.3% (P=0.0722). The NCCN-IPI is a simple scale that uses conventional clinical factors, but did not reflect survival in our cohort. The NCCN-IPI may require further evaluation for different regions and ethnicities before adopting it for routine clinical use.
Keywords: NCCN-IPI, DLBCL, Rituximab, Albumin
Highlights
-
•
The NCCN-IPI is developed to predict survival in the rituximab era.
-
•
The NCCN-IPI failed to predict survival in our cohort.
-
•
The NCCN-IPI may require further evaluation before routine clinical use.
1. Introduction
Recently Zhou et al. developed the new National Comprehensive Cancer Network (NCCN)- International Prognostic Index (IPI) to predict survival in the rituximab era more accurately than the older IPI system [1]. Although reports that used the same prognostic stratification have since been published from various geographic regions, whether these results can be extrapolated to different ethnic populations is unclear. We therefore aimed to validate the NCCN-IPI in the presumably less selected population of Japanese patients with diffuse large B cell lymphoma (DLBCL).
2. Materials and methods
We included 284 patients who were consecutively diagnosed with DLBCL and treated with first-line rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (r-CHOP), or R-CHOP-like treatment at Kansai Medical University Hospital during 2006–2014 in this retrospective analysis. This study was approved by the Ethics Committee of Kansai Medical University. Patient survival was analyzed with the Kaplan–Meier method, and results were compared by log-rank and Cox proportional hazards models. P<0.05 was considered significant. All statistical analyses were performed using EZR (modified R software, Saitama Medical Center, Jichi Medical University, Saitama, Japan).
3. Results
Mean age of these patients was 67 years old (range: 20–91 years). The NCCN-IPI classified 11% of patients being as low risk, 36% as low-intermediate (LI), 47% as high-intermediate (HI) and 6% as high risk (Table 1). Compared to the older IPI, fewer patients were classified as low- or high-risk and more as LI and HI. The NCCN-IPI failed to identify four prognostic groups of patients in our cohort. Our patients’ 5-year overall survival (OS) rates were low-risk: 80.7%; LI: 74.8%; HI: 55.4%; and high-risk: 67.5% (P=0.005) (Fig. 1.(A)). Their 5-year progression-free survival (PFS) rates were low-risk: 76.8%; LI: 78.6%; HI: 63.7%; and high-risk: 58.3% (P=0.0722) (Fig. 2.(A)). For patients who did not receive upfront autologous hematopoietic stem cell transplantation (ASCT), the 5-year OS rates were low-risk: 80.7%; LI: 76.5%; HI: 53.2%, and high-risk: 63.5% (P=0.00137) (Fig. 1.(B)). Their 5-year PFS rates were low-risk: 76.8%; LI: 80.3%; HI: 58.7%; and high-risk: 63.6% (P=0.123) (Fig. 2.(B)).
Table 1.
Patients' characteristics.
| No. of patients (n) | 284 |
|---|---|
| Median age, range(y/o) | 67(20–91) |
| 40≧(%) | 5 |
| >40 to ≦60(%) | 23 |
| >60 to ≦75(%) | 49 |
| >75 (%) | 23 |
| Male sex (%) | 61 |
| IPI/aaIPI (%) | |
| Low | 37 |
| Low-intermediate | 16 |
| High-intermediate | 19 |
| High | 28 |
| NCCN-IPI (%) | |
| Low | 11 |
| Low-intermediate | 36 |
| High-intermediate | 47 |
| High | 6 |
| Stage(%) | |
| Ⅰ | 23 |
| Ⅱ | 14 |
| Ⅲ | 19 |
| Ⅳ | 44 |
| Elevated LDH level (%) | 48 |
| Extranodal disease >1 (%) | 40 |
| upfront ASCT(%) | 9 |
LDH: lactate dehydrogenase
ASCT: autologous hematopoietic stem cell transplantation
Fig. 1.
Five-year OS using NCCN-IPI were 80.7%, 74.8%, 55.4%, 67.5% (p=0.005) (A). Patients without upfront ASCT(B) were 80.7%, 76.5%, 53.2%, 63.5%(p=0.00137) (B). The result revealed that patients were statistically stratified into 4-risk groups, however HI was the worst prognosis.
Fig. 2.
Five-year PFS using NCCN-IPI were 78.6%, 76.8%, 63.7%, 58.3% (p=0.0722) (A). Patients without upfront ASCT(B) were 80.3%, 76.8%, 58.7%, 63.6%(p=0.123)(B).
In multivariate analysis, low albumin level (<3.5 g/dl) was an independent predictor of shorter OS, although lactate dehydrogenase (LDH), hemoglobin (Hb), C-reactive protein (CRP), age, sex, stage, extranodal involvement, and ASCT were not (Table 2).
Table 2.
Multivariate analysis.
| Parameter | HR | 95%CI | p value |
|---|---|---|---|
| LDH | 1.106 | 0.681–1.793 | 0.684 |
| Alb | 1.949 | 1.121–3.386 | 0.018 |
| Hb | 1.088 | 0.666–1.775 | 0.737 |
| CRP | 0.986 | 0.333–2.912 | 0.980 |
| Age | 1.177 | 0.712–1.947 | 0.525 |
| Sex | 1.325 | 0.828–2.119 | 0.241 |
| Stage | 1.642 | 0.866–3.109 | 0.128 |
| extra node | 1.526 | 0.910–2.557 | 0.109 |
| upfront ASCT | 0.404 | 0.151–1.073 | 0.069 |
LDH: lactate dehydrogenase
Alb: albumin
Hb: hemoglobin
CRP: C-reactive protein
ASCT: autologous hematopoietic stem cell transplantation
4. Discussion
Although the NCCN-IPI was developed to improve stratification of high-risk patients with DLBCL (i.e., whose 5-year OS<50%), it failed to detect them in our analysis; the HI group had shorter 5-year OS than the high-risk group (Fig. 1 A.).
In our institute, most eligible high-risk or HI patients were treated with upfront ASCT, which we assumed would improve their survival. When we excluded these patients from our analysis, the poorer 5-year OS for the HI group compared with the high-risk group was even more pronounced (Fig. 1 B.).
As the NCCN-IPI attaches more weight on age in the 4 risk groups, we supposed that its failure to predict outcome in this study was because our patients were older than original cohort; thus prognoses of patients whose high scores were due to age rather than tumor burden (as indicated by LDH or stage) might not be accurately predicted in the NCCN-IPI system. Some reports described results similar to ours, showing that NCCN-IPI failed to accurately predict outcomes for elderly patients [4], [7].
Aside from LDH, information about how other important parameters affect NCCN-IPI results have not been published, as far as we know. Hemoglobin [2], albumin [3], [4], and CRP [5] have been found to be independent prognostic factors in aggressive lymphoma. As these reported parameters were routinely available in our patients’ records, we analyzed their effects on OS, using multivariate analysis; however, we found only low albumin levels to be a significant predictor of worse 5-year OS. As albumin is usually assessed, quite easily and cheaply in standard blood laboratory tests, and is highly reproducible, it could be an important predictor, and be incorporated into a prognostic index.
Although the NCCN-IPI is a promising simple scale based on conventional clinical factors, its usefulness remains controversial [6], [7]. It should be evaluated in populations of different regions and ethnicities before adopting it for routine clinical use.
Conflict of interest
The authors declare no competing financial interest in relation to the work.
References
- 1.Zhou Z., Sehn L.H., Rademaker A.W., Gordon L.I., Lacasce A.S., Crosby-Thompson A. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123(6):837–842. doi: 10.1182/blood-2013-09-524108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Troppan K.T., Melchardt T., Deutsch A., Schlick K., Stojakovic T., Bullock M.D. The significance of pretreatment anemia in the era of R-IPI and NCCN-IPI prognostic risk assessment tools: a dual-center study in diffuse large B-cell lymphoma patients. Hematol. Oncol. 2015;95(6):538–544. doi: 10.1111/ejh.12529. [DOI] [PubMed] [Google Scholar]
- 3.Bairey O., Shacham-Abulafia A., Shpilberg O., Gurion R. Serum albumin level at diagnosis of diffuse large B-cell lymphoma: an important simple prognostic factor. Hematol. Oncol. 2015 doi: 10.1002/hon.2233. [DOI] [PubMed] [Google Scholar]
- 4.Melchardt T., Troppan K., Weiss L., Hufnagl C., Neureiter D., Tränkenschuh W. A modified scoring of the NCCN-IPI is more accurate in the elderly and is improved by albumin and β2 -microglobulin. Br. J. Haematol. 2015;168(2):239–245. doi: 10.1111/bjh.13116. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki K., Terui Y., Nishimura N., Mishima Y., Sakajiri S., Yokoyama M. Prognostic value of C-reactive protein, lactase dehydrogenase and anemia in recurrent or refractory aggressive lymphoma. See comment in PubMed Commons below Jpn. J. Clin. Oncol. 2013;43(1):37–44. doi: 10.1093/jjco/hys194. [DOI] [PubMed] [Google Scholar]
- 6.Huang C.E., Chen Y.Y., Lu C.H., Chen P.T., Lee K.D., Chen C.C. Validation of an enhanced International Prognostic Index (NCCN-IPI) in an Asian cohort of patients with diffuse large B cell lymphoma. Ann. Hematol. 2015;94(6):1063–1065. doi: 10.1007/s00277-014-2293-8. [DOI] [PubMed] [Google Scholar]
- 7.Yamada A., Tamura H., Asayama T., Moriya K., Okuyama N., Kondo-Onodera A. Evaluation of the enhanced International Prognostic Index (NCCN-IP)I) (for cases with diffuse large B-cell lymphoma. Rinsho Ketsueki. 2015;56(7):915–918. doi: 10.11406/rinketsu.56.915. . [Article in Japanes)e] [DOI] [PubMed] [Google Scholar]