Abstract
Background
Patients with sickle cell disease (SCD) are concerned with emergency department care, including time to treatment and staff attitudes and knowledge. Providers are concerned about rapid access to patient information and SCD treatment protocols. A software application that stores and retrieves encrypted personal medical information on a plastic credit card–sized Chart Card was designed.
Objective
To determine the applicability and feasibility of the Chart Card on patient satisfaction with emergency department care and provider accessibility to patient information and care protocols.
Methods
One-half of 44 adults (aged ~18 years) and 50 children with SCD were randomized to either the Chart Card or usual care. Patient satisfaction was surveyed pre and post implementation of the Chart Card program, and emergency department staff was surveyed about familiarity with SCD treatment protocols.
Results
Fifty-two percent of patients were female (mean age, 18.8 ± 15.6); 61% had SCD SS. Adults visited an emergency department 4.2 ± 4.0 times in the year prior to enrollment vs 2.7 ± 3.7 (p = .06) visits for children, most commonly for pain. Patient emergency department care ratings of very good or excellent increased from 47% to 66% (p < .05), and ratings of staff knowledge improved. Qualitative data reflected positive comments about patient and staff experiences with the Chart Card.
Conclusion
Patient satisfaction with emergency department care and efficacy in health care increased post Chart Card implementation. Providers valued immediate access to patient information and SCD treatment guidelines. The technology has potential for application in the treatment of other illnesses in other settings.
Keywords: sickle cell anemia, emergency care
INTRODUCTION
Sickle cell disease (SCD) is the most common genetic blood disorder in the United States with approximately 80 000 affected individuals, predominantly of African American and Hispanic descent. Patients with SCD frequently require treatment in the emergency department for acute pain episodes and life-threatening complications such as overwhelming sepsis, acute chest syndrome (ACS), and splenic sequestration.1,2 Aggressive treatment of medical emergencies has resulted in dramatically improved patient survival rates.3 Despite a focus on prevention of SCD-related complications, the need for emergency department care remains, and people with SCD may receive care from multiple providers and facilities.
There are cultural and socioeconomic barriers to optimal emergency department care for patients with SCD.4-8 Ethnic minority populations receiving emergency department care have lower rates of utilization for some procedures and higher mortality rates, even when controlling for socioeconomic factors.6,7 Although uninsured and minority patients are sometimes part of a less healthy population needing more frequent acute care,9 the reasons for differences in patient care across different demographic groups remain unclear. These disparities lead some to cite provider bias as a contributing factor. In a US survey, emergency department physicians significantly overestimated the prevalence of substance abuse,10 although research supports that less than 10% of patients with SCD meet the clinical criteria for dependence on or abuse of opioid analgesics.11,12 More recently, emergency department providers were found to have more negative attitudes towards patients with SCD presenting with vaso-occlusive episodes, compared with other providers.13 Frequent hospital admissions and prior disputes with staff were associated with the most negative attitudes. Patients with SCD encountered considerable delay in the administration of initial analgesic treatment in a multisite study of emergency department care.14 Undertreatment of pain can contribute to pseudoaddiction and seriously undermine a patient's quality of life.1 Patients with SCD with high emergency department utilization rates may actually have more severe anemia, more painful episodes, greater pain and distress ratings, and worse quality of life compared to those with lower utilization rates.15 Despite the development of national guidelines for the management of SCD pain and other complications,1,16 clinical practice and rates of acceptable care remain variable,17,18 with patients with SCD experiencing high inpatient and emergency department readmission rates.19-21
In a survey of adults and parents of children with SCD, two-thirds expressed concerns about long waiting times in the emergency department, 42% expressed concerns about staff attitudes, and 25% expressed concerns about the lack of SCD-related knowledge among emergency department staff, with overall ratings of emergency department care as poor.22 Emergency department providers expressed the need for immediate access to critical patient history.
A wallet-sized plastic card printed with essential clinical information has been recommended previously for the care of adult patients with SCD to address this need for immediate access to medical history, to improve consistency in care, and to decrease stigma associated with the need for opioid analgesics for pain management.23
In the current study, technology developed by Point Vista software was utilized to develop a wallet-sized plastic card with extensive clinical information, medical history, and treatment algorithms. The information is encrypted to ensure the security of protected health information, and the software application allows for frequent updates and easy replacement of lost cards. A card can also be printed with any information desired by the patient or their caregiver if requested. The objective of this study was to determine the feasibility of the Point Vista Chart Card program on patient and family satisfaction with emergency department care. It was hypothesized that the technology-enabling storage of extensive personal medical information and history as well as standard of care guidelines for treatment of common complications of SCD on a wallet-size credit card could be implemented in 2 distinct institutions and lead to improved patient satisfaction.
METHODS
The institutional review boards at a pediatric and a nearby community hospital in the San Francisco Bay area of California approved all study procedures. The study took place between February 2007 and March 2008.
Chart Card
The Point Vista Chart Card application suite is a hardware and software solution for sharing medical records across unaffiliated facilities. Microchip technology and associated proprietary software were developed and embedded on a plastic card the size of a credit card (Figure 1). When read by a Point Vista–authorized reader (interfaced with a PC using a USB cable), the encrypted information provides a cogent summary of the medical history, disease and symptom status, recent laboratory values, current prescriptions, and insurance information. The Chart Card chip holds 19 kilobytes of uncompressed data in a read/write format on a 32-kb microprocessor and 128 kb read/write on a 16-bit CPU microprocessor. This is equivalent to 30 single-spaced pages of uncompressed data. The personalization/repository system allows for backup of the information, dynamic upload/delete applets, format memory, patient data update, and downloading of usage logs. The Chart Cards were encrypted and only the card readers in the participating emergency departments were able to read the cards. The patient's personal information number and photographic identification positively identified patients and allow access to the database on the Chart Card.
Figure 1.
Sample Chart Card, Demonstrating Size Perspective
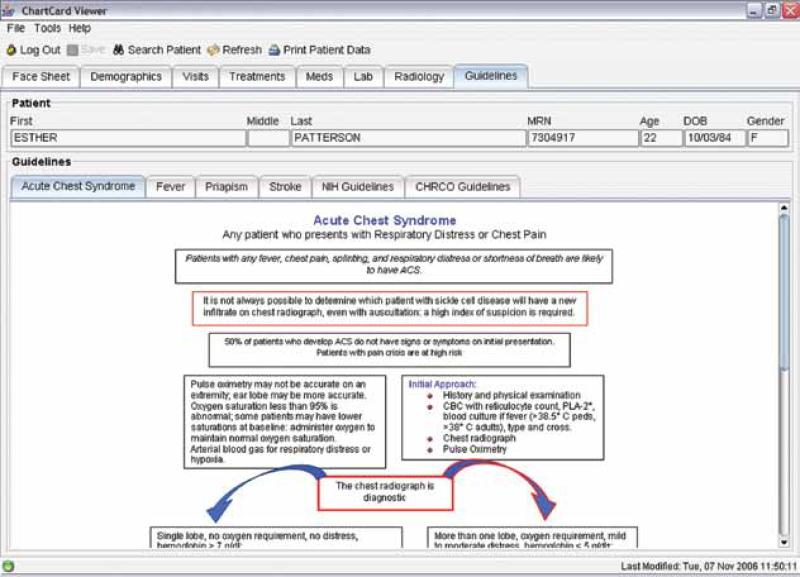
For the purposes of the study, readers were placed in the emergency department in the pediatric hospital and in the community hospital emergency department, where the adult patients were seen. Emergency department providers were surveyed regarding their familiarity with SCD standard of care guidelines and their comfort in taking care of patients with SCD. They were educated about the Chart Card technology and about standard care guidelines for management of pain, fever, and acute chest syndrome contained on the card (Figure 2). Information about the Chart Card was posted in the 2 emergency departments.
Figure 2.
Sample Standard of Care Guideline for the Treatment of Sickle Cell–Related Complications (Acute Chest Syndrome) That Can Be Accessed Using the Chart Card
Participants
Patients with any SCD diagnosis were eligible for participation; only those without a confirmed diagnosis, patients not utilizing one of the participating emergency departments for care, or those who had not had an emergency department visit in the 12 months prior to enrollment were ineligible. After informed consent, surveys were administered to adults, youth, and primary care-givers of pediatric patients in the clinic or by telephone regarding their perception and experiences of emergency room care and providers. Survey items consisted of 5-point rating scales: excellent (EX), very good (VG), good (G), fair (F), and poor (P). Patients were then randomly assigned to 1 of 2 groups—those with a Chart Card and those without—and were trained in the use of the Chart Card. After their next emergency department visit, patients were resurveyed and exited from the study. The survey was designed to evaluate the patient's experience with the program and, for those patients randomized to carry the card, to identify any barriers to use of the card in the emergency department.
Data Analyses
Demographic and baseline measures were descriptively compared using χ2 tests (with Yates continuity correction if indicated) for categorical data and Student t test for continuous variables. For comparison of patient ratings of emergency department visits prior to study entry to those at study exit, a McNemar test of correlated proportions was employed. Any comparison of the 2 treatment groups was intent-to-treat analysis and included patients in the Chart Card group that may have forgotten their card during the emergency department visit, for example.
RESULTS
Consecutive patients and their family members attending clinic were approached for enrollment. Of 107 eligible patients, 50 pediatric and 44 adults consented to participate (Table 1). The average age of the group was 18.8 years (SD, 15.6), 52% were female, and 61% had the diagnosis of SCD SS. There were no significant demographic differences between those assigned to have a Chart Card and those not assigned. The adults reported an average of 4.2 (SD, 4.0) emergency department visits in the year prior to study entry compared to 2.7 (SD, 3.8) in the pediatric patients (p = .06). Pain was a component of 70% of emergency department visits prior to study entry for adults and of 54% of visits in the pediatric group (nonsignificant).
Table 1.
Demographics of Patients With Sickle Cell Disease (SCD)
| Randomization |
|||
|---|---|---|---|
| Chart Card | No Card | Total | |
| Pediatric (<18 y) | n = 25 | n = 25 | n = 50 |
| Mean age, y (SD) | 6.6 (4.2) | 8 (5.7) | 7.3 (5.0) |
| n (%) | n (%) | n (%) | |
| Females | 10 (40) | 11 (44) | 21(42) |
| Diagnosis | |||
| SCD-SS | 16 (64) | 14 (56) | 30 (60) |
| SCD-SC | 5 (20) | 5 (20) | 10 (20) |
| SCD-Sβ0 thalassemia | 2 (8) | 1 (4) | 3 (6) |
| SCD-Sβ+ thalassemia | 2 (8) | 5 (20) | 7 (14) |
| Adult (≥18 y) | n = 23 | n = 21 | n = 44 |
| Mean age, y (SD) | 32.6 (13.1) | 31 (13.2) | 31.8 (13.0) |
| n (%) | n (%) | n (%) | |
| Females | 12 (52) | 16 (76) | 28 (64) |
| Diagnosis | |||
| SCD-SS | 16 (70) | 11 (52) | 27 (61) |
| SCD-SC | 5 (22) | 8 (38) | 13 (30) |
| SCD-Sβ0 thalassemia | 1 (4) | 0 | 1 (2) |
| SCD-Sβ+ thalassemia | 1 (4) | 2 (10) | 3 (7) |
Overall, 43 of 89 (48%) patients rated the emergency department visit occurring before study entry as excellent or very good: 63% of the pediatric group and 33% of the adults (Table 2, p = .004). There was no difference in prestudy satisfaction ratings between the patients randomized to receive the card and those without. At the time of study close, 69 of 89 (78%) had revisited the emergency department, and 47 completed a satisfaction survey (50% of patients with a Chart Card and 50% of those without). Of those who completed both the preand poststudy surveys, the proportion of patients who rated their study emergency department visit as excellent to very good increased from 47% to 66% (McNemar test, p = .05), and there were no differences between the study groups.
Table 2.
Ratings of Emergency Care Prior to Study
| Chart Card | No Card | Total | |
|---|---|---|---|
| Pediatric (<18 y) | n = 23 | n = 23 | n = 46 |
| n (%) | n (%) | n (%) | |
| Excellent | 11 (47) | 6 (26) | 17 (37) |
| Very Good | 5 (22) | 7 (30) | 12 (26) |
| Good | 5 (22) | 8 (35) | 13 (28) |
| Fair | 2 (9) | 1 (4) | 3 (7) |
| Poor | 0 | 1 (4) | 1 (2) |
| Adult (≥18 y) | n = 22 | n = 21 | n = 43 |
| n (%) | n (%) | n (%) | |
| Excellent | 2 (9) | 5 (24) | 7 (16) |
| Very Good | 4 (18) | 3 (14) | 7 (16) |
| Good | 9 (41) | 5 (24) | 14 (32) |
| Fair | 6 (27) | 7 (33) | 13 (31) |
| Poor | 1 | 1 (5) | 2 (5) |
At the start of the study, 49% of patients rated emergency department physician knowledge of SCD disease as excellent or very good: 59% of the pediatric group vs. 39% of the adults (p = .07). These proportions did not change by the end of the study. In response to the question, “What do you think could be made better with regard to you/your child's emergency department treatment?,” the majority of participants responded “Patients need to be seen more quickly.”
Sixteen pediatric and 21 community (adult) emergency department physicians completed baseline surveys regarding emergency department care of patients with SCD. More than half reported that they treated patients with SCD often or very frequently. Only 25% of pediatric and 5% of adult providers rated their familiarity with current National Institutes of Health management protocols of SCD disease as excellent or very good, but 25% of pediatric and 52% of adult providers rated their familiarity as good. Although not statistically significant, 63% of pediatric providers described their access to pain and fever protocols as excellent or very good compared to 35% of adult providers. Sixty percent rated access to individual patient information as excellent or very good and 57% were interested in Chart Card technology, with no differences between adult and pediatric emergency department providers. Only 6 of the 37 emergency department physicians returned poststudy surveys.
Patients who were randomized to the Chart Card group were interviewed about their experiences, with 25 (14 adults and 11 primary caregivers of children) of the 48 patients interviewed. Responses were overwhelmingly positive about the Chart Card, reflecting improved timeliness, communication, staff knowledge and attitudes; and increased efficacy in health care (Box). However, patients did forget to take their card to the emergency department and on several occasions, emergency department staff forgot to ask for the card.
DISCUSSION
This study demonstrated the feasibility of implementing the Chart Card program in that the software and hardware technology were successfully installed on electronic medical record systems and integrated into 2 separate non-affiliated institutions with different electronic medical record software/patient information systems and emergency department facilities. There was no difference in increased satisfaction in the group with the Chart Cards and the group without, suggesting that education about SCD provided to the emergency department physicians resulted in some improvements in their provision of care with better awareness of potential issues. Qualitative data from providers and patients suggested uniformly positive views of the Chart Card program. For providers, the cards could improve access to protocols and to specific patient medical information. Qualitatively, patients reported having a greater sense of control in their care received in the emergency department. They noted improvements in time-liness, communication, and staff knowledge and attitudes. Future studies should include objective assessment of such variables as timeliness in the provision of care24 and of any impact of the program on communication across providers and institutions.
The Chart Card could address problems of emergency department management that have been found to be rooted in emergency department registration errors,25 as encrypted individual medical record information was successfully installed on the cards. The Chart Card could also address poor communication with and lack of trust in providers that can unfortunately be a feature of sickle cell care in the emergency department, particularly for adult patients.26 Our study confirms reports of the need for better access to SCD treatment protocols and current standard of care guidelines for treatment of SCD complications.27 The Chart Card appears to be an ideal mechanism for ready access to guidelines to address problems in timely implementation of pain management from triage to effective analgesia.28 New technology allows for improvements over previous suggestions for this type of an identification card23 in that the Chart Card has the advantage of real-time updates of number of recent admissions; follow-up visits after hospitalizations, and recent acute chest syndrome (all risk factors for readmission20,21); secure protected health information; and storage of much more information, including individual treatment plans and national standards of care for treatment. Even when patients forgot to take their individual cards to their emergency department visits, the readers continued to work throughout the study and the SCD treatment protocols were accessible on the software platform on computers in both emergency departments.
Limitations
Both facilities and patients had difficulties with consistently using the Chart Cards, thus precluding meaningful comparisons of the satisfaction between the 2 study groups. In the future, strategies need to be developed to improve provider and patient adherence with a new system. Concerns with privacy that invariably arise with the use of electronic records will need to be addressed. A release of information following Health Insurance Portability and Accountability Act guidelines could indicate that the patient's presentation of the card to a health care provider suffices to confirm that the patient is allowing that provider to access the information on the card voluntarily. The patient thus remains aware of the data on the card and the data should be reviewed at clinic visits. Another limitation of the study was the difficulty in obtaining emergency department physician poststudy surveys of satisfaction with the Chart Card, with only a 16% return rate. The interest in the program and treatment algorithms was very high at the beginning of the study during initiation visits at local emergency departments. It may be that the physicians did not have the time to fill out the surveys at the end of the study and/or the novelty of the system may have proved challenging to use and so only a few of the participating emergency department physicians responded. In future applications, the software could be tailored to initially display information most likely to be utilized by emergency department physicians and algorithms that are more succinct can be created. The software described could be programmed to generate a clinical information card readable by the naked eye for those patients who would like a card in that format should they be receiving care at institutions without card readers. More emergency department in-service meetings and demonstrations of the technology would likely be beneficial.
CONCLUSIONS
The Chart Card technology holds great potential in the care of SCD and other illnesses in the emergency department and in other settings. A meta-analysis of tele-health evaluation studies showed that there is evidence for diagnostic accuracy and patient and staff satisfaction with these strategies, but there remains a need for documentation of clinical and cost effectiveness.29
Box.
Qualitative Responses—Chart Card Experience
| Timeliness | “It helped me get straight through, fast.” |
| “Very helpful, fast, accurate, and informative. Speeds up the process!” | |
| Improved communication | “Less questioning while in pain. The information was readily available.” |
| “I handed the card to the doctor and they could find out about my son's illness in a more detailed way.” | |
| “Wherever you go, they would know that you have sickle cell disease because you have the card. [I have been asked before how long] have you had sickle cell disease!” | |
| “It was a way of helping when doctors ask questions and there was something I couldn't remember.” | |
| Improved attitudes | “Sometimes I think they don't believe me that my girls have sickle cell (patients are Hispanic). If the card could tell them, that would help a lot.” |
| “Chart Card helps dispel biased notions about sickle cell disease, that they are drug users. Legitimizes you.” | |
| Improved efficacy in health care | “It helped me because he's (my) first child with sickle cell disease. I didn't always know the names of medicines that doctors needed to know. I didn't know exact antibiotic, or dose. Also, labs in the past were on the card.” |
| “[Before] I had no control, I didn't know. With the card, I knew the answers and medical history were right there.” | |
| “It made me feel safer.” | |
| “It's a plan everyone should have, just in case you're incoherent—it's there in your wallet, bam.” | |
| “I knew they had all the information...knew medicines and labs” | |
| Negative aspects of Chart Card program | “They discontinued it!” |
| “The ER staff was not always aware of what to do with it.” | |
| “I had to give up the card.” |
ACKNOWLEDGMENTS
The authors wish to acknowledge the support of Mary Rutherford, MD, Children's Hospital and Research Center Oakland Emergency Department director; William Hawk, MD, Children's Hospital and Research Center Oakland Emergency Department codirector; Steven Schrager, MD, Alta Bates Medical Center Emergency Department director; participating emergency department providers; François Orsini of Point Vista Software, LLC; the Comprehensive Sickle Cell Center staff (adult and pediatric programs) at Children's Hospital and Research Center Oakland; and participating patients and families.
Funding/Support: Funding for this study included a Small Business Innovation Research/Small Business Technology Transfer Phase II grant (2 R44 MD000552-02/5 R44 MD000552-03) from the National Center on Minority Health and Health Disparities, National Institutes of Health, to the second author.
Footnotes
Previous Presentation: A presentation based on the results of this study was given at the Third Annual Sickle Cell Disease Research and Educational Symposium and Annual Sickle Cell Disease Scientific Meeting, February 2009, Fort Lauderdale, Florida.
REFERENCES
- 1.Benjamin LJ, Dampier CD, Jacox A, et al. Guideline for the Management of Acute and Chronic Pain in Sickle Cell Disease. American Pain Society; Glenview, IL: 1999. [Google Scholar]
- 2.Wilimas JA, Flynn PM, Harris S, et al. A randomized study of outpatient treatment with ceftriaxone for selected febrile children with sickle cell disease. N Engl J Med. 1993;329:472–476. doi: 10.1056/NEJM199308123290705. [DOI] [PubMed] [Google Scholar]
- 3.Vichinsky E. Hematologic disorders in the emergency department. In: Schwartz G, editor. Principles and Practice of Emergency Medicine. Lea & Febiger; Philadelphia, PA: 1992. pp. 2019–2025. [Google Scholar]
- 4.Ruger JP, Richter CJ, Lewis LM. Association between insurance status and admission rate for patients evaluated in the emergency department. Acad Emerg Med. 2003;10:1285–1288. doi: 10.1111/j.1553-2712.2003.tb00614.x. [DOI] [PubMed] [Google Scholar]
- 5.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health. 2003;93:2067–2073. doi: 10.2105/ajph.93.12.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blanchard JC, Haywood YC, Scott C. Racial and ethnic disparities in health: an emergency medicine perspective. Acad Emerg Med. 2003;10:1289–1293. doi: 10.1111/j.1553-2712.2003.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 7.Selassie AW, McCarthy ML, Pickelsimer EE. The influence of insurance, race, and gender on emergency department disposition. Acad Emerg Med. 2003;10:1260–1270. doi: 10.1111/j.1553-2712.2003.tb00611.x. [DOI] [PubMed] [Google Scholar]
- 8.Richardson LD, Babcock Irvin C, Tamayo-Sarver JH. Racial and ethnic disparities in the clinical practice of emergency medicine. Acad Emerg Med. 2003;10:1184–1188. doi: 10.1111/j.1553-2712.2003.tb00601.x. [DOI] [PubMed] [Google Scholar]
- 9.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42:176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manag. 1997;14:168–174. doi: 10.1016/S0885-3924(97)00019-5. [DOI] [PubMed] [Google Scholar]
- 11.Elander J, Lusher J, Bevan D, Telfer P. Pain management and symptoms of substance dependence among patients with sickle cell disease. Soc Sci Med. 2003;57:1683–1696. doi: 10.1016/s0277-9536(02)00553-1. [DOI] [PubMed] [Google Scholar]
- 12.Jacob E. Pain management in sickle cell disease. Pain Manag Nurs. 2001;2:121–131. doi: 10.1053/jpmn.2001.26297. [DOI] [PubMed] [Google Scholar]
- 13.Ratanawongsa N, Haywood C, Jr, Bediako SM, et al. Health care provider attitudes toward patients with acute vaso-occlusive crisis due to sickle cell disease: development of a scale. Patient Educ Couns. 2009;76:272–278. doi: 10.1016/j.pec.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanabe P, Myers R, Zosel A, et al. Emergency department management of acute pain episodes in sickle cell disease. Acad Emerg Med. 2007;14:419–425. doi: 10.1197/j.aem.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 15.Aisiku IP, Smith WR, McClish DK, et al. Comparisons of high versus low emergency department utilizers in sickle cell disease. Ann Emerg Med. 2009;53:587–593. doi: 10.1016/j.annemergmed.2008.07.050. [DOI] [PubMed] [Google Scholar]
- 16.The Management of Sickle Cell Disease, Fourth Edition. National Institutes of Health; National Heart, Lung and Blood Institute; US Department of Health and Human Services Publication; Bethesda, MD: 2002. NIH 02-2117. [Google Scholar]
- 17.Silbergleit R, Jancis MO, McNamara RM. Management of sickle cell pain crisis in the emergency department at teaching hospitals. J Emerg Med. 1999;17:625–630. doi: 10.1016/s0736-4679(99)00050-5. [DOI] [PubMed] [Google Scholar]
- 18.Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA. 2003;290:1624–1632. doi: 10.1001/jama.290.12.1624. [DOI] [PubMed] [Google Scholar]
- 19.Frei-Jones MJ, Field JJ, DeBaun MR. Multi-modal intervention and prospective implementation of standardized sickle cell pain admission orders reduces 30-day readmission rate. Pediatr Blood Cancer. 2009;53:401–405. doi: 10.1002/pbc.22048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Frei-Jones MJ, Field JJ, DeBaun MR. Risk factors for hospital readmission within 30 days: a new quality measure for children with sickle cell disease. Pediatr Blood Cancer. 2009;52:481–485. doi: 10.1002/pbc.21854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303:1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 22.Treadwell MJ, McClough L, Quirolo K, et al. Improving emergency department care for patients with sickle cell disease.. Proceedings of the 29th Annual Meeting of the National Sickle Cell Disease Program; Memphis, TN. 2006 April 10-12; Abstract #244. [Google Scholar]
- 23.Ballas SK. Treatment of pain in adults with sickle cell disease. Am J Hematol. 1990;34:49–54. doi: 10.1002/ajh.2830340111. [DOI] [PubMed] [Google Scholar]
- 24.Zempsky WT, Loiselle KA, McKay K, Lee BH, Hagstrom JN, Schechter NL. Do children with sickle cell disease receive disparate care for pain in the emergency department? J Emerg Med. doi: 10.1016/j.jemermed.2009.06.003. doi:10.1016/j.jemermed.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 25.Hakimzada AF, Green RA, Sayan OR, Zhang J, Patel VL. The nature and occurrence of registration errors in the emergency department. Int J Med Inform. 2008;77:169–175. doi: 10.1016/j.ijmedinf.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Haywood C, Jr., Lanzkron S, Ratanawongsa N, et al. The association of provider communication with trust among adults with sickle cell disease. J Gen Intern Med. 2010;25:543–548. doi: 10.1007/s11606-009-1247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morrissey LK, Shea JO, Kalish LA, Weiner DL, Branowicki P, Heeney MM. Clinical practice guideline improves the treatment of sickle cell disease vasoocclusive pain. Pediatr Blood Cancer. 2009;52:369–372. doi: 10.1002/pbc.21847. [DOI] [PubMed] [Google Scholar]
- 28.Tanabe P, Artz N, Mark Courtney D, et al. Adult emergency department patients with sickle cell pain crisis: a learning collaborative model to improve analgesic management. Acad Emerg Med. 2010;17:399–407. doi: 10.1111/j.1553-2712.2010.00693.x. [DOI] [PubMed] [Google Scholar]
- 29.Aoki N, Dunn K, Johnson-Throop KA, Turley JP. Outcomes and methods in telemedicine evaluation. Telemed J E Health. 2003;9:393–401. doi: 10.1089/153056203772744734. [DOI] [PubMed] [Google Scholar]