Abstract
Purpose
Up to 71% of South Korean postmenopausal women have vitamin D deficiency {serum 25-hydroxyvitamin D [25(OH) D] level <50 nmol/L}. Data on vitamin D supplementation was collected during the screening phase of an efficacy/safety study of denosumab in Korean postmenopausal women with osteoporosis. This report describes the effect of vitamin D supplementation on repletion to 25(OH)D levels ≥50 nmol/L in Korean postmenopausal women with osteoporosis.
Materials and Methods
Vitamin D levels of Korean postmenopausal women (60–90 years old) were measured by extracting 25(OH)D2 and 25(OH)D3 from serum samples via protein precipitation and using liquid chromatography with tandem mass spectrometry detection. Calibration curves were constructed from the mass chromatograms to obtain total vitamin D levels. Subjects with serum 25(OH)D levels <50 nmol/L were supplemented with 1000 IU of vitamin D tablets during the 2.5-month-long screening period. Dose, frequency, and duration were determined by the investigator. If repletion was achieved (≥50 nmol/L) on retest, subjects were eligible to be rescreened for study entry.
Results
Of 371 subjects screened, 191 (52%) required vitamin D supplementation, and 88% (168 of 191) were successfully repleted. More than half of the subjects (58%) who were successfully repleted received doses of 2000 IU daily. The mean time to successful repletion was 31 days (standard deviation 8.4 days; range 11–48 days).
Conclusion
Supplementation with daily median doses of 2000 IU vitamin D successfully repleted 88% of Korean postmenopausal women with osteoporosis within 48 days to a serum vitamin D level of 50 nmol/L.
Keywords: Vitamin D, postmenopause, osteoporosis, Korean
INTRODUCTION
Adequate vitamin D levels are important in the prevention of fractures in patients with osteoporosis. Treatment guidelines on the management of postmenopausal osteoporosis recommend maintaining adequate vitamin D intake to prevent bone loss.1 Vitamin D deficiency impairs bone mineralization and calcium absorption, as well as muscle strength and balance, which may consequently increase the risk of falling. In a Women's Health Initiative trial, postmenopausal women receiving calcium and vitamin D supplementation had a lower risk of hip fracture [hazard ratio, 0.62; 95% confidence interval (CI), 0.38–1.00] than those receiving placebo.2 Similarly, a meta-analysis reported that vitamin D supplementation (≥800 IU daily) compared with placebo or calcium alone in patients ages 65 years or older reduces hip fracture risk by 30% (hazard ratio, 0.70; 95% CI, 0.58–0.86) and nonvertebral fracture risk by 14% (hazard ratio, 0.86; 95% CI, 0.76–0.96).3
Data from the 2008–2009 Korea National Health and Nutrition Examination Survey (KNHANES) demonstrated that osteoporosis risk decreases with increased serum levels of 25-hydroxyvitamin D [25(OH)D].4 An evaluation of multinational postmenopausal women (n=2606) with osteoporosis revealed that South Korea had the lowest mean serum 25(OH)D level (44 nmol/L) out of 18 countries studied (from Europe, the Middle East, Asia, Latin America, and Australia).5 The prevalence of vitamin D inadequacy, defined as a serum 25(OH)D level of <75 nmol/L, in South Korean postmenopausal women was 92%. With a lower cutoff value of 50 nmol/L, vitamin D inadequacy was 64%. KNHANES data from 2008 indicated that 64.5% of females aged 10 years or older had vitamin D insufficiency, and only 6.7% had a serum 25(OH)D level of >75 nmol/L.6
Korean postmenopausal women with osteoporosis have high rates of vitamin D deficiency and may need increased doses of vitamin D to restore adequate blood 25(OH)D levels. A phase III, randomized, double-blind, placebo-controlled, parallel-group, multicenter study (ClinicalTrials.gov identifier: NCT01457950; study number: DPH114163) was conducted to evaluate the efficacy and safety of denosumab in Korean postmenopausal women with osteoporosis.7 Subjects with vitamin D deficiency, defined as a serum 25(OH)D level of <50 nmol/L in this study, underwent repletion during the screening phase prior to study entry. This is a descriptive report of the effect of vitamin D supplementation on repletion to 25(OH)D levels of ≥50 nmol/L in Korean postmenopausal women with osteoporosis, according to the standard of care in Korea.
MATERIALS AND METHODS
The methods of the efficacy and safety study in Korean postmenopausal women have been described previously.7
Data on vitamin D repletion were collected during the screening phase of the efficacy and safety study. To be eligible for the study, subjects needed a serum 25(OH)D level of ≥50 nmol/L. Korean postmenopausal women (60–90 years old) with vitamin D deficiency at screening received supplemental vitamin D (Nature's Plus® Vitamin D 1000 IU, Natural Organics, Inc., Melville, NY, USA) tablets. Dose, frequency, and duration were determined by the investigator. A maximum of 75 days was allowed for the screening period, which included time allowed for vitamin D repletion.
Both 25(OH)D2 and 25(OH)D3 were extracted from serum samples via protein precipitation and measured via liquid chromatography with tandem mass spectrometry (LC-MS/MS) detection (Thermo Finnigan TSQ Quantum Ultra MS/MS System with PC, Thermo Fisher Scientific, Waltham, MA, USA). All assays met reproducibility requirements of ≤20% coefficient of variation (CV) and were acceptable for clinical use. Intra-assay CVs were 6.7–12.5% for 25(OH)D2 and 4.4–13.7% for 25(OH)D3, and inter-assay CVs were 10.9–16.9% for 25(OH)D2 and 9.1–15.4% for 25(OH)D3. Total vitamin D levels were quantitated using calibration curves constructed from the mass chromatograms.
After vitamin D supplementation, a second blood sample was obtained and tested. If repletion was successful (≥50 nmol/L) on retest, subjects were eligible to be rescreened for study entry.
RESULTS
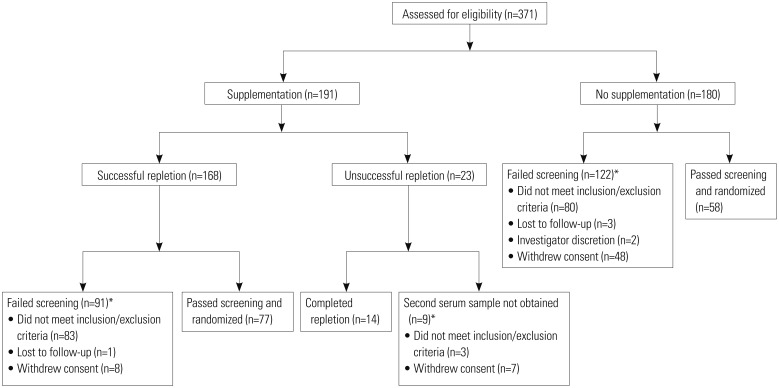
More than 50% (191 of 371) of all subjects assessed for eligibility required vitamin D supplementation. Of the 191 subjects who underwent vitamin D supplementation, 168 (88%) were successfully repleted. Among the remaining 23 subjects, 14 were repletion-complete, meaning that they did not achieve adequate vitamin D levels (≥50 nmol/L), and a second serum sample was not obtained in 9; thus, these subjects were excluded from study entry. Those with sufficient vitamin D levels (≥50 nmol/L) who met all other study eligibility criteria were randomized (n=135) (Fig. 1). Of these 135 randomized subjects, 58 (43%) had adequate vitamin D levels, and 77 (57%) received vitamin D supplementation therapy and achieved adequate vitamin D levels.
Fig. 1. Subject flow of vitamin D supplementation in Korean study. A total of 135 patients met eligibility criteria and were randomized. *Subjects may have had more than 1 reason for screen failure.
Mean age, albumin-corrected calcium, and years since menopause were similar between randomized subjects not requiring vitamin D supplementation and those who were successfully repleted (Table 1). The median dose administered during supplementation was 2000 IU vitamin D (range 1000–9000 IU) (Table 1). Most subjects (58%) who were successfully repleted received doses of 2000 IU daily (Table 2). Table 2 also shows the repletion rates at different doses of vitamin D used. The mean time to successful repletion was 31 days (standard deviation 8.4 days; range 11–48 days) (Fig. 2). Mean vitamin D levels after successful repletion were 71.4 nmol/L in randomized subjects and 70.4 nmol/L in non-randomized subjects, compared with 71.3 nmol/L in randomized subjects who did not require vitamin D supplementation at screening (Table 3).
Table 1. Demography of 135 Randomized Subjects Who Did or Did Not Receive Vitamin D Supplementation.
| Parameter | Randomized subjects not requiring supplementation (n=58)* | Randomized subjects who were Parameter successfully repleted (n=77) |
|---|---|---|
| Age (yr) | ||
| n | 58 | 77 |
| Mean (SD) | 65.9 (4.88) | 66.9 (4.78) |
| Albumin-corrected calcium (mmol/L) | ||
| n | 58 | 77 |
| Mean (SD) | 2.33 (0.083) | 2.32 (0.073) |
| Years since menopause | ||
| n | 58 | 77 |
| Mean (SD) | 17.5 (6.51) | 18.9 (6.74) |
| Daily vitamin D dose (IU) during repletion | ||
| n | NA | 76 |
| Mean (SD) | NA | 1761.9 (961.46) |
| Median (range) | NA | 2000 (1000–9000) |
NA, not applicable; SD, standard deviation.
*58 patients did not require vitamin D supplementation to achieve repletion during the study.
Table 2. Average Daily Vitamin D Supplemental Dose in Successfully and Unsuccessfully Repleted Subjects*.
| Average daily dose (IU) | Successful repletion population, n (%) | Unsuccessful repletion population, n (%) | ||||
|---|---|---|---|---|---|---|
| Randomized (n=77)† | Non-randomized (n=91) | Total (n=168) | Repletion complete (n=14) | Repletion not complete (n=9)† | Total (n=23) | |
| 1000 | 24 (31) | 41 (45) | 65 (39) | 3 (21) | 2 (22) | 5 (22) |
| >1000 to <2000 | 2 (3) | 1 (1) | 3 (2) | 1 (7) | 0 (0) | 1 (4) |
| 2000 | 49 (64) | 48 (53) | 97 (58) | 10 (71) | 4 (44) | 14 (61) |
| 4000 to 9000 | 1 (1) | 1 (1) | 2 (1) | 0 (0) | 0 (0) | 0 (0) |
*One subject in the non-repleted population received 2000 IU of vitamin D, †Data are missing for one randomized successfully repleted subject and three unsuccessfully repleted subjects who did not complete repletion.
Fig. 2. Time to achieve successful vitamin D repletion in Korean study. Of the 191 patients who entered the trial, 168 were fully repleted, and in 23, repletion to the goal of ≥50 nmol/L was not achieved.
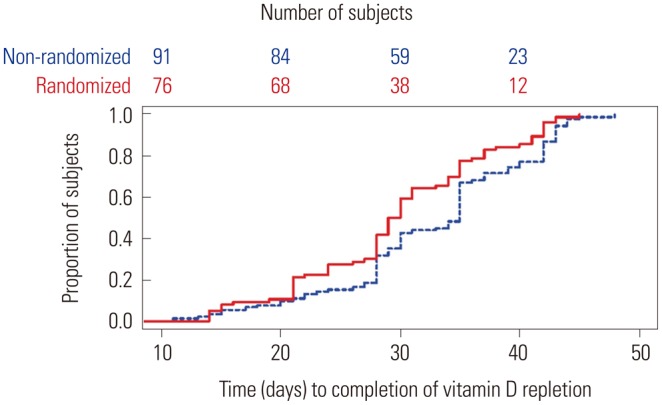
Table 3. Vitamin D Levels (nmol/L) Pre- and Post-Repletion in Screening Phase.
| Time point | Subjects not requiring supplementation | Successful repletion population | ||
|---|---|---|---|---|
| Randomized (n=58) | Non-randomized (n=122) | Randomized (n=77) | Non-randomized (n=91) | |
| Initial screening | ||||
| n | 58 | 115* | 77 | 90* |
| Mean (SD) | 71.3 (15.00) | 52.6 (22.91) | 29.7 (9.73) | 29.4 (10.56) |
| Median (range) | 70 (50–118) | 53 (10–103) | 30 (13–48) | 30 (10–62) |
| Post-repletion assessment | ||||
| n | NA | NA | 77 | 91 |
| Mean (SD) | NA | NA | 71.4 (13.18) | 70.4 (13.32) |
| Median (range) | NA | NA | 70 (50–103) | 68 (50–113) |
NA, not available; SD, standard deviation.
*Vitamin D levels at initial screening were not available for seven non-randomized subjects not requiring repletion and one non-randomized subject who was successfully repleted.
Non-serious adverse events were not collected during the screening phase of the study, and no serious adverse events were reported during this phase.
DISCUSSION
For postmenopausal women with osteoporosis, pharmacologic therapy must be accompanied by appropriate lifestyle changes, including ensuring vitamin D adequacy.1 Vitamin D levels, along with many other factors such as general nutrition, exercise, and smoking, affect the rate of bone loss and fracture risk. In this study, daily median supplemental doses of 2000 IU vitamin D successfully repleted 88% of Korean postmenopausal women with osteoporosis within 11 to 48 days to a serum vitamin D level of 50 nmol/L.
Many regimens of vitamin D are currently used in clinical practice to treat patients with low serum levels of vitamin D and may depend on the individual patient as well as any underlying conditions. Patients from the Atlanta Veterans Affairs Medical Center, a majority of whom were male, received vitamin D prescriptions for osteoporosis, chronic kidney disease, and myalgias.8 The regimens ranged from 400 IU to 40000 IU at a frequency of twice daily to once monthly, as there was no universal standard regimen. In the University of Colorado Hospital outpatient clinical system, patients (83.2% female, 44.3% Caucasian) without chronic conditions other than vitamin D deficiency were treated with 50000 to 100000 IU vitamin D weekly for several weeks to replete serum levels.9 The American Association of Clinical Endocrinologists medical guidelines for the management of postmenopausal osteoporosis state that many experts recommend 1000 to 2000 IU vitamin D daily for adults 50 years or older, and certain individuals may require more supplementation to achieve the currently accepted minimum 25(OH)D level of 75 nmol/L.1
These data are pertinent to this trial and patient population, and it should not be assumed that 2000 IU of vitamin D over the time period seen in this trial will provide successful repletion in other patient populations or in postmenopausal women with osteoporosis and different baseline characteristics. It does, however, provide a starting point for the dosing of vitamin D for a good portion of Korean postmenopausal women with osteoporosis and similar characteristics. Doses of 1000 to 2000 IU in the majority of subjects in this study were sufficient to reach the predefined level of 50 nmol/L within the screening period of 75 days. This observation supports the hypothesis that vitamin D repletion to the goal levels in Korean postmenopausal women with osteoporosis can be achieved with doses lower than those used in the studies above, which were conducted in the United States. Vitamin D repletion was not successful in 7.3% (14 of 191) of subjects who received daily oral supplementation of 2000 IU vitamin D during the screening phase for up to 75 days. This suggests that some Korean postmenopausal women with osteoporosis may need doses higher than 2000 IU of plain vitamin D to achieve adequate serum 25(OH) D levels.
Consistent with previous findings, there is a high prevalence of severe vitamin D deficiency in Korean postmenopausal women with osteoporosis. In our study, 51% of subjects screened required vitamin D supplementation to achieve the threshold of 50 nmol/L. This proportion is consistent with results from other studies in Korean postmenopausal women that reported vitamin D inadequacy rates of up to 64% using a 50-nmol/L cut-off value.5
It would be useful to fully understand why some patients were successfully repleted within the study timeline while others were not. We can only speculate on the reasons as to why this occurred. One possible reason was the lack of patient compli ance. If the patient had an unknown gastrointestinal disease that affected absorption, this could have been another reason (patients with known malabsorption were excluded from participation in the trial). Other reasons could have included not enough time for repletion if there was either a delay in the administration of vitamin D or a delay in obtaining the initial laboratory results that indicated repletion was necessary for enrollment.
In the pivotal Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Months (FREEDOM) study that investigated the efficacy and safety of denosumab in a multinational population, vitamin D repletion was also required prior to study entry.10 Both studies (Korean and FREEDOM) required subjects to receive ≥400 IU vitamin D daily and ≥1000 mg calcium throughout the study. Compared to the 50-nmol/L minimum vitamin D threshold for the Korean study, a lower minimum vitamin D threshold was used in the FREEDOM study. Subjects with vitamin D levels of 30–50 nmol/L could be enrolled on the condition that they receive a higher dose of vitamin D (800 IU daily) during the study. Subjects with vitamin D levels of <30 nmol/L failed screening yet could be repleted and rescreened. This difference reflected an update in guidelines, which occurred after the FREEDOM study was designed and defined vitamin D deficiency as a 25(OH)D level of <50 nmol/L.11
These findings provide insight on vitamin D repletion in Korean postmenopausal women; however, the limitations of this study must be considered. This was not a controlled study of vitamin D repletion, as data provided from the screening phase of a randomized study are observational in nature. Data were limited for subjects who failed initial screening, and reasons for failure to achieve vitamin D repletion were not collected. Investigators were instructed to use vitamin D supplementation as per the local standard of care; thus, doses may have varied between study sites.
These data confirm that supplemental daily doses of 1000 to 2000 IU of vitamin D during a screening period of 75 days are effective in repleting serum 25(OH)D levels to ≥50 nmol/L in the majority of Korean subjects with postmenopausal osteoporosis.
ACKNOWLEDGEMENTS
The authors would like to thank all investigators, Chan-Soo Shin, Sung-Kil Lim, Jung-Min Koh, Dong Jin Chung, Yoon-Sok Chung, Moo-Il Kang, In-Ju Kim, Yong-Ki Min, Han-Jin Oh, and Il Hyung Park, for their work conducting the study and interacting with the patients, and acknowledge Han-Kyu Lee, MD, MS, for his review and assistance with this manuscript.
Footnotes
This study was presented as a poster at the 2013 Annual Meeting of the American Society for Bone and Mineral Research in Baltimore, Maryland on October 7, 2013.
Funding: This study was sponsored by GlaxoSmithKline. GlaxoSmithKline was involved in the study design; in the collection, analysis analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication. Grace H. Lee, PharmD and John Romankiewicz, PharmD, of Scientific Therapeutics Information, Inc., Madison, New Jersey, provided editorial assistance, which was funded by Glaxo-SmithKline.
Disclosure statement and conflicts of interest: Jung-Min Koh, Dong Jin Chung, Yoon-Sok Chung, Moo-Il Kang, In-Ju Kim, Yong-Ki Min, Han-Jin Oh, and Il Hyung Park declare no financial conflict of interest. Yil-Seob Lee, Barbara Kravitz, Brian Waterhouse, Antonio Nino, and Lorraine A. Fitzpatrick are employees of GlaxoSmithKline and receive stock and stock options in the company.
The authors have no financial conflicts of interest.
References
- 1.Watts NB, Bilezikian JP, Camacho PM, Greenspan SL, Harris ST, Hodgson SF, et al. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of postmenopausal osteoporosis. Endocr Pract. 2010;16(Suppl 3):1–37. doi: 10.4158/ep.16.s3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prentice RL, Pettinger MB, Jackson RD, Wactawski-Wende J, Lacroix AZ, Anderson GL, et al. Health risks and benefits from calcium and vitamin D supplementation: Women's Health Initiative clinical trial and cohort study. Osteoporos Int. 2013;24:567–580. doi: 10.1007/s00198-012-2224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367:40–49. doi: 10.1056/NEJMoa1109617. [DOI] [PubMed] [Google Scholar]
- 4.Hong H, Kim EK, Lee JS. Effects of calcium intake, milk and dairy product intake, and blood vitamin D level on osteoporosis risk in Korean adults: analysis of the 2008 and 2009 Korea National Health and Nutrition Examination Survey. Nutr Res Pract. 2013;7:409–417. doi: 10.4162/nrp.2013.7.5.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lips P, Hosking D, Lippuner K, Norquist JM, Wehren L, Maalouf G, et al. The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med. 2006;260:245–254. doi: 10.1111/j.1365-2796.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- 6.Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea--a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab. 2011;96:643–651. doi: 10.1210/jc.2010-2133. [DOI] [PubMed] [Google Scholar]
- 7.Koh JM, Oh HJ, Park IH, Kim IJ, Kang MI, Lim SK, et al. Efficacy and safety results from a six month double-blind study comparing 60 mg denosumab (DMAb) and placebo in Korean postmenopausal women with osteoporosis. [accessed on 2014 January 6];J Bone Miner Res. 2013 28(Suppl 1) Available at: http://www.asbmr.org/asbmr-2013-abstract-detail?aid=f2f88d4e-888b-4ef4-b170-4244d1d6d02c. [Google Scholar]
- 8.Pepper KJ, Judd SE, Nanes MS, Tangpricha V. Evaluation of vitamin D repletion regimens to correct vitamin D status in adults. Endocr Pract. 2009;15:95–103. doi: 10.4158/EP.15.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vande Griend JP, McQueen RB, Linnebur SA, Vondracek SF. Prescription ergocalciferol dosing for vitamin D repletion: a retrospective evaluation. Pharmacotherapy. 2012;32:135–141. doi: 10.1002/PHAR.1052. [DOI] [PubMed] [Google Scholar]
- 10.Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 11.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]