Abstract
In this study, we evaluated national differences in emergency department (ED) crowding to identify factors significantly associated with crowding in institutes and communities across Korea. This was a cross-sectional nationwide observational study using data abstracted from the National Emergency Department Information System (NEDIS). We calculated mean occupancy rates to quantify ED crowding status and divided EDs into three groups according to their occupancy rates (cutoffs: 0.5 and 1.0). Factors potentially related to ED crowding were collected from the NEDIS. We performed a multivariate regression analysis to identify variables significantly associated with ED crowding. A total of 120 EDs were included in the final analysis. Of these, 73 were categorized as 'low crowded' (LC, occupancy rate < 0.50), 37 as 'middle crowded' (MC, 0.50 ≤ occupancy rate < 1.00), 10 EDs as 'high crowded' (HC, 1.00 ≤ occupancy rate). The mean ED occupancy rate varied widely, from 0.06 to 2.33. The median value was 0.39 with interquartile ranges (IQRs) from 0.20 to 0.71. Multivariate analysis revealed that after adjustment, ED crowding was significantly associated with the number of visits, percentage of patients referred, number of nurses, and ED disposition. This nationwide study observed significant variety in ED crowding. Several input, throughput, and output factors were associated with crowding.
Keywords: Emergency Service, Hospital, Crowding, National Health Program
Graphical Abstract
INTRODUCTION
Emergency Department (ED) crowding has become a major public health concern (1,2,3). It is defined as the state when demand for acute care overwhelms the capacity of an emergency department, which attenuates the quality of emergency care, resulting in deterioration of timeliness, efficiency, effectiveness, equitability, safety, and patient-centeredness (4,5,6,7). The problem is not limited to North America, but has been an increasingly major global issue (8,9,10,11).
The major cause of crowding is, as defined by the American College of Emergency Physicians, the need for emergency services that exceeds limited ED resources (12,13,14). Various studies have identified factors significantly associated with ED crowding, including academic status, proportion of uninsured patients, longer wait time, and distribution of patient socioeconomic status (15,16,17,18). However, to our knowledge, no studies have described crowding status nationwide, and little is known about the factors that contribute to the disparity of crowding level.
This study described the wide variety of crowding status among EDs and investigated factors associated with the level of crowding.
MATERIALS AND METHODS
Study design and setting
This was a nationwide cross-sectional observational study. EDs are officially categorized as level I, II, or III by a government health authority. There are 16 level I EDs, 115 level II EDs, and approximately 330 level III EDs in Korea.
The National Emergency Department Information System (NEDIS) database was the major source of information for this study. The NEDIS is a nationwide government-run system that contains clinical and administrative data. The NEDIS contains patient demographics and clinical information, including age, sex, type of medical insurance, and vital signs at presentation. The NEDIS also provides information about the process of care, such as route of visit, mode of visit (EMS or other), information about arrival and discharge times, and patient disposition after the ED visit. Information regarding ED resources such as the number of beds, physicians, and nurses was acquired from the annual report from the National Emergency Medical Center.
Selection of participating EDs
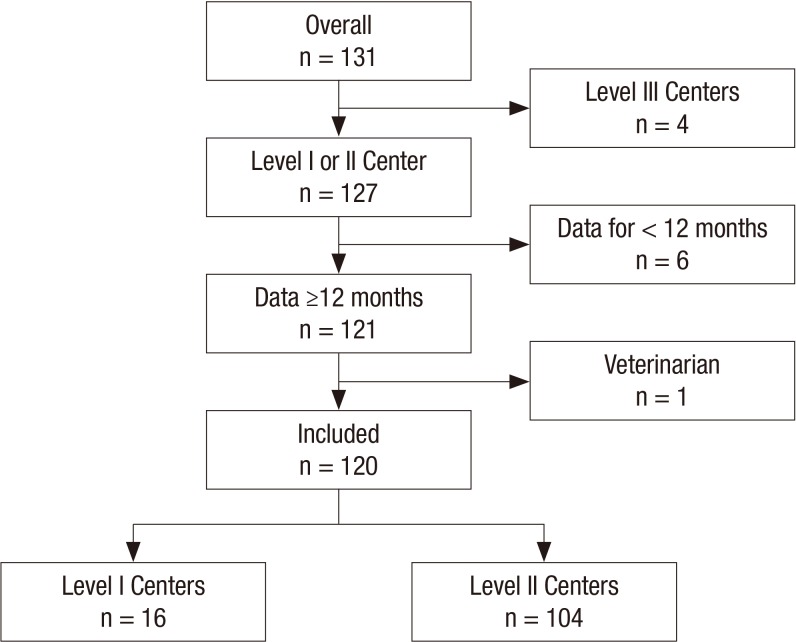
This study was conducted from June 1, 2009, to May 30, 2010. We included EDs above level III. We excluded hospitals for which NEDIS data had been collected for less than 12 months. Finally, one veteran's hospital was excluded because it was an ED that only served as a route for emergency admission. The process of selecting EDs is illustrated in Fig. 1.
Fig. 1.
Selection of study hospitals. Overall, 120 nation-wide Emergency centers were included.
Data collection and processing
We abstracted data from the NEDIS and calculated mean occupancy rates to quantify the crowding status of the EDs included in this study. Patient log data were used to calculate patient volume, which is the sum of patients staying at the ED at a specific time. The log data includes timing of entrance and exit to emergency department for each patient along with its mode. We used ED occupancy rates to define crowded categories in order to standardize comparisons of crowding states across different EDs; this measure has been widely accepted as the 'crowding index' (19,20,21,22,23,24). We divided the EDs into three groups according to their mean occupancy rates. Occupancy rates of 0.50 and 1.00 were used as cut-off values.
Outcome measures
Factors associated with ED crowding were included for analysis. Variables were grouped into three categories: input factors, throughput factors, and output factors (25,26).
Primary data analysis
STATA version 12.1 (Stata Corp, College Station, Tx) software was used for statistical analysis. Continuous variables are presented as median (IQR: interquartile range). Categorical variables are expressed in percentages of the total number of data points available within the database. Univariate linear regression was used to compare continuous variables between groups. Finally, multivariate regression analysis of the generalized-linear model was used to estimate crowding status after adjusting for other potential factors.
Ethics statement
The study was approved by the institution's ethics committee, and researchers signed a confidentiality term regarding the handling of patient data (2015-03-001). Informed consent was exempted by the board.
RESULTS
Characteristics of study subjects
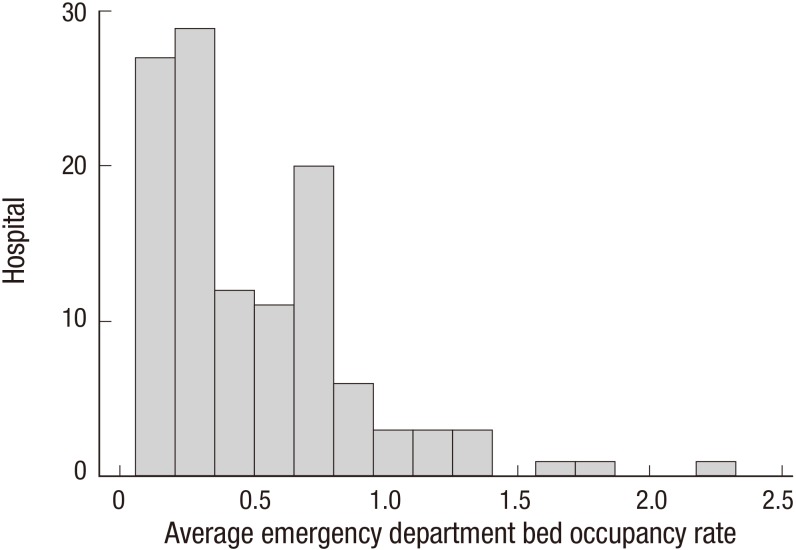
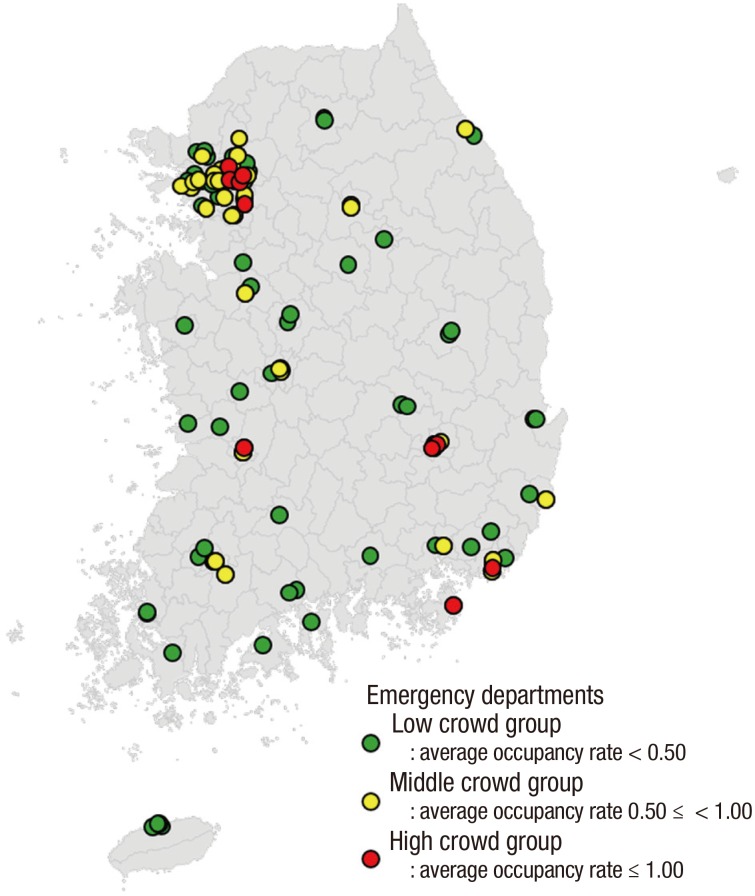
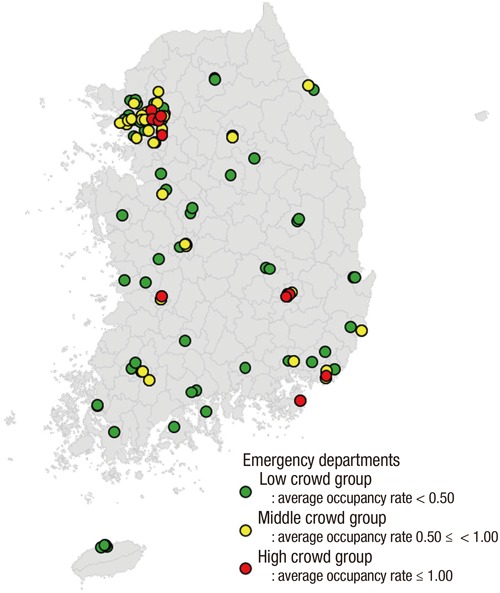
A total of 120 EDs were included in the final analysis. Of these, 16 were level I and 104 were level II (Fig. 1). The mean occupancy rate varied from 0.06 to 2.33. The median value was 0.39 with an IQR of 0.20 to 0.71. Fig. 2 shows the distribution of ED occupancy rates. There were 73 (60.8%) EDs in the 'low crowded' (LC) group (occupancy rate < 0.50), 37 (30.8%) in the 'middle crowded' (MC) group (0.50 ≤ occupancy rate < 1.00), and 10 (8.4%) in the 'high crowded' (HC) group (1.00 ≤ occupancy rate). The distribution of EDs is shown in Fig. 2 and 3. Many overcrowded EDs were located in metropolitan areas, especially around Seoul.
Fig. 2.
Average ED bed occupancy rate. The median was 0.39 with inter-quartile range 0.20–0.71.
Fig. 3.
Locations of enrolled emergency departments. Note that high crowd emergency departments are co-located among low crowd emergency departments. Many overcrowded EDs are located in Metropolitan area, especially in Seoul.
Main results
We first analyzed input factors. The median annual visits increased from 23,706 in the LC group to 41,443 in the HC group (P value for trend < 0.001). The percentage of elderly patients increased from 12.4% to 21.4% (P value for trend < 0.001). Patients transported by ambulance increased from 15.0% to 17.5%, but the difference was not statistically significance (P value for trend = 0.101). The percentage of patients referred from other facilities increased approximately 4-fold, from 5.09% to 20.2% (P value for trend < 0.001). Patients with injuries decreased from 26.1% to 22.4% (P value for trend < 0.001). Patients with unstable presenting vital signs increased from 3.99% to 9.57% (P value for trend = 0.001). Patient visits during office hours increased from 23.5% to 36.4% (P value for trend < 0.001). In brief, crowded EDs had higher annual visits, older patients, higher percentages of referred cases, lower percentages of patients with injuries, and higher rates of patients with unstable vital signs (Table 1).
Table 1. Characteristics of input factors.
| Mean occupancy rates | Average ED occupancy rates | P for trend | |||
|---|---|---|---|---|---|
| Low crowd Group (LC) < 0.50 n = 73 |
Middle crowd Group (MC) 0.50-1.00 n = 37 |
High crowded Group (HC) 1.00 ≤ n = 10 |
Overall n = 120 |
||
| Annual visits, No. | 23,706 (17,160-32,181) | 37,513 (32,519-57,940) | 41,443 (32,014-64,024) | 30,188 (20,235-41,861) | < 0.001 |
| Age, yr | 32 (30-36) | 32 (28-42) | 42 (34-47) | 32 (29-38) | 0.021 |
| ≥ 65, % | 12.4 (10.7-15.8) | 15.7 (11.4-21.6) | 21.4 (14.8-26.5) | 13.3 (11.1-19.1) | < 0.001 |
| < 15, % | 26.6 (22.7-30.9) | 29.8 (19.7-37.1) | 25.4 (19.1-26.9) | 26.7 | 0.819 |
| Transportation by ambulance, % | 15.0 (12.7-18.2) | 16.0 (12.1-22.3) | 17.5 (12.1-26.7) | 15.1 (12.3-19.1) | 0.101 |
| Transferred from other hospitals, % | 5.09 (3.00-7.41) | 10.3 (7.14-17.8) | 20.2 (11.1-24.9) | 7.13 (3.87-12.9) | < 0.001 |
| Injured patients, % | 26.1 (22.6-31.2) | 21.5 (18.3-26.4) | 22.4 (15.3-25.6) | 24.8 (20.6-29.2) | < 0.001 |
| Unstable vital signs, % | 3.99 (2.42-6.47) | 7.62 (4.55-13.4) | 9.57 (4.59-13.1) | 5.67 (2.95-9.63) | 0.001 |
| Office hours, % | 23.5 (20.0-26.1) | 28.2 (25.5-32.0) | 36.4 (32.5-41.0) | 25.2 (21.4-29.6) | < 0.001 |
All figures were given in median and interquartile range.
P for trend was calculated based on volume-bed ratio as continuous variable.
Among throughput factors, the median number of beds increased from 21 to 41 (P value for trend < 0.001). The median number of emergency physicians and nurses also increased (P value for trend < 0.001). However, patient-physician and patient-nurse ratios decreased as crowding increased (P value for trend < 0.001). The ED length of stay (LOS) increased from 110.2 to 563.6 minutes (P value for trend < 0.001). Among all patient groups, the LOS of admitted patients increased the most, from 183.9 to 1,161.4 minutes (P value for trend < 0.001) (Table 2).
Table 2. Characteristics of throughoutput factors.
| Mean occupancy rates | Average ED occupancy rates | P for trend | |||
|---|---|---|---|---|---|
| Low crowd Group (LC) < 0.50 n = 73 |
Middle crowd Group (MC) 0.50–1.00 n = 37 |
High crowded Group (HC) 1.00 ≤ n = 10 |
Overall n = 120 |
||
| ED beds | 21 (20–27) | 30 (23–36) | 41 (30–46) | 24 (20–30) | < 0.001 |
| Emergency physicians | 4 (2–7) | 9 (6–13) | 11 (7–19) | 6 (3–9) | < 0.001 |
| Patient-physician ratio | 1.11 (0.81–1.64) | 2.71 (1.68–3.90) | 3.76 (2.81–7.38) | 1.56 (0.97–2.94) | < 0.001 |
| Emergency nurses | 16 (13–20) | 29 (24–34) | 46 (31–55) | 20 (14–28) | < 0.001 |
| Patient-nurse ratio | 0.31 (0.24–0.43) | 0.80 (0.60–0.84) | 1.13(0.97–1.33) | 0.46 (0.29–0.74) | < 0.001 |
| ED LOS, overall, min | 110.2 (90.4–141.9) | 285.0 (187.1–402.5) | 563.6 (433.0–719.0) | 143.0 (106.4–273.2) | < 0.001 |
| ED LOS, discharged | 95.5 (73.9–122.2) | 186.9 (145.6–275.5) | 357.4 (237.4–408.5) | 122.7 (91.3–195.9) | < 0.001 |
| ED LOS, transferred, | 181.7 (127.5–221.4) | 364.2 (268.4–650.1) | 888.6 (771.1–933.0) | 232.0 (158.9–368.3) | < 0.001 |
| ED LOS, admitted | 183.9 (147.8–230.3) | 603.7 (369.0–796.7) | 1161.4 (1119.4 –1402.2) | 278.2 (175.2–606.4) | < 0.001 |
| ED LOS, age ≥ 65 yr | 159.0 (136.6–209.0) | 497.9 (293.3–661.9) | 886.2 (788.4–1066.4) | 225.0 (152.6–479.3) | < 0.001 |
| ED LOS, age < 15 yr | 82.4 (61.3–103.2) | 152.9 (137.7–198.3) | 295.0 (222.7–360.4) | 104.8 (74.0–160.6) | < 0.001 |
| ED LOS, injured | 98.4 (75.7–119.7) | 184.3 (154.9–311.6) | 295.4 (203.9–433.1) | 125.1 (91.1–183.1) | < 0.001 |
| ED LOS, unstable vital signs | 137.3 (111.1–176.2) | 338.0 (212.7–451.5) | 668.1 (586.3–826.9) | 173.9 (114.2–390.2) | < 0.001 |
| ED LOS, office hours | 118.7 (98.8–161.6) | 357.3 (236.5–515.1) | 729.2 (586.3–826.9) | 173.9 (114.2–390.2) | < 0.001 |
All figures were given in median and interquartile range.
P for trend was calculated based on volume-bed ratio as continuous variable.
Output factors were also analyzed. The percentage of discharge decreased from 76.9% to 69.2% from LC to HC (P value for trend < 0.001). Both rates of transfer and transfer after transfer increased (P value for trend < 0.001). The rate of death increased from 0.90% to 1.85%. However, the rate of death of unstable patients decreased from 12.8% to 6.82% (P value for trend = 0.022). Hospital beds increased from 477 to 833 as ED occupancy rate increased (P value for trend < 0.001). The mean occupancy rate of hospital beds increased from 85.6% to 93.3% (P value for trend = 0.002). Hospital beds occupied by emergency patients also increased from 26.3% to 41.0% (P value for trend < 0.001) (Table 3).
Table 3. Characteristics of output factors.
| Mean occupancy rates | Average ED occupancy rates | P for trend | |||
|---|---|---|---|---|---|
| Low crowd Group (LC) < 0.50 n = 73 |
Middle crowd Group (MC) 0.50-1.00 n = 37 |
High crowded Group (HC) 1.00 ≤ n = 10 |
Overall n = 120 |
||
| Hospital beds | 477 (380-557) | 736 (608-897) | 833 (736-1435) | 553 (407-796) | < 0.001 |
| Occupancy, % | 85.6 (79.4-91.4) | 90.6 (86.7-94.4) | 93.3 (91.7-95.4) | 89.3 (82.0-93.9) | 0.002 |
| Occupancy by emergency, % | 26.3 (14.3-36.8) | 36.2 (28.7-45.3) | 41.0 (32.6-46.2) | 32.5 (20.7-40.7) | < 0.001 |
| Ratio (elective/emergency) | 2.04 (1.30-4.66) | 1.66 (1.00-2.35) | 1.28 (1.03-1.65) | 1.77 (1.16-3.06) | 0.119 |
| ED disposition | |||||
| Discharge, % | 76.9 (73.2-82.8) | 75.0 (63.0-80.2) | 69.2 (54.2-75.7) | 76.5 (67.4-81.3) | 0.001 |
| Discharge after transfer, % | 28.4 (21.2-36.9) | 38.0 (28.8-43.9) | 37.0 (35.1-40.6) | 33.9 (24.0-40.6) | < 0.001 |
| Trauma discharge, % | 79.1 (71.4-86.2) | 81.1 (72.8-87.3) | 79.6 (67.1-90.0) | 80.1 (71.1-87.0) | 0.531 |
| Unstable patient discharge, % | 43.2 (30.2-61.8) | 57.4 (44.1-66.6) | 45.2 (39.9-52.6) | 50.0 (33.8-63.8) | 0.224 |
| Transfer, % | 0.89 (0.46-1.62) | 1.33 (0.57-3.35) | 3.09 (2.01-6.00) | 0.99 (0.54-2.01) | < 0.001 |
| Re-transfer after transfer, % | 2.07 (1.16-3.50) | 3.32 (1.34-6.98) | 6.94 (5.31-11.2) | 2.49 (1.27-5.28) | 0.031 |
| Trauma transfer, % | 1.01 (0.47-2.10) | 2.04 (0.69-6.08) | 4.84 (3.53-9.55) | 1.48 (0.54-2.96) | < 0.001 |
| Unstable patient transfer, % | 2.42 (1.25-5.78) | 2.03 (1.30-3.60) | 5.06 (3.14-6.95) | 2.39 (1.39-5.50) | 0.058 |
| Admission, % | 17.1 (14.3-21.9) | 20.9 (16.2-33.6) | 25.7 (19.4-34.2) | 18.8 (15.2-24.8) | 0.002 |
| Admission after transfer, % | 2.07 (1.16-3.50) | 3.32 (1.35-6.98) | 6.94 (5.31-11.2) | 2.49 (1.27-5.28) | 0.031 |
| Trauma admission, % | 18.2 (11.2-22.3) | 12.8 (8.14-20.1) | 14.6 (6.73-18.5) | 15.5 (6.73-18.5) | 0.011 |
| Unstable patient admission, % | 33.9 (24.8-43.2) | 36.0 (26.9-41.5) | 35.0 (31.2-41.9) | 34.3 (25.9-42.9) | 0.895 |
| Death, % | 0.90 (0.65-1.21) | 1.33 (0.98-1.96) | 1.85 (1.68-2.72) | 1.02 (0.74-1.65) | < 0.001 |
| Death after transfer, % | 2.77 (1.45-4.00) | 3.10 (2.11-4.06) | 3.66 (2.49-4.63) | 2.91 (1.61-4.09) | 0.364 |
| Death of injured, % | 0.56 (0.38-0.78) | 0.91 (0.43-1.56) | 0.87 (0.36-1.94) | 0.62 (0.38-0.97) | 0.001 |
| Death of unstable patient, % | 12.8 (6.38-18.5) | 9.08 (4.99-11.2) | 6.82 (5.58-12.8) | 10.1 (5.71-17.5) | 0.022 |
All figures were given in median and interquartile range.
P for trend was calculated based on volume-bed ratio as continuous variable.
Finally, we performed multivariate analysis that included potentially significant factors (P ≤ 0.10). After adjustment, ED crowding was significantly influenced by the number of visits (0.42% increase per 1,000 additional visits, P = 0.053), percentage of patients referred (0.14% increase per 1% of elderly patients, P = 0.015), number of nurses (0.96% increase per nurse, P = 0.009), and ED dispositions such as transfer from ED, admission from ED, and death in ED (P = 0.041, P < 0.001, P < 0.001, respectively). However, there was no statistically significant association between hospital factors and ED crowding (Table 4).
Table 4. Multivariate analysis predicting ED crowding (mean occupancy rate).
| Variables | Coefficient | 95% Confidence Interval | P value | |
|---|---|---|---|---|
| Input factors | ||||
| Annual volume (/1,000 visits) | 0.42 | -0.01 | 0.84 | 0.053 |
| % of over 65 yr | 0.14 | -0.88 | 1.15 | 0.788 |
| % of transported by ambulance | 0.24 | -0.85 | 1.33 | 0.661 |
| % of transferred from other hospital | 1.16 | 0.24 | 2.09 | 0.015 |
| % of injuries | -0.53 | -1.22 | 0.17 | 0.135 |
| % of unstable patients (Unstable vital signs) | 0.48 | -0.28 | 1.24 | 0.214 |
| Throughput factors | ||||
| Registered physicians | 1.06 | -0.31 | 2.42 | 0.129 |
| Registered nurses | 0.96 | 0.25 | 1.67 | 0.009 |
| Output factors | ||||
| Disposition | ||||
| % of transfer from ED to other facilities | 2.99 | 0.12 | 5.87 | 0.041 |
| % of admission from ED | -1.05 | -1.76 | -0.35 | < 0.001 |
| % of death in ED | 20.0 | 10.9 | 29.1 | < 0.001 |
| Hospital factors | ||||
| No. of hospital beds | -0.01 | -0.03 | 0.01 | 0.384 |
| % of average hospital occupancy rate | 0.47 | -0.06 | 0.99 | 0.083 |
DISCUSSION
In our study, we gathered data from 120 officially designated EDs and found significant differences in crowding state. Since Korea has a very high population density and EDs are generally not very far away from one another, the wide variance among EDs is noteworthy. In contrast, ED crowding in the USA tends to rise simultaneously among neighboring institutes, resulting in gridlocks (29). This implies that national optimization efforts are required to efficiently solve the problem. The spatial variance of hospitals and crowding state shown in Fig. 2 also emphasizes the need for further investigation on community factors that affect ED crowding. Many overcrowded EDs are located alongside less crowded EDs in metropolitan areas, especially around Seoul.
Among input factors evaluated in this study, ED crowding was associated with the number of visits and patient severity level, both factors reported previously. However, unlike other studies, the number of patients transferred by ambulances was not associated with crowding in this study (25,27,30). The number of patients with injuries and patients referred from other facilities were negatively and positively associated with crowding with strong statistical significance, respectively, factors also not previously described. Patient visits during office hours may imply that EDs serve these patients as walk-in clinics or acute-relief units for chronic conditions, which might be targets for further interventions to reduce crowding.
Among throughput factors, the number of healthcare providers and relative manpower were strongly associated with crowding level. The absolute number of care providers was higher in crowded EDs, but the provider-to-patient ratio was lower, consistent with previous studies (25,31). In our dataset, we could not show specific throughput intervals such as time to triage or time to certain labs; we instead focused on the length of stay for specific categories of patients and on the evaluation of their associations with ED crowding state.
Among output factors, we focused on hospital capacity and found a positive correlation between hospital bed occupancy rates and ED crowding state, similar to reports from other studies (30,32). We also identified a positive association with strong statistical significance between hospital bed size and crowding. This finding is contrary to previous reports that in-hospital resource expansion would relieve ED crowding, and observation that requires further investigation (21). The elective: emergency ratio revealed that hospitals with ED crowding try to admit more patients from EDs, though a significant proportion of patients were still admitted from the outpatient department. We also found diverse outcome differences regarding crowding state that increased secondary transfer of patients, and increased overall mortality among EDs with high crowding state.
This study has some practical and potential limitations. First, even though EDs were sampled nationwide, not every ED was included. All level III and some level II EDs were excluded from this study. Therefore, selection bias is possible. However, our data showed that ED crowding more frequently occurs at more comprehensive centers such as level I EDs, so this potential bias should not have significant affected the results.
Second, we only used occupancy rates as a surrogate marker of ED crowding. Other indices, such as the number of patients who leave without being seen (LWBS) and ambulance diversions, were not included in this study (21,28). The cut-off values of occupancy rate in this study are not consensus values, which could also influence the outcome.
Third, the study took place in Korea, which has its unique emergency medical systems. Distinct from western countries, Korean emergency medical system shows high level of low acuity patients, low rate of ambulance-transported patients, and frequent transportation among emergency facilities (33,34,35).
Finally, we only searched for association among factors. We were unable to identify causal relationships. For example, hospital beds occupied by emergency beds were significantly associated with the level of crowding, but it is not clear whether the association was the result or the cause of crowding.
In conclusion, this nationwide study revealed great disparities in ED crowding. The number of ED visits, proportion of transfer patients, number of nurses, ED disposition to wards, relationship to other institutes, and ED mortality were factors associated with ED crowding.
Footnotes
Funding: This study is supported by the Ministry of Health and Welfare.
DISCLOSURE: All authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design of study: Ahn KO, Cha WC, Cho JS. Acquisition of data: Ahn KO, Shin SD. Analysis and interpretation of data: Park JH. Drafting the article or revising it critically for important intellectual content: Cha WC. Final approval of the version to be submitted: all authors.
References
- 1.Institute of Medicine Committee on the Future of Emergency Care in the United States Health System (US) Hospital-Based Emergency Care: at the Breaking Point. Washington, D.C.: National Academies Press; 2007. [Google Scholar]
- 2.Sun BC, Binstadt ES, Pelletier A, Camargo CA., Jr Characteristics and temporal trends of “left before being seen” visits in US emergency departments, 1995-2002. J Emerg Med. 2007;32:211–215. doi: 10.1016/j.jemermed.2006.05.045. [DOI] [PubMed] [Google Scholar]
- 3.Asaro PV, Lewis LM, Boxerman SB. Emergency department overcrowding: analysis of the factors of renege rate. Acad Emerg Med. 2007;14:157–162. doi: 10.1197/j.aem.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Pines JM, Localio AR, Hollander JE, Baxt WG, Lee H, Phillips C, Metlay JP. The impact of emergency department crowding measures on time to antibiotics for patients with community-acquired pneumonia. Ann Emerg Med. 2007;50:510–516. doi: 10.1016/j.annemergmed.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1–5. doi: 10.1016/j.annemergmed.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Krochmal P, Riley TA. Increased health care costs associated with ED overcrowding. Am J Emerg Med. 1994;12:265–266. doi: 10.1016/0735-6757(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 7.Bayley MD, Schwartz JS, Shofer FS, Weiner M, Sites FD, Traber KB, Hollander JE. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med. 2005;45:110–117. doi: 10.1016/j.annemergmed.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Cameron PA. Hospital overcrowding: a threat to patient safety? Med J Aust. 2006;184:203–204. doi: 10.5694/j.1326-5377.2006.tb00200.x. [DOI] [PubMed] [Google Scholar]
- 9.Weber EJ, Mason S, Carter A, Hew RL. Emptying the corridors of shame: organizational lessons from England's 4-hour emergency throughput target. Ann Emerg Med. 2011;57:79–88.e1. doi: 10.1016/j.annemergmed.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 10.Hatamabady HR. 291: causes of length of stay in a typical crowded emergency department of a teaching hospital in Tehran capital city. Ann Emerg Med. 2008;52(Suppl):S131. [Google Scholar]
- 11.Miró O. State of emergency medicine in Spain. Int J Emerg Med. 2010;3:219–226. doi: 10.1007/s12245-010-0249-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Emergency Physicians. Emergency department crowding information paper [Internet] [accessed on 24 Feburary 2016]. Available at http://www.acep.org/workarea/DownloadAsset.aspx?id=8872.
- 13.Derlet RW, Richards JR. Overcrowding in the nation's emergency departments: complex causes and disturbing effects. Ann Emerg Med. 2000;35:63–68. doi: 10.1016/s0196-0644(00)70105-3. [DOI] [PubMed] [Google Scholar]
- 14.Derlet RW. Overcrowding in emergency departments: increased demand and decreased capacity. Ann Emerg Med. 2002;39:430–432. doi: 10.1067/mem.2002.122707. [DOI] [PubMed] [Google Scholar]
- 15.Pham JC, Ho GK, Hill PM, McCarthy ML, Pronovost PJ. National study of patient, visit, and hospital characteristics associated with leaving an emergency department without being seen: predicting LWBS. Acad Emerg Med. 2009;16:949–955. doi: 10.1111/j.1553-2712.2009.00515.x. [DOI] [PubMed] [Google Scholar]
- 16.Hsia RY, Asch SM, Weiss RE, Zingmond D, Liang LJ, Han W, McCreath H, Sun BC. Hospital determinants of emergency department left without being seen rates. Ann Emerg Med. 2011;58:24–32.e3. doi: 10.1016/j.annemergmed.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCabe JB. Emergency department overcrowding: a national crisis. Acad Med. 2001;76:672–674. doi: 10.1097/00001888-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Espinosa G, Miró O, Sánchez M, Coll-Vinent B, Millá J. Effects of external and internal factors on emergency department overcrowding. Ann Emerg Med. 2002;39:693–695. doi: 10.1067/mem.2002.124447. [DOI] [PubMed] [Google Scholar]
- 19.Hoot NR, Leblanc LJ, Jones I, Levin SR, Zhou C, Gadd CS, Aronsky D. Forecasting emergency department crowding: a prospective, real-time evaluation. J Am Med Inform Assoc. 2009;16:338–345. doi: 10.1197/jamia.M2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han JH, Zhou C, France DJ, Zhong S, Jones I, Storrow AB, Aronsky D. The effect of emergency department expansion on emergency department overcrowding. Acad Emerg Med. 2007;14:338–343. doi: 10.1197/j.aem.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Solberg LI, Asplin BR, Weinick RM, Magid DJ. Emergency department crowding: consensus development of potential measures. Ann Emerg Med. 2003;42:824–834. doi: 10.1016/S0196064403008163. [DOI] [PubMed] [Google Scholar]
- 22.Ospina MB, Bond K, Schull M, Innes G, Blitz S, Rowe BH. Key indicators of overcrowding in Canadian emergency departments: a Delphi study. CJEM. 2007;9:339–346. doi: 10.1017/s1481803500015281. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy ML, Aronsky D, Jones ID, Miner JR, Band RA, Baren JM, Desmond JS, Baumlin KM, Ding R, Shesser R. The emergency department occupancy rate: a simple measure of emergency department crowding? Ann Emerg Med. 2008;51:15–24. 24.e1–24.e2. doi: 10.1016/j.annemergmed.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Hoot NR, Zhou C, Jones I, Aronsky D. Measuring and forecasting emergency department crowding in real time. Ann Emerg Med. 2007;49:747–755. doi: 10.1016/j.annemergmed.2007.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42:173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 26.Hwang U, McCarthy ML, Aronsky D, Asplin B, Crane PW, Craven CK, Epstein SK, Fee C, Handel DA, Pines JM, et al. Measures of crowding in the emergency department: a systematic review. Acad Emerg Med. 2011;18:527–538. doi: 10.1111/j.1553-2712.2011.01054.x. [DOI] [PubMed] [Google Scholar]
- 27.Bullard MJ, Villa-Roel C, Bond K, Vester M, Holroyd BR, Rowe BH. Tracking emergency department overcrowding in a tertiary care academic institution. Healthc Q. 2009;12:99–106. doi: 10.12927/hcq.2013.20884. [DOI] [PubMed] [Google Scholar]
- 28.Schull MJ, Slaughter PM, Redelmeier DA. Urban emergency department overcrowding: defining the problem and eliminating misconceptions. CJEM. 2002;4:76–83. doi: 10.1017/s1481803500006163. [DOI] [PubMed] [Google Scholar]
- 29.Schull MJ, Morrison LJ, Vermeulen M, Redelmeier DA. Emergency department gridlock and out-of-hospital delays for cardiac patients. Acad Emerg Med. 2003;10:709–716. doi: 10.1111/j.1553-2712.2003.tb00064.x. [DOI] [PubMed] [Google Scholar]
- 30.Asaro PV, Lewis LM, Boxerman SB. The impact of input and output factors on emergency department throughput. Acad Emerg Med. 2007;14:235–242. doi: 10.1197/j.aem.2006.10.104. [DOI] [PubMed] [Google Scholar]
- 31.Steele R, Kiss A. EMDOC (Emergency Department overcrowding) Internet-based safety net research. J Emerg Med. 2008;35:101–107. doi: 10.1016/j.jemermed.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 32.Jones SS, Evans RS, Allen TL, Thomas A, Haug PJ, Welch SJ, Snow GL. A multivariate time series approach to modeling and forecasting demand in the emergency department. J Biomed Inform. 2009;42:123–139. doi: 10.1016/j.jbi.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Park HA, Ahn KO, Shin SD, Cha WC, Ro YS. The Effect of emergency medical service use and inter-hospital transfer on prehospital delay among ischemic stroke patients: a multicenter observational study. J Korean Med Sci. 2016;31:139–146. doi: 10.3346/jkms.2016.31.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwak YH, Kim DK, Jang HY. Utilization of emergency department by children in Korea. J Korean Med Sci. 2012;27:1222–1228. doi: 10.3346/jkms.2012.27.10.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kang SW, Park HS. Emergency department visit volume variability. Clin Exp Emerg Med. 2015;2:150–154. doi: 10.15441/ceem.14.044. [DOI] [PMC free article] [PubMed] [Google Scholar]