Abstract
Traditional B-Mode and Doppler sonography have been the stalwart of renal tract imaging for many years, and indeed, are in daily use in most centres as the modality of choice for the initial assessment of renal pathology. However, traditional ultrasound scanning can be limited in its ability to accurately characterise renal pathology, and can be inaccurate at determining benign from malignant lesions. Contrast-enhanced ultrasound conveys many benefits, being safe (especially in patients with renal dysfunction), does not require the use of ionising radiation, is quick and relatively cheap and can help to establish whether a focal renal lesion is sinister. Furthermore, it is our experience that contrast-enhanced ultrasound is not a difficult technique to master for the experienced ultrasound practitioner. In this article, we discuss the technique, interpretation and value of contrast-enhanced ultrasound in renal imaging, and describe how we use it in our practice.
Keywords: Kidney, ultrasound, ultrasound contrast, contrast microbubbles
Introduction
Renal ultrasound (US) is a frequently used examination, and incidental findings are therefore common. The kidneys are also imaged with CT and MRI; this can be both to investigate renal pathology directly but also as a consequence of imaging other organs. Incidental findings are common; thus, a robust method of characterising renal abnormalities is required. Standard ultrasound (US) is a good screening tool but cannot always characterise lesions. Particular challenges include the fact that lesions are frequently isoechoic to the renal parenchyma on grey-scale imaging, and assessment of the micro-circulation using Doppler can be difficult. Standard US therefore remains inaccurate at distinguishing benign from malignant lesions.1
In 2011, guidelines were published by the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) for the non-liver use of CEUS.2 They recommend several indications for the use of CEUS in the kidneys, despite this being an unlicensed use. These are: in suspected vascular disorders (infarction, cortical necrosis); differentiating between solid and cystic lesions; differentiating between tumours and pseudotumours; characterisation and follow-up of complex cystic masses; identification of renal abscesses; in radiofrequency ablation (RFA) of non-surgical masses.
Across the country, imaging departments are under increasing pressure to provide rapid and accurate diagnoses, within ever increasing financial restraints.3 There is a year on year increase in cross-sectional imaging, with a rise of 11.1% in the number of CT scans performed in England over the two years between 2012/13 and 2014/15 alone.4 Incidentally, detected renal lesions are therefore on the rise, with the incidence of renal cancer rising from 7.1 to 10.8 cases per 100,000 between 1983 and 2002 in one large US study.5 Whilst changes in risk factors are likely to be partially contributory,6 most of this rise can be attributed to the incidental detection of small, potentially curable renal cancers.5 The timing is ripe, therefore, for the wider adoption of this straightforward, relatively cheap, reliable and safe method for accurately characterising renal lesions. In this article, we discuss the technique, interpretation and value of CEUS in renal imaging, and describe how we use it in our practice.
Are microbubbles safe?
Microbubbles are safer than iodinated- and gadolinium-based contrast material, particularly in patients with renal impairment. They have been in clinical use for more than 15 years and were initially developed for use in echocardiography.7 Much early published work focused on their role in liver imaging2 and their use for this purpose is now routine and recommended in NICE guidelines.8 In the UK, the market is dominated by SonoVue (Bracco International BV, Amsterdam, The Netherlands) with other agents used infrequently. SonoVue is authorised for use in Europe for echocardiography and the imaging of large vessels, as well as microvasculature (specifically of the liver and breast).9 Microbubbles are biologically inert and generally consist of a biocompatible shell and a core of gas.10 In the case of SonoVue, there is a phospholipid shell encasing a sulfur hexafluoride gas centre.2 Rates of adverse events are extremely low, with one large multicentre trial quoting incidence in less than 0.01% of examinations.11 Generally, these represented hypotensive reactions which responded readily to fluid resuscitation. Although anaphylactoid reactions occur at a vanishingly rare rate, less than 0.002%,11 available resuscitation facilities are mandatory when using microbubble contrast. Their use is contraindicated in patients known to have right-to-left shunts, severe pulmonary hypertension, uncontrolled systemic hypertension and in patients with adult respiratory distress syndrome.9 Rates of adverse events from microbubbles compare favourably with those from low-osmolar iodine based and gadolinium-based agents, which have been reported as occurring at between 0.2% and 0.7% and 0.07% and 2.4%, respectively.12 Serious and life-threatening acute reactions to low osmolar CT contrast agents occur in approximately 0.04% of cases but are very rare in gadolinium-based agents.12
Described cellular effects in vitro from microbubbles include sonoporation (increase in permeability of the cell membrane), haemolysis and cell death. These are the result of cavitation of the microbubbles when subjected to the ultrasonic waves. Some studies have concluded that capillary microhaemorrhage can occur when contrast agents are insonated at high mechanical index (MI).13 Outside of particular sensitive tissues, such as the eyes and brain, these effects are not generally felt to be of concern in people. Some work has suggested that CEUS can have deleterious effects to rat glomeruli, but a later study into porcine kidneys (a closer analogue of human tissue) did not reproduce this effect.13 They are therefore not considered nephrotoxic.2 This is in direct contrast with CT and MRI contrast agents that are known to impact negatively upon renal function or have serious untoward effects in patients with already impaired renal function. CEUS therefore provides a safe first-line tool for investigating renal anomalies, which are often picked up incidentally when US scanning the patient with acute kidney injury or chronic kidney disease.
Whilst the safety of these agents is generally accepted, it must be borne in mind that their use in the kidneys is unlicensed. At the authors’ institution, we have an honest discussion with patients before proceeding with the examination, and in our experience the patient is always happy to proceed after an explanation. This verbal consent for the ‘off-label’ use of the drug is documented in the report. We have had no serious adverse events to date in our institution.
Technique and normal findings
The kidneys are retroperitoneal organs normally found in the flanks at the level of T12 to L3, lying obliquely. Normal size is 9–12 cm. On B mode US in a slim or young patient, the moderately echogenic renal cortex can be distinguished from the hypoechoic medullary pyramids. The pyramids are separated by renal columns (of Bertin). Centrally, one can observe the echogenic renal sinus fat, the amount of which varies with size and body habitus. The anechoic renal pelvis is often not seen in the unobstructed kidney. On Doppler imaging, the renal arteries (often multiple) and vein can be observed, the artery branching into lobar, interlobar and arcuate branches, which can all be readily identified with careful technique. Examination can be performed supine or in the lateral decubitus position, using either an intercostal approach and using the liver or spleen as an acoustic window or by using a posterior approach.
Microbubbles produce echoes through oscillation at a low acoustic pressure. A measure of this value is provided by the MI and imaging is typically performed at an MI of 0.3 or below. At higher MIs, microbubble disruption occurs readily. Dedicated software is employed, present on most commercially available scanners. Imaging at a low acoustic pressure and with harmonic imaging minimises echoes from the background tissue, allowing clear visualisation of the microbubbles. The image appears dark, and normal structures are difficult to identify. Spatial localisation is therefore achieved with synchronous B-mode imaging, viewed using a split-screen display.
The contrast is injected through an intravenous cannula in the arm, ideally the antecubital fossa. A fast injection of the microbubbles is followed immediately by a flush of 10 ml of saline. A lower dose is required for renal imaging than for intravascular and cardiac use, so a 1.2 ml bolus of SonoVue is usually sufficient. In the kidneys, the majority of the microbubbles concentrate in the cortex (approximately 90%). It is the experience of us, and others in the field,14 that if much more than 2.4 ml is used then one risks obscuring the deeper parts of the kidney.
Enhancement timings are similar to those utilised for renal-specific CT imaging but have the benefit of being monitored in real-time, so optimum images can be obtained even in hyper- or hypodynamic circulations, where predetermined imaging timings with CT or MR might have missed the maximum enhancement. The cortical phase typically begins 10 to 15 seconds after injection and lasts 20 to 40 seconds, followed by a slower medullary phase lasting 45 to 120 seconds (Figure 1).14,15 The outer medulla fills first with gradual fill in of the pyramids, which become isoechoic with the cortex in the medullary phase.14 The examination is normally concluded by 3 minutes.
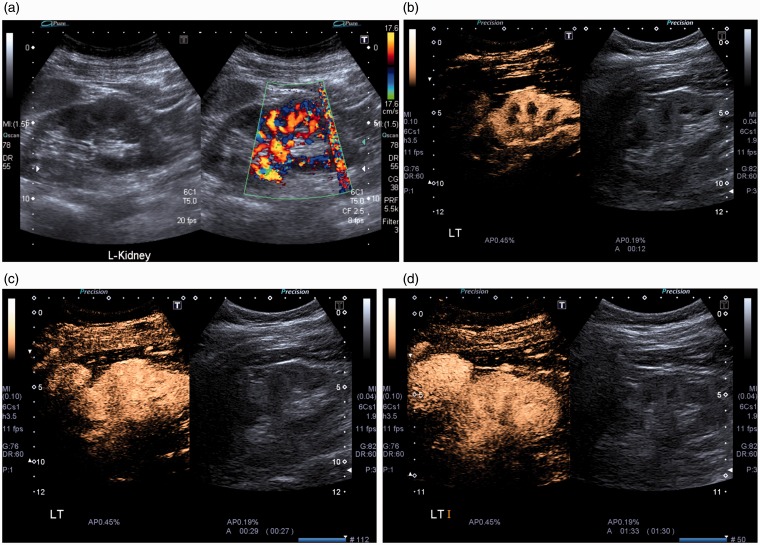
Figure 1.
Pseudotumour (dromedary hump). (a) Conventional ultrasound images demonstrate a focal bulge in the cortex of the mid to lower portion of the left kidney, with slightly heterogenous echogenicity and flow on Doppler imaging. (b) Cortical phase enhancement. (c) Early medullary phase (medullary pyramids filling in with contrast). (d) Later medullary phase. CEUS proves the enhancement pattern of the lesion is identical to that of the surrounding cortex, confirming a pseudotumour.
As described below, the characterisation of most renal lesions relies on the demonstration or absence of blood flow within a lesion, so in many ways is a less complex assessment that that required for CEUS in the liver where timings and washout are critical. The lesion of interest is observed constantly in the early stages of enhancement, and several images are taken. In the later stages, observation is often more sporadic, in order to preserve microbubble integrity. Cine clips can also be stored. The remaining contrast in the vial of SonoVue can be used any time within the next 6 hours,9 which allows multiple studies on the same list to be performed using just one vial of contrast.
It is the experience of the authors that CEUS is a relatively straightforward technique to learn for experienced US practitioners. Whilst there is no good published data on this subject, EFSUMB has published a curriculum16 that can enable the practitioner to target their learning needs and feel confident that they are working safely and appropriately.
Indications for renal CEUS and image interpretation
Differentiating cystic from solid lesions
Distinguishing between solid lesions and complex or hyperdense cysts can be difficult with any imaging modality. Hyperdense lesions are often discovered incidentally on CT scans performed for other reasons. When their density measures above 70 Hounsfield Units (HU) on unenhanced CT, they can be definitively diagnosed as high-density cysts.17 Between 20 and 70 HU, they require correlation with conventional sonography, where they can frequently be confidently diagnosed as cystic. In less conclusive cases, when for example the lesion is not clearly cystic on US, further characterisation remains essential, and has traditionally necessitated a dedicated bi-, or tri-phasic contrast enhanced CT scan, with the inherent disadvantages of radiation dose and potential nephrotoxicity from the contrast. The goal of this further imaging is the demonstration of contrast enhancement within the lesion; this implies perfusion and should be considered highly suspicious for malignancy. The absence of flow can allow the practitioner to confidently diagnose the lesion as benign (Figure 2).
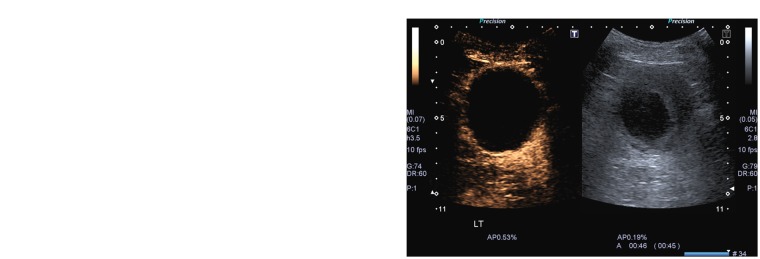
Figure 2.
Haemorrhagic cyst. (a) Grey-scale ultrasound with power Doppler image demonstrates a complex cystic lesion of the left kidney, with some solid material peripherally and a more cystic, multiseptated region centrally. (b) CEUS confirms the absence of vascularity within the lesion thereby allowing a confident diagnosis of a haemorrhagic cyst.
Even with a CT scan performed with a dedicated renal mass protocol, there remains the potential for false negatives, with one study of pathologically proven renal malignancies demonstrating no CT enhancement in 17% of cases.18 These hypovascular malignancies are most frequently papillary renal cell carcinoma.19 CEUS has been shown to be more sensitive than both CT and conventional sonography in detecting microvascular flow.18,20,21 In addition, unlike Doppler imaging it is not angle dependent, which is especially beneficial when imaging lesions at the poles. It also obviates the need for more invasive diagnostic tests such as biopsy, which can sometimes be required when all imaging tests prove inconclusive or prior to percutaneous therapy such as RFA/cryotherapy. Biopsies can be unpleasant for the patient and carry the risks of haemorrhage and tumour seeding. Their avoidance is therefore advantageous. Newer Doppler-based microvascular imaging techniques22 may as yet provide an alternative to CEUS use in this regard, but their efficacy is as yet unproven.
Differentiating masses from pseudotumours
The atypical appearing pseudotumour (such as a hypertrophied column of Bertin or dromedary hump) is a normal variant, which is frequently encountered on routine US lists. In most cases, these have an obviously benign appearance; the hypertrophied column of Bertin is typically seen as cortical tissue extending inwards from the periphery and ‘splitting’ the renal sinus. A dromedary hump is a focal bulge on the lateral border of the left kidney. When imaging characteristics are less typical, the practitioner faces the dilemma of either arranging a CT at a later date, at the cost of increased anxiety to the patient (as well as a radiation burden and possibly nephrotoxicity from the contrast) or calling the lesion normal, at the cost of increased anxiety to the practitioner. CEUS provides a quick and cheap way to solve this dilemma and provide a definitive diagnosis. Pseudotumours can be confidently diagnosed when the enhancement pattern mirrors that of the surrounding parenchyma in all phases (Figure 1).2,23,24 As described below, they can be easily distinguished from renal neoplasms, which will show differential enhancement in at least one phase.14
Characterisation (and follow-up) of complex renal cysts
CEUS is at least as accurate as CT in characterising complex cystic lesions.20,25,26 Whilst cysts are frequently encountered during routine renal sonography, unenhanced US can be inaccurate at differentiating between benign and malignant disease.1,26 CT is considered the gold standard, and complex cysts can be graded using the Bosniak system27 with high interobserver reliability.20 Grading ranges from I to IV, with grades I and II considered benign (grade IIF indicates a probably benign lesion that requires follow-up) and grades III and IV indicating a higher probability of malignancy. The latter are generally considered surgical lesions. A modified Bosniak classification has also been suggested for use with CEUS.20 Benign lesions typically show no enhancement, and if seen this reliably confirms benignity with a positive predictive value (PPV) of 100% in one study.28 They may also demonstrate the occasional bubble within septa.29
CEUS can identify more septa, characterise septa as thicker and pick up solid components within cystic lesions more frequently than CT (Figure 3).25,26,28 This has the effect of upgrading cysts from IIF to III (thick septa) or from III to IV (enhancing nodule indicating a frankly malignant lesion). There is no significant increase in the rate of false positives.
Figure 3.
Complex renal cyst. (a) Contrast-enhanced CT shows a minimally complex cyst in the left kidney with some appreciable septations, reported as a Bosniak IIF cyst (likely benign but requiring follow-up). (b) CEUS demonstrates enhancing septations within the cyst. (c) A further CEUS image from the same study shows areas of nodular enhancement (arrow). On the basis of the CEUS, this would be classified as a probable malignant lesion (the patient elected to continue active surveillance).
Characterisation of indeterminate renal lesions
CEUS really comes into its own in the assessment of indeterminate renal lesions, where its ability to demonstrate slow and low flow within lesions allows their characterisation as solid. The key to CEUS characterisation of renal lesions, rather than any particular enhancement pattern such as one would use in the liver, is the fact that malignant lesions generally show enhancement characteristics different to cortex in at least one phase.14 The diagnosis of pseudotumour can be definitively made if enhancement characteristics match the cortex throughout all phases. Any other enhancing lesion should be considered suspicious for malignancy.29 Whilst not all solid enhancing lesions are malignant, CEUS cannot at present reliably distinguish malignant from benign lesions based on enhancement characteristics, and thus is not recommended for the purpose of characterising solid lesions in the EFSUMB guidelines.2 In the case of renal angiomyolipomas (AMLs), these are typically echogenic lesions on conventional ultrasound. Various enhancement characteristics are described, ranging from a lesion enhancing less than the cortex, often peripherally,29 to sustained, homogenous enhancement with no wash-out.30 Significant overlap is present between the patterns of enhancement of AMLs and renal cell carcinomas (RCCs), so a diagnosis of AML should not be made with CEUS alone. In suspected AMLs, non-contrast CT or MRI to demonstrate macroscopic fat is required to confirm.14
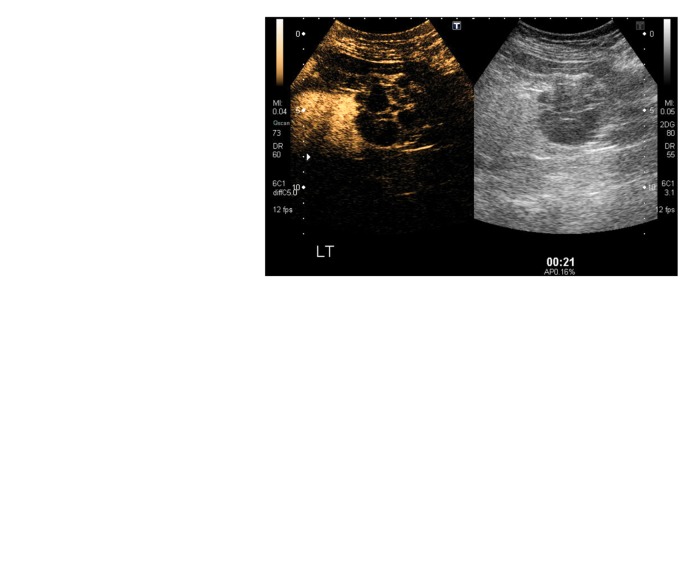
Typical patterns of contrast enhancement in malignant lesions include hyperenhancement, delayed enhancement, early washout or (in complex cysts) enhancing nodularity. An enhancing pseudocapsule around the lesion, secondary to compressed, necrotic and ischaemic tissue is considered characteristic of RCC.31 Using the above criteria, Barr et al.29 achieved a sensitivity of 100% for malignant lesions in a cohort of 596 lesions with only five false positives (three oncocytomas and two Bosniak III cysts). The consensus is that CEUS is an extremely accurate modality for characterising renal lesions32 and that it can even outperform CT (Figure 4).25,26
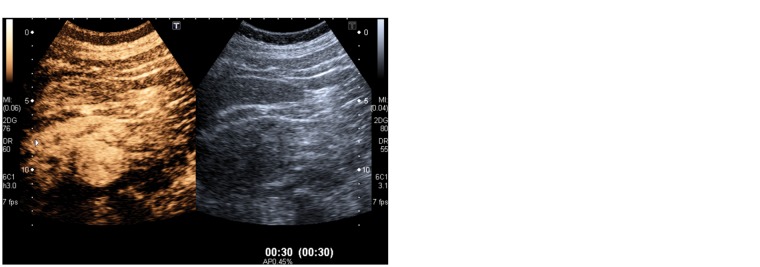
Figure 4.
Papillary renal cell carcinoma. (a) Pre- and postcontrast CT images demonstrate a minimally complex lesion with a rim of peripheral enhancement but no subjective or objective internal enhancement (less than 8 Hounsfield Units when measured). (b) Grey-scale ultrasound with power Doppler image of the lesion demonstrates heterogeneously high echogenicity but with only a trace of internal flow. (c) On the left, contrast enhanced image, there is marked peripheral enhancement on CEUS indicating a malignant lesion. This was subsequently proved on histology to be a papillary cell carcinoma.
Whilst CEUS is accurate in characterising indeterminate and complex cystic lesions, most departments will need to take a pragmatic approach to its use. It has been suggested that all complex cystic lesions should be initially evaluated with CEUS.26 Whilst this may be applicable within some institutions, most hospitals have only a limited number of practitioners with a limited amount of time to perform these studies. When an RCC is diagnosed, CT is required for staging of the chest and abdomen. So in the case of probable malignant lesions found on unenhanced US or other modalities, a tri-phasic CT examination will allow characterisation of the lesion at the same time as completing staging. This will avoid duplicating workload (CEUS then staging CT scan) when resources are limited.
A more practical remit for CEUS would be the further assessment of minimally complex cysts, for example those with low-level echoes or thin septa on standard sonography or high-density lesions seen on CT. Absent or minimal microbubble enhancement would allow these lesions to be confidently categorised as benign. CEUS can also reasonably be used to follow-up Bosniak IIF lesions, avoiding the need for multiple CTs and the inherent radiation burden this entails. Finally, one paper14 has suggested the use of CEUS to characterise small renal cystic lesions. These can pose a problem because enhancement is often difficult to appreciate on CT due to their size and the partial volume effect. The improved spatial resolution and sensitivity for enhancement provided by CEUS can allow more accurate characterisation.
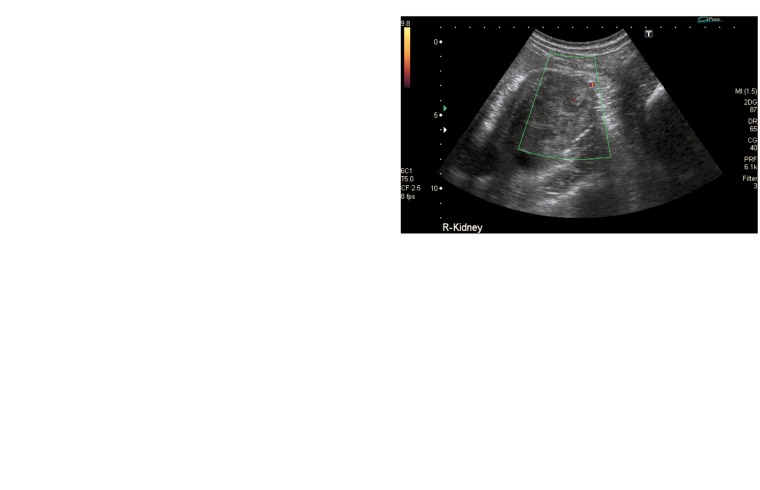
Renal ischaemia
Renal infarction is encountered infrequently in general radiological practice, and is often missed.33 It can be suspected by a history of unexplained flank pain and risk factors for thromboembolism (for example atrial fibrillation or prosthetic heart valve). Whilst contrast enhanced CT is likely to remain the modality of choice for investigating these patients with non-specific or unexplained abdominal pain, some will not be candidates for this test, particularly those with accompanying renal impairment. CEUS has been shown to be of comparable accuracy to CT in diagnosing renal infarction,33 and is much more accurate than B-mode and Doppler US alone. In addition, the excellent spatial resolution of CEUS allows for accurate differentiation between infarction and cortical necrosis. Renal infarction appears on CEUS as a wedge-shaped area of non-perfusion; cortical necrosis appears similar but with preserved hilar vascularity (Figure 5).34 These two entities have different aetiologies, and therefore CEUS could provide focus for further investigation. Whilst the setting of ischaemia might be an uncommon indication for the use of the technique, it is worth considering when the history is suggestive and CT is not available. It is likely to be more straightforward than other modalities such as MRI.
Figure 5.
Cortical necrosis. The low MI grey-scale image (to the right) demonstrates mildly increased cortical echogenicity of the right kidney. The CEUS image demonstrates no cortical perfusion but preserved enhancement of the sinus, features in keeping with cortical necrosis.
Renal infection
US scans are frequently performed for patients with pyelonephritis that fails to settle with antibiotics. The goal of these scans is to exclude an obstructed collecting system and to assess for complications. Chief amongst these is abscess formation. The EFSUMB guidelines2 suggest that CEUS can be used to assess for complications if the patient remains febrile after 72 hours. They admit that evidence for this is limited and is based largely on expert opinion. Renal abscesses appear as rounded, hypoechoic lesions. They may contain internal debris. They demonstrate no enhancement with microbubble use. Crucially, they contain no internal vascularity, as this is destroyed by the liquefactive necrosis.34 Presence of vessels should lead the practitioner to consider alternative diagnoses. These features may allow a more confident diagnosis of abscess to be made than with the use of B-mode and Doppler imaging alone. There is also evidence to suggest that CEUS is as good as CT at diagnosing uncomplicated pyelonephritis.35 CEUS demonstrates focal pyelonephritis as a wedge-shaped region of hypoperfusion on both longitudinal and axial sections.35 The role of imaging in uncomplicated pyelonephritis does, however, remain dubious and on the current evidence it is difficult to justify the use of CEUS regularly.
Targeted renal ablation (radiofrequency and cryotherapy); guidance and follow-up
For patients unfit for resection of renal malignancies or with multiple tumours, RFA and cryotherapy provide an alternative management strategy. This involves inserting a needle into a lesion under image guidance, followed by heating or freezing of the tumour to achieve cell death. The EFSUMB guidance2 recommends its use when performing US-guided RFA. It can improve the localisation of lesions which are inconspicuous on standard ultrasound.2 It can also be employed in the follow-up of patients whom have had RFA or cryotherapy, as long as CEUS has been performed prior to the ablation (Figure 6). On follow-up imaging with CEUS, residual tumour appears nodular or crescent like.36 False positives can occur when peripheral vessels are misinterpreted as tumour, but these can be distinguished by their more linear appearance. In general, residual tumour should have similar enhancement characteristics as on the preablation imaging. Careful comparison between the two studies is therefore paramount to avoid mistakes.
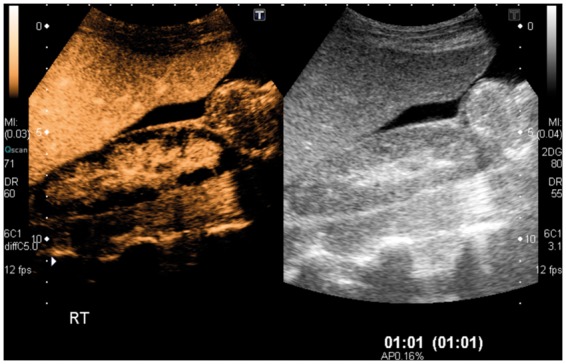
Figure 6.
Cryotherapy. (a) Preablative CEUS image demonstrates a slightly heterogeneously enhancing mass in the lower pole of the right kidney. (b) Postcryoablation CEUS demonstrates avascularity of the target region which is seen on the low MI grey-scale image (to the right) as a residual cystic area.
Other potential uses
The above described indications represent the entirety of those recommended by EFSUMB. The use of renal CEUS in other situations is more difficult to justify with the current evidence, but we include two where there is mounting evidence of the benefits of CEUS.
Trauma
In the setting of trauma, CEUS demonstrates parenchymal injuries as focal defects of perfusion.34 It can identify lacerations and also renal arterial transection and thrombosis, which are seen as an absence of parenchymal perfusion. Active haemorrhage may also be observed at the time of scanning. Its use in this setting is limited by its inability to image the collecting system (being a purely intravascular agent that is not filtered by the kidney). In addition, it cannot provide an adequate assessment of bowel, the retroperitoneum, the thorax or bones14 and, therefore, CT remains the modality of choice for acute traumatic injury. CEUS should be used sparingly, perhaps only in the follow-up of injuries or in the rare circumstances when CT is unavailable or contraindicated.
Transplant kidneys
For transplant kidneys, B-mode and Doppler US remain the imaging modality of choice. CEUS in these patients may one day allow assessment of vascular dynamics to predict graft success and failure.2 Within the clinical imaging world of today, CEUS helps as a problem solving tool when the standard B-mode and Doppler assessment of a renal transplant proves inconclusive. Patients who have recently had a transplant can be difficult to image, and the angle dependence of Doppler imaging can make assessment of the vasculature challenging. CEUS can improve the conspicuity of vessels in these circumstances as it is not angle dependent.
Of course, all of the focal lesions described above can manifest in transplanted as well as native kidneys. It could be argued that the use of CEUS in this patient cohort over alternative modalities such as CT is even more important than in the general population due to the lack of nephrotoxicity associated with microbubbles.
Conclusion
CEUS in the kidneys is an inexpensive and effective imaging modality. It is accurate in characterising indeterminate lesions, complex cysts and infective pathology. It provides excellent imaging of the renal vasculature and accurately characterises focal infarction and cortical necrosis. It can be used when there are contraindications to CT or MRI and in many cases, it offers significant advantages over these other modalities; there is no exposure to ionising radiation, it is more sensitive to contrast enhancement in hypoperfused masses and there is no requirement for potentially nephrotoxic contrast agents. It is quick to perform and can often be undertaken immediately following an equivocal conventional US scan, obviating the need to recall the patient and reducing unnecessary anxiety.
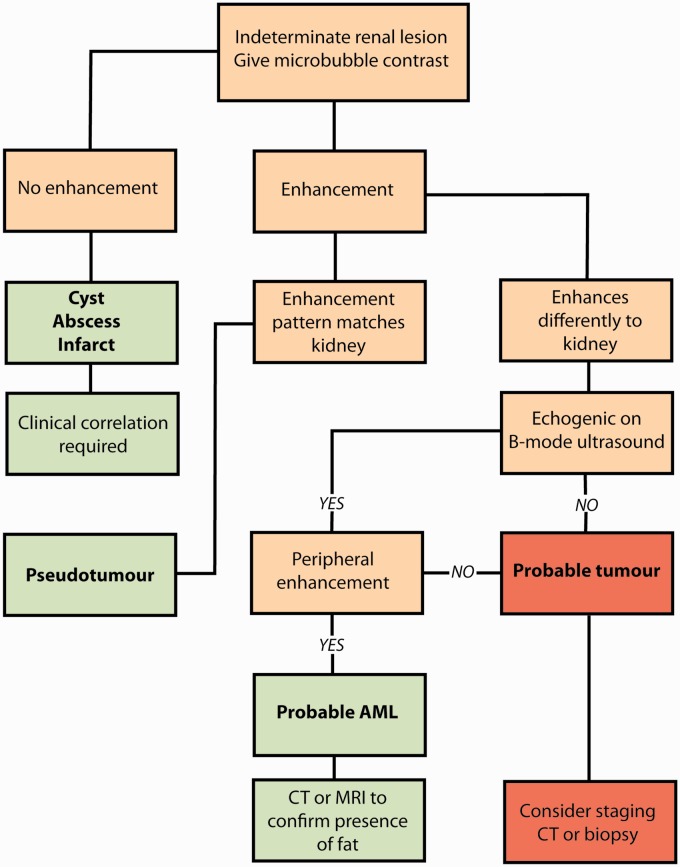
Our experience is that CEUS is not a difficult technique to learn, and for practitioners already familiar with performing CEUS in the liver, evaluating renal lesions will not present a great challenge. Unlike the liver, where the timing of enhancement and washout of contrast must be assessed, the decision making when assessing renal lesions with CEUS is very simple and essentially consists of only two questions: does the lesion enhance, and if it does, does it enhance homogenously with the remainder of the kidney? This forms the basis of the simple flowchart (Figure 7) that we have designed to allow the reader to consider how they might approach an indeterminate renal lesion with CEUS. The authors find it an invaluable problem solving tool in the assessment of renal lesions which significantly improves the diagnostic accuracy of US and rivals that of CT and MRI when used appropriately.
Figure 7.
Suggested flow diagram for assessing indeterminate renal lesions using CEUS.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Not applicable.
Guarantor
SCT.
Contributorship
SCT researched literature for this review article. SCT wrote the first draft of the manuscript. Both authors sourced images for the article. Both authors wrote and approved the final version of the manuscript.
References
- 1.Nicolau C, Buñesch L, Paño B, et al. Prospective evaluation of CT indeterminate renal masses using US and contrast-enhanced ultrasound. Abdom Imaging 2015; 40: 542–551. [DOI] [PubMed] [Google Scholar]
- 2.Piscaglia F, Nolsøe C, Dietrich C, et al. The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 2011; 33: 33–59. [DOI] [PubMed] [Google Scholar]
- 3.2020 Delivery (commissioned by Cancer Research UK). Horizon Scanning. An evaluation of imaging capacity across the NHS in England. https://www.cancerresearchuk.org/sites/default/files/horizon_scanning_exec_sum_final.pdf (accessed 2 November 2015).
- 4.Department of Health. Diagnostic imaging dataset annual statistical release 2014/15, www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2014/11/Annual-Statistical-Release-2014-15-DID-PDF-1.1MB.pdf (accessed 15 December 2015).
- 5.Hollingsworth JM, Miller DC, Daignault S, et al. Rising incidence of small renal masses: a need to reassess treatment effect. J Natl Cancer Inst 2006; 98: 1331–1334. [DOI] [PubMed] [Google Scholar]
- 6.Cancer Research UK. Kidney cancer incidence statistics, www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/kidney-cancer/incidence (accessed 15 December 2015).
- 7.Nanda NC. History of echocardiographic contrast agents. Clin Cardiol 1997; 20(S1): 7–11. [DOI] [PubMed] [Google Scholar]
- 8.Newland A, et al. SonoVue (sulphur hexafluoride microbubbles) – contrast agent for contrast-enhanced ultrasound imaging of the liver. NICE diagnostic guidance [DG5], www.nice.org.uk/Guidance/DG5 (accessed 2 November 2015).
- 9.Medicines.org.uk. SonoVue 8 microlitres/ml, powder and solvent for dispersion for injection – summary of product characteristics (SPC) – (eMC), www.medicines.org.uk/emc/medicine/7777 (accessed 20 October 2015).
- 10.Quaia E. Microbubble ultrasound contrast agents: an update. Eur Radiol 2007; 17: 1995–2008. [DOI] [PubMed] [Google Scholar]
- 11.Piscaglia F, Bolondi L. The safety of Sonovue® in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol 2006; 32: 1369–1375. [DOI] [PubMed] [Google Scholar]
- 12.Ellis J, et al. ACR Manual on Contrast Media Version 10.1, www.acr.org/quality-safety/resources/contrast-manual (accessed 20 October 2015).
- 13.ter Haar G. Safety and bio-effects of ultrasound contrast agents. Med Biol Eng Comput 2009; 47: 893–900. [DOI] [PubMed] [Google Scholar]
- 14.Harvey C, Alsafi A, Kuzmich S, et al. Role of US contrast agents in the assessment of indeterminate solid and cystic lesions in native and transplant kidneys. Radiographics 2015; 35: 1419–1430. [DOI] [PubMed] [Google Scholar]
- 15.Harvey C, Sidhu P. Ultrasound contrast agents in genitourinary imaging. Ultrasound Clin 2010; 5: 489–506. [Google Scholar]
- 16.EFSUMB. Minimum training requirements for the practice of medical ultrasound in Europe. Ultraschall Med 2010; 31: 426–427. [DOI] [PubMed] [Google Scholar]
- 17.Jonisch A, Rubinowitz A, Mutalik P, et al. Can high-attenuation renal cysts be differentiated from renal cell carcinoma at unenhanced CT? Radiology 2007; 243: 445–450. [DOI] [PubMed] [Google Scholar]
- 18.Tamai H, Takiguchi Y, Oka M, et al. Contrast-enhanced ultrasonography in the diagnosis of solid renal tumors. J Ultrasound Med 2005; 24: 1635–1640. [DOI] [PubMed] [Google Scholar]
- 19.Onishi T, Oishi Y, Goto H, et al. Histological features of hypovascular or avascular renal cell carcinoma: the experience at four university hospitals. Int J Clin Oncol 2002; 7: 159–164. [DOI] [PubMed] [Google Scholar]
- 20.Ascenti G, Mazziotti S, Zimbaro G, et al. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology 2007; 243: 158–165. [DOI] [PubMed] [Google Scholar]
- 21.Park BK, Kim B, Kim SH, et al. Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol 28; 61: 310–314. [DOI] [PubMed]
- 22.Toshiba Medical Systems Corporation. Ultrasound (seeing the unseen with superb micro-vascular imaging(SMI)), www.toshibamedicalsystems.com/products/us/aplio_smi.html (accessed 20 October 2015).
- 23.Correas J, Claudon M, Tranquart F, et al. The kidney: imaging with microbubble contrast agents. Ultrasound Q 2006; 22: 53–66. [PubMed] [Google Scholar]
- 24.Mazziotti S, Zimbaro F, Pandolfo A, et al. Usefulness of contrast-enhanced ultrasonography in the diagnosis of renal pseudotumors. Abdom Imaging 2009; 35: 241–245. [DOI] [PubMed] [Google Scholar]
- 25.Park B, Kim B, Kim S, et al. Assessment of cystic renal masses based on Bosniak classification: comparison of CT and contrast-enhanced US. Eur J Radiol 2007; 61: 310–314. [DOI] [PubMed] [Google Scholar]
- 26.Quaia E, Bertolotto M, Cioffi V, et al. Comparison of contrast-enhanced sonography with unenhanced sonography and contrast-enhanced CT in the diagnosis of malignancy in complex cystic renal masses. Am J Roentgenol 2008; 191: 1239–1249. [DOI] [PubMed] [Google Scholar]
- 27.Bosniak M. The Bosniak renal cyst classification: 25 years later. Radiology 2012; 262: 781–785. [DOI] [PubMed] [Google Scholar]
- 28.Xue L, Lu Q, Huang B, et al. Contrast-enhanced ultrasonography for evaluation of cystic renal mass: in comparison to contrast-enhanced CT and conventional ultrasound. Abdom Imaging 2014; 39: 1274–1283. [DOI] [PubMed] [Google Scholar]
- 29.Barr R, Peterson C, Hindi A. Evaluation of indeterminate renal masses with contrast-enhanced US: a diagnostic performance study. Radiology 2014; 271: 133–142. [DOI] [PubMed] [Google Scholar]
- 30.Xu ZF, Xu HX, Xie XY, et al. Renal cell carcinoma and renal angiomyolipoma differential diagnosis with real-time contrast-enhanced ultrasonography. J Ultrasound Med 2010; 29: 709–717. [DOI] [PubMed] [Google Scholar]
- 31.Ascenti G, Gaeta M, Magno C, et al. Contrast-enhanced second-harmonic sonography in the detection of pseudocapsule in renal cell carcinoma. Am J Roentgenol 2004; 182: 1525–1530. [DOI] [PubMed] [Google Scholar]
- 32.Nicolau C, Bunesch L, Sebastia C. Renal complex cysts in adults: contrast-enhanced ultrasound. Abdom Imaging 2011; 36: 742–752. [DOI] [PubMed] [Google Scholar]
- 33.Bertolotto M, Martegani A, Aiani L, et al. Value of contrast-enhanced ultrasonography for detecting renal infarcts proven by contrast enhanced CT. A feasibility study. Eur Radiol 2007; 18: 376–383. [DOI] [PubMed] [Google Scholar]
- 34.Bertolotto M, Catalano O. Contrast-enhanced ultrasound: past, present, and future. Ultrasound Clin 2009; 4: 339–367. [Google Scholar]
- 35.Mitterberger M, Pinggera G, Colleselli D, et al. Acute pyelonephritis: comparison of diagnosis with computed tomography and contrast-enhanced ultrasonography. BJU Int 2008; 101: 341–344. [DOI] [PubMed] [Google Scholar]
- 36.Hoeffel C, Pousset M, Timsit M, et al. Radiofrequency ablation of renal tumours: diagnostic accuracy of contrast-enhanced ultrasound for early detection of residual tumour. Eur Radiol 2010; 20: 1812–1821. [DOI] [PubMed] [Google Scholar]