Abstract
Patients admitted to UK hospitals with community-acquired pneumonia (CAP) require a chest radiograph for diagnostic purposes and to look for complications. This study investigated the association between a chest radiograph performed early in the process of care and clinical outcomes. Consecutive adults admitted with CAP to a large UK teaching hospital trust over a nine-month period were prospectively studied (n = 461). A time to first radiograph of <4 hours was associated with a significantly shorter median length of hospital stay (LOS) compared with ≥4 hours (5.75 days versus 7.13 days, p<0.01). Antibiotics were administered after the radiograph in 89.8% of patients with a time to first radiograph <4 hours compared with 40.7% of patients with time to first radiograph of ≥4 hours (odds ratio 12.8, p<0.001). A chest radiograph performed within four hours of hospital admission for CAP is significantly associated with a shorter hospital LOS and with antibiotic use after chest radiography.
Key Words: chest X-rays, pneumonia, process of care, respiratory infection
Introduction
Community-acquired pneumonia (CAP) is a cause of substantial and long-term mortality and morbidity,1–3 and the number of patients admitted annually to hospital is increasing.4–6 In recent years controversy has surrounded the prognostic benefit conferred by early antibiotic treatment of CAP on arrival to hospital. A short time to first antibiotic dose (TFA) for patients hospitalised with CAP was initially suggested to decrease mortality7,8 and later hospital length of stay (LOS),9–11 findings which have since been vigorously disputed.12–18 A number of reports have also been published showing an increase in both the CAP misdiagnosis rate and the proportion of patients inappropriately administered antibiotics following the introduction of clinical care pathways advocating a short TFA in all patients with suspected CAP.19–21
International guidelines recommend that CAP be definitively diagnosed with the use of a chest radiograph.22,23 Early diagnosis is desirable for a number of reasons. It facilitates a confident, appropriate management approach and the early use of appropriate antibiotics and severity scoring. It should also prevent the over-diagnosis or misdiagnosis of CAP based on clinical signs alone.24–26 The British Thoracic Society has recently recommended that a diagnostic chest radiograph should be performed in patients admitted with suspected CAP as promptly as possible following admission (preferably within four hours) and that antibiotics should be administered as soon as possible after radiographic confirmation of CAP.23 However, to the authors' knowledge, there are no published data demonstrating that early diagnosis of CAP as measured by time to first chest radiograph (TXR) is associated with improved clinical outcome.
The aim of this study was to determine whether a short TXR in patients hospitalised with CAP is associated with shorter hospital LOS and more appropriate timing of antibiotic administration in relation to chest radiography.
Methods
Patient data
Patients with CAP were prospectively enrolled within one large UK teaching hospital trust between September 2008 and June 2009. Patients were included in the study if they were aged more than 16 years, had at least one acute symptom in keeping with a lower respiratory tract infection (breathlessness, cough, sputum or fever), had new infiltrates on a chest radiograph, and were treated by the admitting team for CAP. Patients were excluded if they had been admitted to hospital in the preceding 10 days, had tuberculosis, were admitted from a nursing home, or had post-obstructive pneumonia due to lung cancer. Participants were identified by the investigators on a daily basis from the acute admitting medical wards, and enrolled following a diagnostic admission chest radiograph. Route of admission was either via referral from primary care or following assessment in the emergency department. All patients were managed in a similar manner according to trust CAP guidelines, at the discretion of the attending clinician.
Data collected included patient demographics, symptoms and observations, pneumonia severity (as measured by CURB-6527), co-morbidity, and dates and times of admission, discharge, first antibiotic administration, and first chest radiograph. Admission and baseline functional status were estimated using the World Health Organization performance status scoring system.28 Admission performance status was determined by the study investigators, whereas baseline performance status was estimated from patient descriptions of their functional status prior to the onset of disease. The time of first chest radiograph was retrieved from the radiology department's computerised records (all chest radiographs are digitally stored together with the exact timing of the investigation). All chest radiographs were reviewed by the duty radiologist, and patients were excluded if the reports were not in keeping with CAP. The time of first antibiotic administration was prospectively determined by drug chart review during the admitting episode (the exact timing of first antibiotic dose is usually recorded by the healthcare professional administrating the drug(s)). The TXR and the TFA were defined as the time from arrival at the hospital to first chest radiograph and to first antibiotic dose respectively. Follow-up of patients occurred between six and eight weeks after hospital discharge.
Ethical approval for this study was granted by the Nottingham regional ethics committee and informed consent was obtained from study participants in accordance with the ethics committee recommendations.
Data analysis and statistical considerations
The primary outcome measure was hospital LOS, and the secondary outcome measures were:
timing of antibiotic administration in relation to chest radiography
30-day mortality
30-day readmission rates.
Thirty-day mortality was ascertained from computerised hospital records, and was defined as death within 30 days of admission and readmission was defined as readmission to hospital for any reason within 30 days of discharge.
For the analyses of TXR and TFA in relation to outcome, data for TXR and TFA were converted to categorical variables using four hours as the threshold value. This threshold value was chosen to reflect the ‘four-hour target’ of admission to treatment that is applied to all acute medical admissions in England and Wales. All non-normally distributed continuous data were transformed logarithmically prior to statistical analysis with the Student's t test. Categorical data were analysed using Pearson's χ2 test, or Fisher's exact test if sample sizes were small. All analyses involving LOS excluded those that had died prior to hospital discharge.
A sample size of 500 patients would have 80% power to detect a fall in LOS of 1.26 days with a significance level of 5%. Assuming a mortality of 15% within the same population, a mortality difference of 7% would be required to achieve statistical significance with 80% power.
Results
Patient characteristics
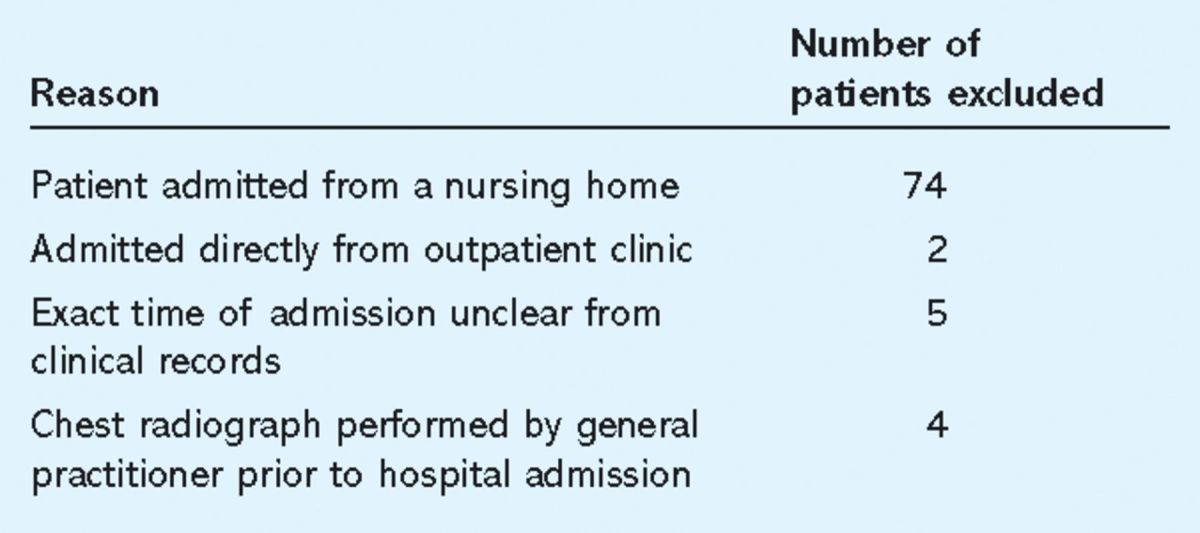
Five hundred and forty-six patients were enrolled. Eighty-five patients were excluded for a variety of reasons (Table 1), leaving 461 for analysis. Of these, 64 died in hospital and were not analysed for LOS. The median age of the study cohort was 72 years (range 17–102 years) and 60.7% were male. Median LOS for the entire cohort was 6.59 days (interquartile range (IQR) 9.45 days), mortality was 13.7%, and readmission rate was 16.2% for those patients who survived to discharge. Median TXR was 1.91 hours (IQR 3.60 hours), with 333 (72.2%) radiographs performed within four hours of admission and 236 (51.2%) within two hours. 49.8% patients received both their chest radiograph and antibiotics within four hours of arrival to hospital. For 35 patients there was uncertainty in the medical records regarding the exact time the first dose of antibiotic was administered, and these patients were therefore excluded from any analyses relating to TFA.
Table 1.
Distribution and explanation of patients excluded from analysis.
Comparison of groups
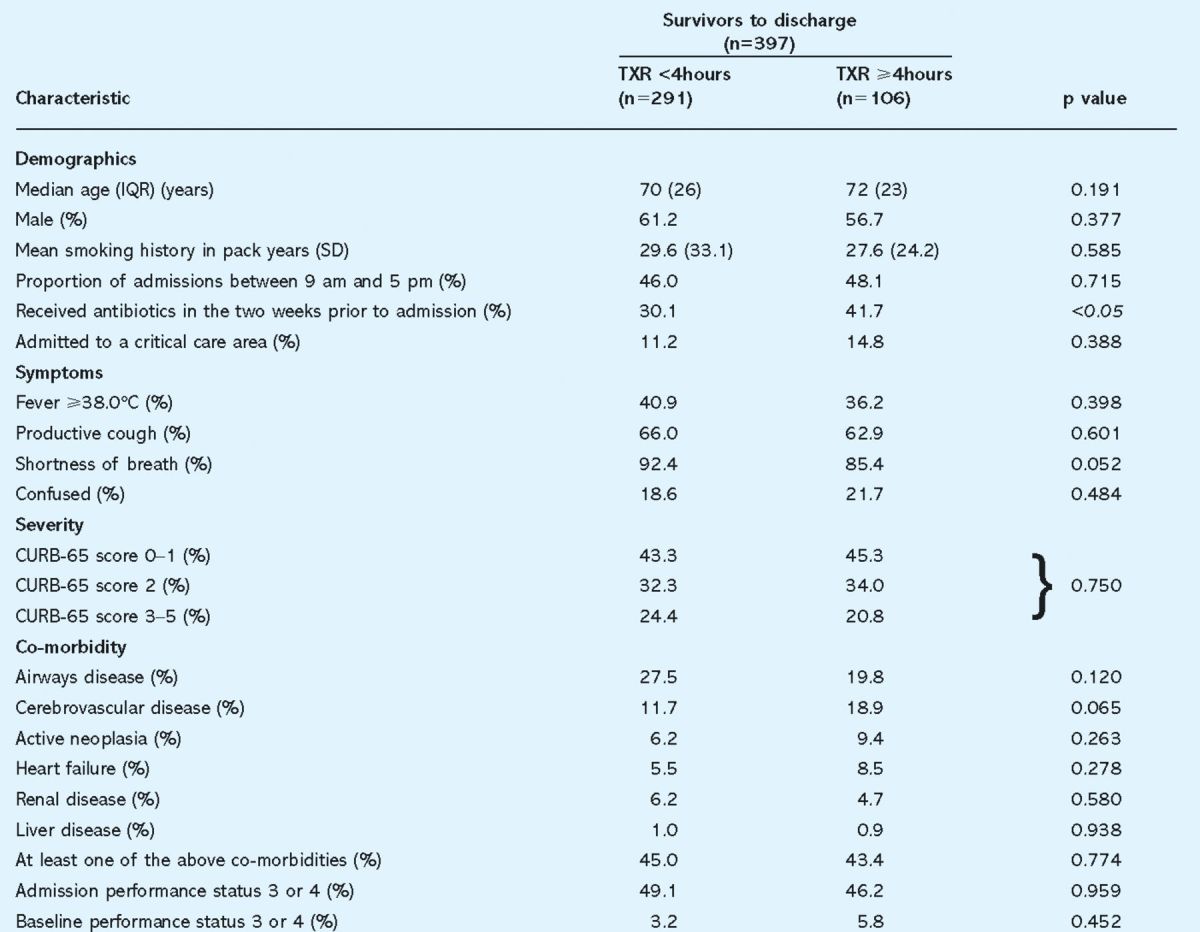
No differences in age, sex, performance status or co-morbidity were found between patients with TXR ≥4 hours and TXR <4 hours (Table 2). Patients with a TXR <4 hours were more likely to be short of breath (92.4% ν 85.4%, p = 0.052, odds ratio (OR) 2.1), but in other respects the prevalence of lower respiratory tract symptoms was not statistically different between these groups. There was a significantly lower rate of antibiotic use in the two weeks prior to hospital admission in patients with TXR <4 hours (30.1% ν 41.7%, p<0.05). Patients with more severe disease (CURB-65 3–5) had a significantly shorter median TXR and TFA compared to patients with low severity CAP (CURB-65 0–1) (for TXR: 1.55 hours ν 2.01 hours, p<0.05; for TFA: 2.80 hours ν 3.67 hours, p<0.05). However, no difference in disease severity was noted between groups according to TXR of greater or less than four hours.
Table 2.
Characteristics of patients admitted to hospital with community-acquired pneumonia who survived to discharge according to time from admission to first chest radiograph (TXR). Symptom data exclude those patients who were unable to communicate at admission. IQR = interquartile range; SD = standard deviation.
Outcome measures
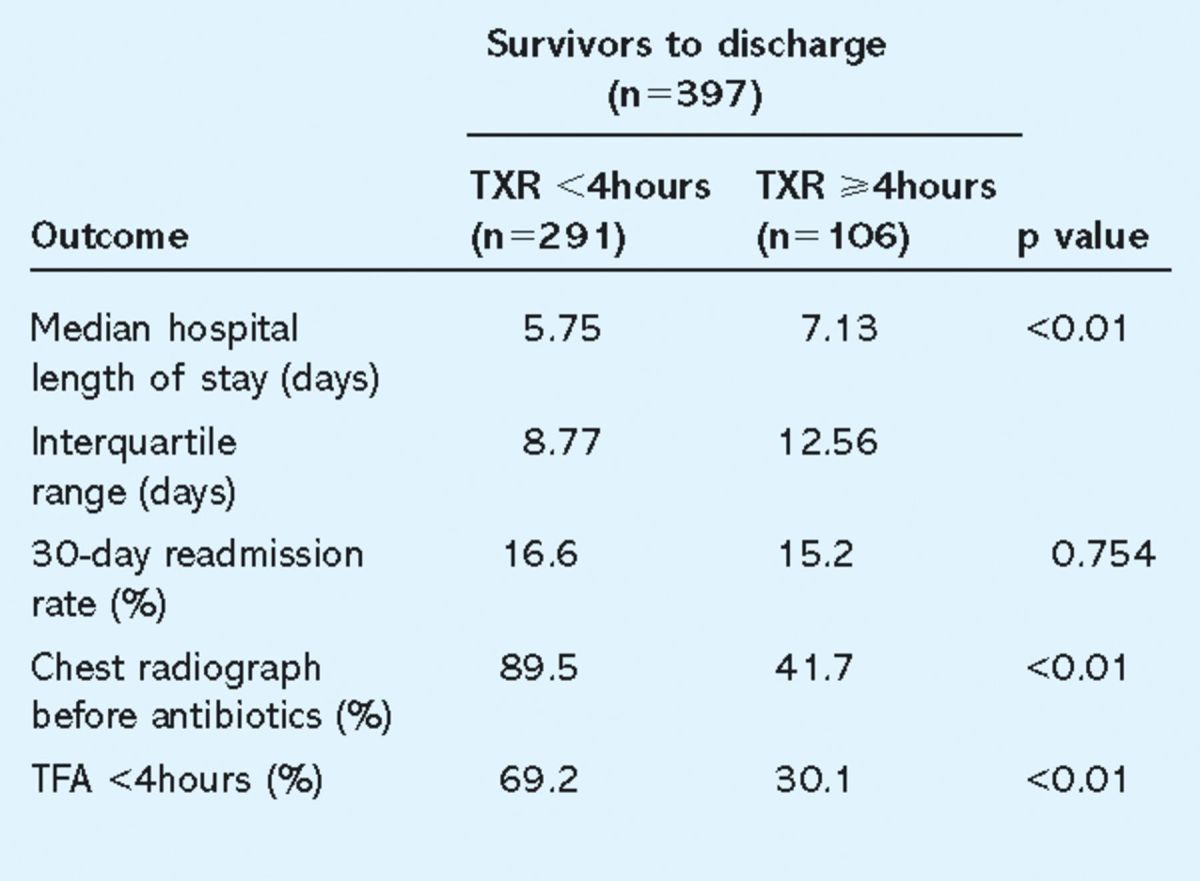
Median LOS was significantly shorter for patients with a TXR <4 hours compared to TXR ≥4 hours (5.75 days ν 7.13 days, p<0.01) (Table 3) and TFA <4 hours compared to TFA ≥4 hours (5.63 days ν 8.07 days, p<0.01). Forty-four (9.5%) patients were hypotensive on admission (systolic blood pressure <90 mmHg). As these patients might have been treated differently from the others, a subanalysis was performed with these patients excluded. In this subanalysis, the association of TXR <4 hours with a reduced median LOS was maintained (5.63 days ν 7.01 days, p<0.01). Antibiotics were administered after the radiograph (rather than vice versa) in significantly more patients with a TXR <4 hours compared to patients with TXR ≥4 hours (89.8% ν 40.7%, OR 12.8, p<0.001).
Table 3.
Comparison of outcome according to time to first chest radiograph. TFA = time to first antibiotic dose; TXR = time from admission to first chest radiograph.
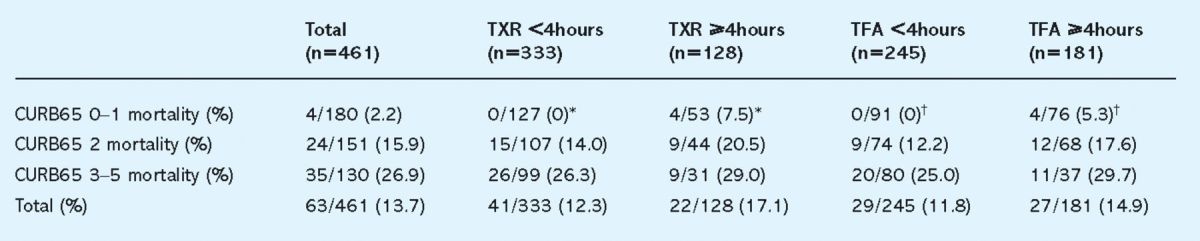
No statistically significant association was observed between 30-day mortality and TXR or TFA <4 hours, although there was a trend towards a lower mortality in both groups (Table 4). Of patients who had low severity CAP (CURB-65 of 0 or 1), four (7.5%) deaths at 30 days were noted in those with TXR ≥4 hours compared to no deaths in those who had both a TXR <4 hours (p<0.01). Having a chest radiograph before antibiotic administration was not associated with a decrease in mortality.
Table 4.
Association of mortality with time to chest radiograph or antibiotic administration, stratified by pneumonia severity. TFA = time to first antibiotic delivery; TXR = time from admission to first chest radiograph; ∗, = p < 0.05, Fisher's exact test.
Discussion
The main finding of this study is that a TXR of less than four hours is associated with a shorter hospital LOS. A decrease in median LOS of just over a day may seem like a modest figure, but it has been shown that with a condition as common as CAP, small changes in LOS can result in substantial cost benefits nationally.29 Furthermore, significantly more patients received antibiotics after chest radiography if the chest radiograph was performed within four hours of admission rather than beyond four hours.
The link between early chest radiography and length of stay
This is the first paper to the authors' knowledge to demonstrate that TXR is associated with benefits in terms of clinical outcome. There are several potential explanations for this finding. There may be clinical factors that have not been controlled for which are affecting both TXR and LOS, such as higher clinical complexity of patients producing delays in care processes including subsequent hospital discharge. However, no differences were observed between the early and late TXR groups in terms of the presence of co-morbidities, performance status and disease severity. An alternative explanation is that an early chest radiograph is a surrogate marker of quality of care in the management of CAP. This complements a previous study which suggested that prompt diagnostic assessment as measured by early oxygenation assessment for CAP was associated with better quality of care and consequently improved outcomes.30
Benefits of a strategy advocating early chest radiograph rather than early antibiotics
This study supports the findings from previous reports that an early antibiotic strategy for CAP is associated with a shorter hospital LOS.10 Unfortunately, an emphasis on early antibiotic delivery as a quality measure has been shown to encourage admitting teams to over-diagnose CAP and over-prescribe antibiotics.19,20 Such inappropriate administration of broad spectrum antibiotics can cause considerable harm, including the promotion of antibiotic resistance and antibiotic-associated complications, such as Clostridium difficile infection. There is also a significant group of patients presenting to acute services for whom the diagnosis of CAP is equivocal when based on clinical features and basic investigations alone.15
On the other hand, a management strategy based on early radiological diagnosis for patients admitted with suspected CAP followed by antibiotic treatment not only provides greater diagnostic accuracy and promotes a more informed approach to patient management, but also potentially enables a reduction in antibiotic use where the diagnosis of CAP is not substantiated by chest radiography. This approach would improve antibiotic stewardship and limit the inappropriate use of antibiotics.
Factors influencing time to chest radiograph
There are several factors which might influence how rapidly a patient arriving at hospital receives a chest radiograph. A previous study demonstrated a shorter TFA in patients with severe pneumonia as defined by a high pneumonia severity index score.13 The current study replicated this finding and also revealed a similar effect on TXR. Resource issues, such as nurse and doctor availability, and number and timing of patient admissions may also have an impact on TXR. These issues are harder to assess quantitatively. In this study, no difference in the proportion of patients with a short TXR was noted in those admitted out of hours compared with those admitted during working hours (9 am to 5 pm). This is an incomplete surrogate measure of resource issues and further research is warranted in this area.
Study criticisms
The main criticism of this study is the possibility that the differences found in LOS were confounded by other undocumented variables. Early and late TXR groups have been compared by several clinical variables including presenting symptoms, CAP severity, functional status and co-morbidity. The only differences found between the groups were a higher proportion of patients with TXR ≥4 hours receiving antibiotics in the community prior to admission, and a borderline lower frequency of breathlessness as a presenting symptom. Nevertheless, there remains a possibility of incomplete adjustment for disease severity and/or other clinical factors.
Length of stay is a less robust end point compared with mortality and may be confounded by other process of care factors, such as delays in organising social care. The exclusion of patients admitted from nursing homes who generally have greater social needs would have reduced the impact of social care factors. Nevertheless, residual confounding cannot be completely discounted.
As indicated by the sample size calculations, the study cohort was insufficiently large to demonstrate a mortality benefit. Although a trend towards a lower mortality was demonstrated for patients with TXR <4 hours, a much larger dataset would be required in order to detect a statistically significant difference, if present.
Conclusion
A chest radiograph performed within four hours of hospital admission for CAP is significantly associated with a shorter hospital LOS and antibiotic administration after chest radiography. It may represent a useful process of care marker in the management of CAP.
References
- 1.Capelastegui A, España PP, Quintana JM, et al. Development of a prognostic index for 90-day mortality in patients discharged after admission to hospital for community-acquired pneumonia. Thorax 2009;64:496–501. 10.1136/thx.2008.098814 [DOI] [PubMed] [Google Scholar]
- 2.Ewig S, Birkner N, Strauss R, et al. New perspectives on community-acquired pneumonia in 388,406 patients. Results from a nationwide mandatory performance measurement programme in healthcare quality. Thorax 2009;64:1062–9. 10.1136/thx.2008.109785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myles PR, McKeever TM, Pogson Z, Smith CJP, Hubbard RB. The incidence of pneumonia using data from a computerized general practice database. Epidemiol Infect 2009;137:709–16. 10.1017/S0950268808001428 [DOI] [PubMed] [Google Scholar]
- 4.Trotter CL, Stuart JM, George R, Miller E. Increasing hospital admissions for pneumonia, England. Emerg Infect Dis 2008;14:727–33. 10.3201/eid1405.071011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA 2005;294:2712–19. 10.1001/jama.294.21.2712 [DOI] [PubMed] [Google Scholar]
- 6.Thomsen RW, Riis A, Nørgaard M, et al. Rising incidence and persistently high mortality of hospitalized pneumonia: a 10-year population-based study in Denmark. J Intern Med 2006;259:410–17. 10.1111/j.1365-2796.2006.01629.x [DOI] [PubMed] [Google Scholar]
- 7.Houck PM, Bratzler DW, Nsa W, Ma A, Bartlett JG. Timing of antibiotic administration and outcomes for Medicare patients hospitalized with community-acquired pneumonia. Arch Intern Med 2004;164:637–44. 10.1001/archinte.164.6.637 [DOI] [PubMed] [Google Scholar]
- 8.Meehan TP, Fine MJ, Krumholz HM, et al. Quality of care, process, and outcomes in elderly patients with pneumonia. JAMA 1997;278:2080–4. [PubMed] [Google Scholar]
- 9.Berjohn CM, Fishman NO, Joffe MM, Edelstein PH, Metlay JP. Treatment and outcomes for patients with bacteremic pneumococcal pneumonia. Medicine (Baltimore) 2008;87:160–6. 10.1097/MD.0b013e318178923a [DOI] [PubMed] [Google Scholar]
- 10.Battleman DS, Callahan M, Thaler HT. Rapid antibiotic delivery and appropriate antibiotic selection reduce length of hospital stay of patients with community-acquired pneumonia: link between quality of care and resource utilization. Arch Intern Med 2002;162:682–8. 10.1001/archinte.162.6.682 [DOI] [PubMed] [Google Scholar]
- 11.Huang JQ, Hooper PM, Marrie TJ. Factors associated with length of stay in hospital for suspected community-acquired pneumonia. Can Respir J 2006;13:317–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu KT, Wyer PC. Evidence-based emergency medicine/critically appraised topic. Evidence behind the 4-hour rule for initiation of antibiotic therapy in community-acquired pneumonia. Ann Emerg Med 2008;51:651–62, 662.e1–2. [DOI] [PubMed] [Google Scholar]
- 13.Cheng AC, Buising KL. Delayed administration of antibiotics and mortality in patients with community-acquired pneumonia. Ann Emerg Med 2009;53:618–24. 10.1016/j.annemergmed.2008.07.017 [DOI] [PubMed] [Google Scholar]
- 14.Silber SH, Garrett C, Singh R, et al. Early administration of antibiotics does not shorten time to clinical stability in patients with moderate-to-severe community-acquired pneumonia. Chest 2003;124:1798–804. 10.1378/chest.124.5.1798 [DOI] [PubMed] [Google Scholar]
- 15.Waterer GW, Kessler LA, Wunderink RG. Delayed administration of antibiotics and atypical presentation in community-acquired pneumonia. Chest 2006;130:11–5. 10.1378/chest.130.1.11 [DOI] [PubMed] [Google Scholar]
- 16.Dedier J, Singer DE, Chang Y, Moore M, Atlas SJ. Processes of care, illness severity, and outcomes in the management of community-acquired pneumonia at academic hospitals. Arch Intern Med 2001;161:2099–104. 10.1001/archinte.161.17.2099 [DOI] [PubMed] [Google Scholar]
- 17.Barlow G, Nathwani D, Williams F, et al. Reducing door-to-antibiotic time in community-acquired pneumonia: controlled before-and-after evaluation and cost-effectiveness analysis. Thorax 2007;62:67–74. 10.1136/thx.2005.056689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wachter RM, Flanders SA, Fee C, Pronovost PJ. Public reporting of antibiotic timing in patients with pneumonia: lessons from a flawed performance measure. Ann Intern Med 2008;149:29–32. [DOI] [PubMed] [Google Scholar]
- 19.Kanwar M, Brar N, Khatib R, Fakih MG. Misdiagnosis of community-acquired pneumonia and inappropriate utilization of antibiotics: side effects of the 4-h antibiotic administration rule. Chest 2007;131:1865–9. 10.1378/chest.07-0164 [DOI] [PubMed] [Google Scholar]
- 20.Welker JA, Huston M, McCue JD. Antibiotic timing and errors in diagnosing pneumonia. Arch Intern Med 2008;168:351–6. 10.1001/archinternmed.2007.84 [DOI] [PubMed] [Google Scholar]
- 21.Metersky ML, Sweeney TA, Getzow MB, et al. Antibiotic timing and diagnostic uncertainty in Medicare patients with pneumonia: is it reasonable to expect all patients to receive antibiotics within 4 hours?. Chest 2006;130:16–21. 10.1378/chest.130.1.16 [DOI] [PubMed] [Google Scholar]
- 22.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44(Suppl 2):S27–S72. 10.1086/511159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim WS, Baudouin SV, George RC, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 2009;64(Suppl 3):iii1–ii55. 10.1136/thx.2009.121434 [DOI] [PubMed] [Google Scholar]
- 24.Woodhead MA, Macfarlane JT, McCracken JS, Rose DH, Finch RG. Prospective study of the aetiology and outcome of pneumonia in the community. Lancet 1987;1:671–4. 10.1016/S0140-6736(87)90430-2 [DOI] [PubMed] [Google Scholar]
- 25.Wipf JE, Lipsky BA, Hirschmann JV, et al. Diagnosing pneumonia by physical examination: relevant or relic?. Arch Intern Med 1999;159:1082–7. 10.1001/archinte.159.10.1082 [DOI] [PubMed] [Google Scholar]
- 26.Metlay JP, Kapoor WN, Fine MJ. Does this patient have community-acquired pneumonia? Diagnosing pneumonia by history and physical examination. JAMA 1997;278:1440–5. [PubMed] [Google Scholar]
- 27.Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58:377–82. 10.1136/thorax.58.5.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–55. 10.1097/00000421-198212000-00014 [DOI] [PubMed] [Google Scholar]
- 29.Raut M, Schein J, Mody S, et al. Estimating the economic impact of a half-day reduction in length of hospital stay among patients with community-acquired pneumonia in the US. Curr Med Res Opin 2009;25:2151–7. 10.1185/03007990903102743 [DOI] [PubMed] [Google Scholar]
- 30.Blot SI, Rodriguez A, Solé-Violán J, et al. Effects of delayed oxygenation assessment on time to antibiotic delivery and mortality in patients with severe community-acquired pneumonia. Crit Care Med 2007;35:2509–14. 10.1097/01.CCM.0000287587.43801.9C [DOI] [PubMed] [Google Scholar]


