Key Points
Malnutrition is a common, under-recognised and undertreated condition in hospital patients
Disease-related malnutrition arises due to reduced dietary intake, malabsorption, increased nutrient losses or altered metabolic demands
Wide-ranging changes in physiological function occur in malnourished patients leading to increased rates of morbidity and mortality
Routine nutritional screening should be undertaken in all patients admitted to hospital using a validated tool such as the Malnutrition Universal Screening Tool
Healthcare costs are significantly increased in malnourished patients
The term ‘malnutrition’ has no universally accepted definition. It has been used to describe a deficiency, excess or imbalance of a wide range of nutrients, resulting in a measurable adverse effect on body composition, function and clinical outcome.1 Although malnourished individuals can be under- or overnourished, ‘malnutrition’ is often used synonymously with ‘undernutrition’, as in this article.
The size of the problem
Malnutrition is a common, under-recognised and undertreated problem facing patients and clinicians. It is both a cause and consequence of disease and exists in institutional care and the community. Approximately 5% of the UK population are underweight with a body mass index (BMI) below 20 kg/m2, although obese individuals who unintentionally lose weight and subsequently have a BMI within the normal range are also at risk of malnutrition. Other patients become at risk as a result of an acute event (eg small bowel infarction), leaving them unable to meet their metabolic requirements both in the short and longer term. The prevalence of malnutrition increases by at least twofold in the elderly and those with chronic disease, and threefold in individuals living in institutional care.2
The prevalence of malnutrition in UK hospitals reported over the last 15 years ranges from 13–40%, many patients seeing a further decline in their nutritional status during hospital admission.3 A large survey conducted by the British Association of Parenteral and Enteral Nutrition (BAPEN) in 2008 found that 28% of inpatients were at risk of malnutrition. The prevalence was higher in specific subpopulations: for example, 34% of all emergency admissions and 52% of admissions from care homes.4
Specific micronutrient deficiencies are also common, especially in the elderly: for example, folate deficiency has been described in 29% of the independent elderly population and 35% of those in institutional care.5
Causes of malnutrition
Malnutrition in developed countries is unfortunately still more common in situations of poverty, social isolation and substance misuse. However, most adult malnutrition is associated with disease and may arise due to:
reduced dietary intake
reduced absorption of macro- and/or micronutrients
increased losses or altered requirements
increased energy expenditure (in specific disease processes).2
Dietary intake
Probably the single most important aetiological factor in disease-related malnutrition is reduced dietary intake. This is thought to occur due to reductions in appetite sensation as a result of changes in cytokines, glucocorticoids, insulin and insulin-like growth factors.6 The problem may be compounded in hospital patients by failure to provide regular nutritious meals in an environment where they are protected from routine clinical activities, and where they are offered help and support with feeding when required.7
Malabsorption
For patients with intestinal failure and those undergoing abdominal surgical procedures, malabsorption represents an independent risk factor for weight loss and malnutrition.
Increased losses or altered requirements
In some circumstances, such as enterocutaneous fistulae or burns, patients may have excessive and/or specific nutrient losses; their nutritional requirements are usually very different from normal metabolism.
Energy expenditure
It was thought for many years that increased energy expenditure was predominantly responsible for disease-related malnutrition. There is now clear evidence that in many disease states total energy expenditure is actually less than in normal health. The basal hypermetabolism of disease is offset by a reduction in physical activity, with studies in intensive care patients demonstrating that energy expenditure is usually below 2,000 kcal/day. The exception is patients with major trauma, head injury or burns where energy expenditure may be considerably higher, although only for a short period of time.8,9
Consequences of malnutrition
Malnutrition affects the function and recovery of every organ system.
Muscle function
Weight loss due to depletion of fat and muscle mass, including organ mass, is often the most obvious sign of malnutrition. Muscle function declines before changes in muscle mass occur, suggesting that altered nutrient intake has an important impact independent of the effects on muscle mass. Similarly, improvements in muscle function with nutrition support occur more rapidly than can be accounted for by replacement of muscle mass alone.2,9
Downregulation of energy dependent cellular membrane pumping, or reductive adaptation, is one explanation for these findings. This may occur following only a short period of starvation. If, however, dietary intake is insufficient to meet requirements over a more prolonged period of time the body draws on functional reserves in tissues such as muscle, adipose tissue and bone leading to changes in body composition. With time, there are direct consequences for tissue function, leading to loss of functional capacity and a brittle, but stable, metabolic state. Rapid decompensation occurs with insults such as infection and trauma. Importantly, unbalanced or sudden excessive increases in energy intake also put malnourished patients at risk of decompensation and refeeding syndrome.6
Cardio-respiratory function
Reduction in cardiac muscle mass is recognised in malnourished individuals. The resulting decrease in cardiac output has a corresponding impact on renal function by reducing renal perfusion and glomerular filtration rate. Micronutrient and electrolyte deficiencies (eg thiamine) may also affect cardiac function, particularly during refeeding. Poor diaphragmatic and respiratory muscle function reduces cough pressure and expectoration of secretions, delaying recovery from respiratory tract infections.
Gastrointestinal function
Adequate nutrition is important for preserving GI function: chronic malnutrition results in changes in pancreatic exocrine function, intestinal blood flow, villous architecture and intestinal permeability. The colon loses its ability to reabsorb water and electrolytes, and secretion of ions and fluid occurs in the small and large bowel. This may result in diarrhoea, which is associated with a high mortality rate in severely malnourished patients.
Immunity and wound healing
Immune function is also affected, increasing the risk of infection due to impaired cell-mediated immunity and cytokine, complement and phagocyte function. Delayed wound healing is also well described in malnourished surgical patients.2,9
Psychosocial effects
In addition to these physical consequences, malnutrition also results in psychosocial effects such as apathy, depression, anxiety and self-neglect.
Malnutrition, clinical outcome and the health economy
Clinical outcome
The consequences of malnutrition on physiological function have an important impact on clinical outcome. In the 1930s surgeons observed that patients who were starved or underweight had a higher incidence of postoperative complications and mortality. A large number of studies have subsequently supported this original observation. Malnourished surgical patients have complication and mortality rates three to four times higher than normally nourished patients, with longer hospital admissions, incurring up to 50% greater costs. Similar findings have also been described in medical patients, particularly the elderly.2,10 It is often difficult to separate the deleterious effects of malnutrition from the underlying disease process itself, especially because each can be a cause and/or consequence of the other. However, there is clear evidence that nutrition support significantly improves outcomes in these patients; it is therefore vital that malnutrition is identified through screening.11
The cost
Malnutrition is also a major resource issue for public expenditure. BAPEN has recently calculated that the costs associated with disease-related malnutrition in the UK in 2007 were over £13 billion (greater than that for obesity). This calculation involved the summing of treatment costs for both the underlying disease process and malnutrition. The potential cost savings associated with prevention and treatment of malnutrition are considerable: a saving as small as 1% represents £130 million per year. There is evidence that for specific situations treating malnutrition produces cost savings of 10–20% or more.12
Assessment of nutritional status
Identification of patients at risk of malnutrition at an early stage of hospital admission (or attendance to the outpatient clinic) allows for early intervention with nutritional therapy.
The Malnutrition Universal Screening Tool (MUST)
MUST is a simple, rapid and easy method to screen patients and has been proven to be reliable and valid.11 It aims to identify those at risk by incorporating:
current weight (BMI)
history of recent unintentional weight loss
likelihood of future weight loss.
Figure 1 provides a guide for using MUST. The total MUST score is a better predictor of outcome than scores from the individual components.
Fig 1.
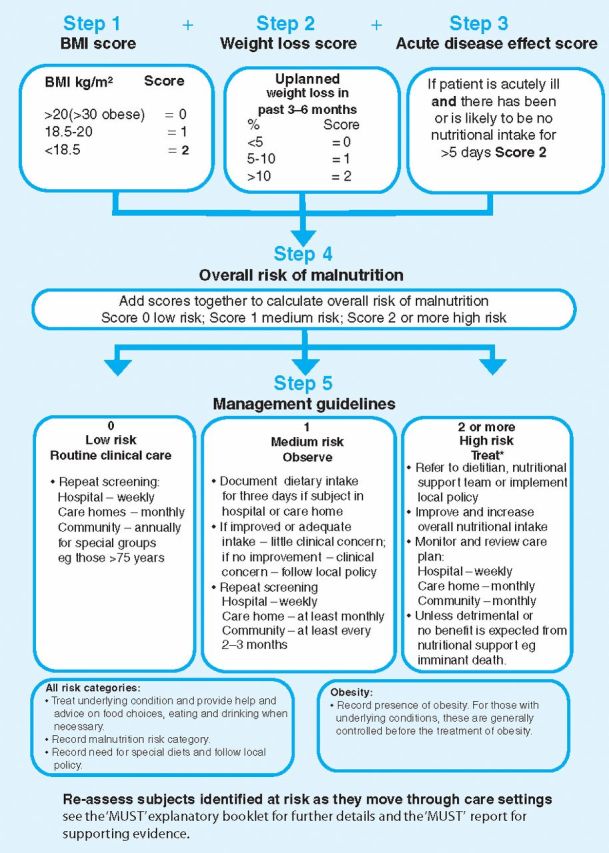
The Malnutrition Universal Screening Tool (MUST) BMI = body mass index. Reproduced with kind pemission of BAPEN.
Screening. The screening process identifies patients who require a more detailed assessment and formulation of an individualised stepwise management plan by a nutrition specialist. In vulnerable patient groups the simple provision of regular meals or food with better nutritional content may be enough to address nutritional risk. Additional measures may include broader menu choices or providing assistance with feeding. Patients in whom these ‘social’ interventions are insufficient to ensure that nutritional requirements are met need the addition of oral nutritional supplements or enteral tube feeding under dietetic supervision. Patients rarely require parenteral nutrition (PN). Need for PN usually occurs in the context of an inaccessible or non-functioning GI tract. Rescreening of inpatients at seven-day intervals throughout a hospital admission alerts clinicians to those who have lost weight and require greater intervention.
Initiatives to improve nutritional care
Several publications 7,13,14 from professional and patient organisations, including the Royal College of Physicians, have highlighted the problems associated with malnutrition. Unfortunately, standards of care in many institutions remain poor. Therefore, a collaboration between the Department of Health and stakeholders with an interest and expertise in nutritional care has published the Nutrition Action Plan which sets out key priorities15 including:
raising awareness
ensuring access to guidance
promoting screening and training
clarifying standards.
The Care Quality Commission has identified nutritional care as one of the core standards which all acute trusts are required to deliver, but not all services are inspected annually and patients continue to die as a consequence of malnutrition. As a result, nutritional care has been included in a new regulatory framework introduced in April 2010 for health and social care services, which will ensure that more attention is focused on nutrition.16 At a local level, all hospitals should have an established multidisciplinary nutrition support team for managing patients with complex nutritional problems. Within each organisation there should also be a nutrition steering committee to develop policies for nutritional care, which should be regularly audited as part of clinical governance frameworks.
Conclusions
Malnutrition, which is often overlooked by clinicians, is common and has wide-ranging effects on physiological function. It is associated with increased rates of morbidity and mortality in hospital patients and significantly increases healthcare costs. Implementation of a simple screening tool identifies patients at risk and allows appropriate treatment to be instituted; this can significantly improve clinical outcomes and reduce healthcare expenditure. Every doctor should recognise that proper nutritional care is fundamental to good clinical practice.14 By addressing deficiencies in education of all healthcare professionals and exerting influence through clinical leadership there can be genuine improvements in nutritional care.
References
- 1.Elia M, editor. Guidelines for detection and management of malnutrition. Malnutrition Advisory Group, Standing Committee of BAPEN. Maidenhead: BAPEN, 2000. [Google Scholar]
- 2.Stratton R, Green CJ, Elia M. Disease-related malnutrition: an evidence-based approach to treatment. Oxon: Cabi Publishing, 2003. [Google Scholar]
- 3.Elia M, Stratton RJ. How much undernutrition is there in hospitals?. Br J Nutr 2000;84:257–9. 10.1017/S0007114500001525 [DOI] [PubMed] [Google Scholar]
- 4.Russell CA, Elia M. Nutrition Screening Survey in the UK in 2008. Redditch, Worcestershire: BAPEN, 2009. [Google Scholar]
- 5.Finch S, Doyle W, Lowe C, et al. National diet and nutrition survey. London: The Stationery Office, 1998. [Google Scholar]
- 6.Jackson AA. Severe malnutrition. In: Warrell DA, Cox TM, Firth JD, Benz EJ, Oxford textbook of medicine 2003. 4th edn vol 1. Oxford: Oxford University Press; 1054–61. 10.1093/med/9780199204854.003.1103 [DOI] [Google Scholar]
- 7.Age Concern Hungry to be heard. The scandal of malnourished older people in hospital. London: Age Concern, 2006. [Google Scholar]
- 8.Elia M. Changing concepts of nutrient requirements in disease: implications for artificial nutrition support. Lancet 1995;345:1279–84. 10.1016/S0140-6736(95)90929-X [DOI] [PubMed] [Google Scholar]
- 9.Green CJ. Existence, causes and consequences of disease-related malnutrition in the hospital and the community, and clinical and financial benefits of nutrition intervention. Clin Nutr 1999;18(Suppl 2):3–28.10459070 [Google Scholar]
- 10.Stratton RJ, King CL, Stroud MA, Jackson AA, Elia M. ‘Malnutrition Universal Screening Tool’ predicts mortality and length of hospital stay in acutely ill elderly. Br J Nutr 2006;95:325–30. [DOI] [PubMed] [Google Scholar]
- 11.Elia M, Russell CA, editors. on behalf of BAPEN and collaborators. The ‘MUST’ Report. Nutritional screening for adults: a multidisciplinary responsibility. Development and use of the ‘Malnutrition Universal Screening Tool’ (MUST) for adults. A report by the Malnutrition Advisory Group of the British Association for Parenteral and Enteral Nutrition, 2003.
- 12.Elia M, Russell CA, editors. Combating malnutrition: Recommendations for action. A report from the Advisory Group on Malnutrition, led by BAPEN. London: BAPEN. 2009. [Google Scholar]
- 13.Leonard-Jones JE, editor. A positive approach to nutrition as treatment. King's Fund Report. London: King's Fund Centre, 1992. [Google Scholar]
- 14.Royal College of Physicians . Nutrition and patients: a doctor's responsibility. Report of a working party of the Royal College of Physicians. London: RCP, 2002. [Google Scholar]
- 15.Department of Health and the Nutrition Summit Stakeholder Group Improving nutritional care: A joint action plan from the Department of Health and Nutrition Summit stakeholder group. London: DH, 2007. [Google Scholar]
- 16.Nutrition Action Plan Delivery Board: end of year progress report. London: DH, 2009. [Google Scholar]


