Abstract
Bile acid malabsorption (BAM) is never life threatening but can cause chronic symptoms. A survey of senior British gastroenterologists was conducted to examine their approach to patients with potential BAM. Of the 706 gastroenterologists contacted, 62% replied. Gastroenterologists see on average 500 new patients in clinic annually; 34% have chronic diarrhoea and 1% are diagnosed with BAM. In those with chronic diarrhoea, 6% of gastroenterologists investigate for BAM first line, while 61% consider the diagnosis only in selected patients or not at all. Sixty-one per cent of patients are diagnosed with type 1 BAM (secondary to terminal ileal disease), 22% have type 2 (idiopathic bile acid malabsorption) and 15% type 3 (unrelated to terminal ileal disease). Only one third of gastroenterologists use a definitive diagnostic test for BAM. BAM (particularly type 2) is under-diagnosed because it is frequently not considered and even when considered, many patients are not subjected to definitive diagnostic testing.
Key Words: bile acid malabsorption, bile salt, binders, chronic diarrhoea, functional diarrhoea, irritable bowel syndrome, SeHCAT, sequestrants
Introduction
Bile acids are synthesised from cholesterol in the liver, stored in the gall bladder and secreted into the bowel where they play a crucial role in aiding the digestion of fats. A highly efficient system ensures that 95% of the daily secreted load of bile acids (15–25 g) are reabsorbed mainly in the terminal ileum and are recycled back to the liver using the so-called enterohepatic circulation. In disease states where absorption is defective or when bile acid production is increased and the absorptive capacity of the small bowel is overwhelmed, increased quantities of bile reach the colon. This triggers fluid and electrolyte secretion into the colon, causing non-specific symptoms which include watery, erratic diarrhoea, with or without foul smelling wind, abdominal pain, recurrent episodes of faecal incontinence, nocturnal defaecation and steatorrhoea. Symptoms can sometimes be very severe and often significantly affect quality of life.1
For 30 years, a series of studies has suggested that bile acid malabsorption (BAM) is frequently not considered as a possible diagnosis. A recent systematic review confirmed that idiopathic BAM is misdiagnosed as diarrhoea predominant irritable bowel syndrome (IBS) in 32% of all sufferers, denying possibly as many as 10 million patients in Europe and North America a correct diagnosis and the possibility of treatment which could cure their symptoms.2 One reason for this is that the gold standard test for BAM, the selenium-75-homocholic acid taurine (SeHCAT) scan, is available only in eight European countries and in Canada. However, the 7-alpha-hydroxy-4-cholestene-3-one blood test is a reasonable alternative and is available worldwide.3,4,5 A possible second reason is that treatment with bile acid sequestrants, the only definitive treatment, is often poorly tolerated, but new therapeutic options are emerging.6,7
To test the possibility that most gastroenterologists are repeatedly missing the opportunity to diagnose BAM, this survey of consultant gastroenterologist members of the British Society of Gastroenterology (BSG) was performed. The aims of this survey were firstly, to determine how often UK gastroenterologists see patients who might potentially have BAM and secondly, to determine their current practice in identifying, investigating and treating the condition.
Methods
A list of consultant gastroenterologists who are current members of the BSG was obtained. Individuals who were clearly identified as hepatologists with no practice in luminal gastroenterology and those who were clearly engaged in research without any clinical practice were excluded. The others were sent by post a short questionnaire and a stamped addressed envelope. A second questionnaire was posted one month later if no reply was received. A third request was emailed to non-responders two weeks later with an invitation to complete the questionnaire online. Data from returned questionnaires were entered into a database. As this was a survey capturing subjective opinions, the quantitative data obtained are presented descriptively.
Results
A total of 706 questionnaires were sent out and 436 were returned (response rate 62%). Gastroenterologists estimated that they see a total of 18,544 new patients (average 42 patients each) in their clinics per month (500 per year). Of these, 6,303 (34%) present with chronic diarrhoea. In 1,379 of these (22%), BAM is considered a possible cause for their symptoms. Collectively, the respondents estimated that they make 184 new diagnoses of BAM per month. This is equivalent to five diagnoses per gastroenterologist per year (1% of new patients).
When asked about their approach towards requesting investigations for BAM in new patients presenting with episodic, chronic diarrhoea, 23 (6%) gastroenterologists said they performed investigations as a first line test, 123 (33%) arranged investigations for BAM if other investigations were normal, 143 (39%) investigated only a selected group of patients and 82 (22%) tested for BAM very rarely or not at all.
Respondents estimated that almost two thirds (61%) of the patients they diagnosed with BAM, had type 1 disease (ie secondary to terminal ileal disease such as Crohn's disease, radiation enteropathy, surgical resection or bypass), while 22% of patients had type 2 BAM (ie idiopathic BAM) and 15% had type 3 (ie unrelated to terminal ileal disease, eg microscopic colitis, following upper gastrointestinal surgery). Two per cent of respondents did not specify what proportion of the patients they diagnosed belonged to each of the three categories of the disease.
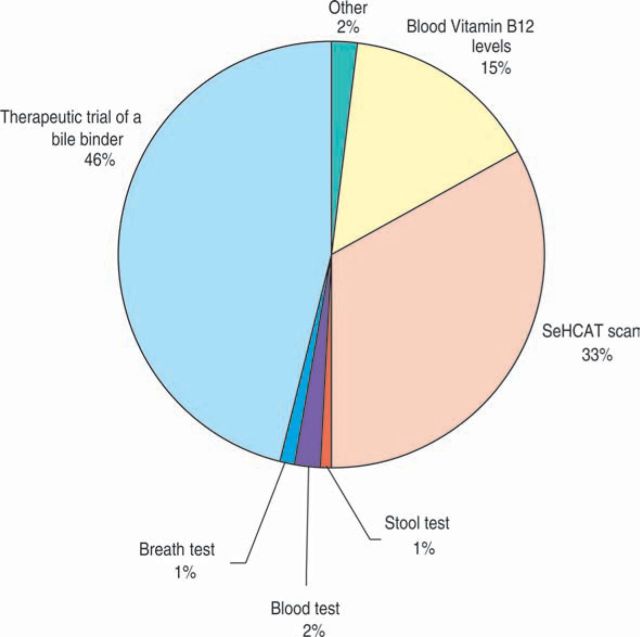
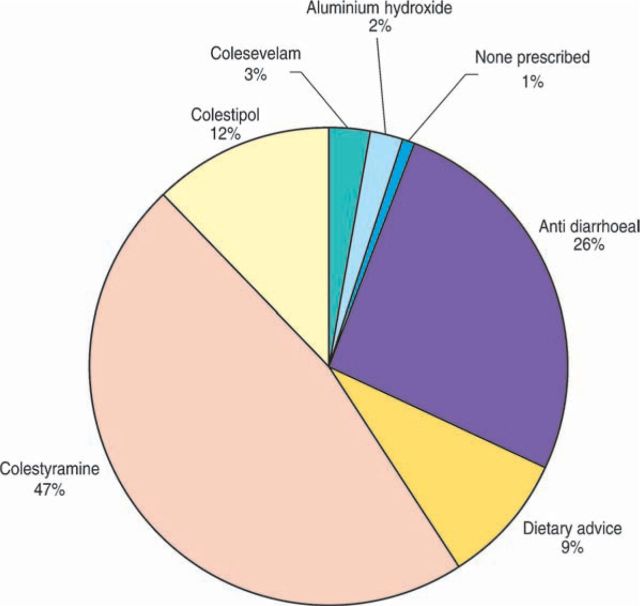
Figure 1 shows the variation in the tests used to confirm a potential diagnosis of BAM. Figure 2 shows the primary treatments prescribed after diagnosis. Some gastroenterologists prescribed more than one primary treatment.
Fig 1.
Test of choice used by each gastroenterologist to diagnose patients with bile acid malabsorption.
Fig 2.
Treatments used for patients diagnosed with bile acid malabsorption.
Conclusion
This survey of senior British gastroenterologists shows that almost one quarter do not consider the diagnosis of BAM and a further third do so rarely. It also shows that idiopathic BAM, in particular, is being significantly under diagnosed.
Consistent data suggest that between 40–60% of all attendees at NHS gastrointestinal outpatient clinics are there to consult about IBS.8 That suggests that between 7,418 and 11,126 patients in this survey consulted because of IBS. One third of all patients with IBS have diarrhoea predominant IBS (ie 2,448–2,708 in this survey) and, as 32% of all patients with diarrhoea predominant IBS type symptoms may in fact have BAM, this means that potentially 783–1,187 patients per month should be diagnosed with idiopathic BAM alone rather than just the 41 patients estimated here (22% of the total of 185 for all causes).
Extrapolating the data obtained from this survey of what gastroenterologists say they do to real life clinical scenarios all around the country has some risks. After all, 38% of gastroenterologists approached did not respond and, in any case, individuals responding to questionnaires may not accurately report what they do in practice while gastroenterologists who are not members of the BSG (a small number) may do something differently. This survey asked individuals to estimate what they do rather than measuring it prospectively. However, these data are completely consistent with take up of the most reliable diagnostic test of BAM, the SeHCAT scan in the UK. The manufacturers confirm that 50% of all requests for SeHCAT scans in the UK come from only 10 hospitals and fewer than 80 of the 250 departments equipped to perform a SeHCAT scan ever do so (M Bewick, GE Healthcare, personal communication). It is also likely that the data gathered here will overestimate rather than underestimate how frequently gastroenterologists look for BAM in their patients. It is safe to conclude that there is a very large gap between the frequency with which gastroenterologists report that they consider the possibility of BAM and the frequency with which they should be considering it as a potential diagnosis.
It is also of note that only one third of respondents used a definitive diagnostic test before reaching a diagnosis and that the majority were content to rely on a therapeutic trial using a bile acid sequestrant. However, these drugs may take 10 days of adequate dosing before achieving a clinically evident response and one in four patients prescribed colestyramine or colestipol are unable to tolerate more than a single dose. Indeed, an early side effect can be worsening diarrhoea or steatorrhoea. These drugs may also have non-specific effects, which lead to an apparent response when BAM is not present. To make a life-changing diagnosis or deny a lifetime of effective treatment on the basis of a potentially flawed therapeutic trial when alternative definitive tests are available may not be the best approach for the patient or the NHS. Even if a condition has no effective treatment, patients deserve a correct diagnosis. However, BAM does often respond dramatically to optimal therapy using diet, anti-diarrhoeals and/or bile acid sequestrants. 1,2,6,7,9 Indeed, if the frequency with which this condition occurs was more widely appreciated, both among primary and secondary care practitioners, it would mean that many patients would not need referral to hospital. Once they reach hospital, almost all of them will be subjected to endoscopic assessment unnecessarily.2 The simplest and cheapest of these (flexible sigmoidoscopy) costs £325 (Department of Health tariff 2009) while a colonoscopy costs over £800. In contrast, a SeHCAT scan for BAM costs £260. If used first line in all patients, it would mean that many endoscopies and outpatient appointments could be avoided.
In summary, more than half of all senior British gastroenterologists do not consider the diagnosis of BAM as frequently as the considerable body of evidence suggests they should and the majority use a flawed diagnostic test to determine whether or not patients should receive long-term therapy.
Funding
An unrestricted educational grant from the Genzyme Corporation (Europe) provided some of the funding for this study. The authors acknowledge NHS funding to the NIHR Biomedical Research Centre. The rest of the funding for this study came from JA's private research funds. No other individuals had any input into the study, its design, what questions were asked or the data received other than the authors.
References
- 1.Bajor A. Bile acid induced diarrhoea: pathophysiological and clinical aspects Gothenburg: University of Gothenburg, 2008 [Google Scholar]
- 2.Wedlake L, A'Hern R, Russell D, et al. Systematic review: the prevalence of idiopathic bile acid malabsorption (I-BAM) as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome (IBS). Aliment Pharmacol Ther 2009;30:707–17 [DOI] [PubMed] [Google Scholar]
- 3.Eusufzai S, Axelson M, Angelin B, Einarsson K. Serum 7alphahydroxy-4-cholesten-3-one concentrations in the evaluation of bile acid malabsorption in patients with diarrhoea: correlation to SeHCAT test. Gut 1993;34:698–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brydon WG, Nyhlin H, Eastwood MA, Merrick MV. Serum 7alphahydroxy-4-cholesten-3-one and selenohomocholytaurine (SeHCAT) whole body retention in the assessment of bile acid induced diarrhoea. Eur J Gastroenterol Hepatol 1996;8:117–23 [DOI] [PubMed] [Google Scholar]
- 5.Sauter GH, Munzing W, Von Ritter C, Paumgartner G. Bile acid malabsorption as a cause of chronic diarrhea. Diagnostic value of 7alphahydroxy-4-cholesten-3-one in serum. Dig Dis Sci 1999;44:14–9 [DOI] [PubMed] [Google Scholar]
- 6.Puleston J, Morgan H, Andreyev HJN. New treatment for bile salt malabsorption. Gut 2005;54:441–2 10.1136/gut.2004.054486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wedlake L, Thomas K, Lalji A, Anagnostopoulos C, Andreyev HJN. Effectiveness and tolerability of colesevelam hydrochloride for bile-acid malabsorption in patients with cancer: a retrospective chart review and patient questionnaire. Clin Ther 2009;31:2549–58 10.1016/j.clinthera.2009.11.027 [DOI] [PubMed] [Google Scholar]
- 8.Jones J, Boorman J, Cann P, et al. British Society of Gastroenterology guidelines for the management of irritable bowel syndrome. Gut 2000;47(Suppl 2ii)1–19 10.1136/gut.47.suppl_2.ii1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wedlake L, Andreyev HJN.Hawkey C, Richter J, Bosch J, Garcia-Tsao G, Chan FKL. Bile acid malabsorption. The textbook of clinical gastroenterology and hepatology 2nd edn Oxford: Wiley-Blackwell, 2010 (in press) [Google Scholar]