Abstract
To comply with the European Working Time Directive (EWTD), from 1 August 2009, junior doctors are required to work no more than 48 hours per week. In accordance with this, East Sussex Hospitals Trust introduced changes to working practice in August 2007. To assess the impact upon patient care and junior doctor welfare a retrospective observational survey comparing data from the year prior to and the year following August 2007 was conducted. No impact on the standard of patient care, as measured by length of stay, death during admission or readmission was found. However, there was a notable increase in episodes of sick leave among junior doctors. Implementation of the EWTD may maintain standards of patient care but may be detrimental to the welfare of doctors in training.
Key Words: European Working Time Directive, junior doctors, patient care, sick leave
Introduction
The European Working Time Directive (EWTD) seeks to promote the welfare of employees by protecting rest periods and by placing a 48-hour limit on the working week.1 Despite a challenge by the UK government, the EWTD was enacted into UK law in 1998 as the Working Time Regulations limiting junior doctors to a 56-hour working week.2 The Department of Health expressed an ‘absolute commitment’ to achieving full compliance with the EWTD by 1 August 2009, with the ‘over-riding objective [of] quality and safety of patient care’, while providing ‘a good work-life balance and training’ for junior doctors.3
The impact on patient care of reducing individual working hours without additional staff is unknown. The introduction of the EWTD may ‘cripple the efficiency of a trust’, since doctors will be required to complete the same volume of work to the same standards but with eight fewer hours per week.4 Alan Robertson, past chair of the British Medical Association's Scottish Junior Doctor Committee, voiced concern over ‘a dramatic reduction in the availability of junior doctors to deliver patient care’.5 The effect of these changes on the welfare of junior doctors has received little attention.
In order to comply with the EWTD, the Department of Medicine at the Conquest Hospital, Hastings (East Sussex) introduced changes in working practice for the August 2007 intake of trainees. As of August 2008, the revised working practices had been in place for a full year. The aim of this study was to investigate the impact of EWTD compliance on patient care and on the welfare of junior doctors
Methods
This was a retrospective observational survey conducted in a single district general hospital. Data were gathered on all nonelective medical admissions during the 12 months preceding the introduction of EWTD-compliant rotas (August 2006–July 2007). For comparison, the same data were also collected for the following 12 months (August 2007–July 2008). To examine the impact on clinical outcomes, length of stay, death during admission, total number of readmissions and episodes of readmission within 30 days were recorded. The results were stratified by age (above and below 75 years) to assess any impact on the care of older patients that might have resulted from the concomitant introduction of ward-based care. To examine the impact on junior doctor welfare, the frequency and duration of their sick leave was examined over the same periods.
The nomenclature of junior doctors changed during the study period. For convenience, the house officer/foundation year 1 grade, senior house officer/foundation year 2/core training grade/general practice vocational training scheme (GPVTS) grade, and specialist registrar/staff grade are referred to as house officer (HO), senior house officer (SHO) and registrar respectively.
Data for medical admissions and readmissions were obtained from the OASIS/PAS Information System (Oasis Medical Solutions, London UK). Patients were included if their date of discharge or death occurred during the study period, and details were recorded on a spreadsheet. Information on sick leave was obtained by hand-searching departmental records. All patient and personal data were anonymised prior to analysis. Data are presented as means and standard deviations for continuous variables and as medians and ranges (length of stay, and episodes and duration of sick leave). Where data were normally distributed, unpaired Student's t test was used to compare values before and after the EWTD implementation. Where data were not normally distributed this comparison was achieved with a non-parametric equivalent (Mann-Whitney U test). Categorical data were compared using a chi square test. All statistical analysis was carried out using SPSS 16.0 (SPSS Inc, Chicago, USA).
Results
In-hospital mortality and length of stay
Prior to the implementation of EWTD-compliant rotas (year to August 2007) there were 8,457 non-elective medical admissions (Table 1). The average age of these patients was 70.2?18.2 years, with similar numbers of males and females. In total, 812 (9.6%) patients died while in hospital. The median length of stay was six days, range 1–305 days. Of the sample, 4,152 patients were aged 75 years or less. Their in-hospital mortality and median length of stay were 4.3% and four days, range 1–305 days, respectively. In contrast, the 4,520 patients aged ≤ slant 75 years experienced an in-hospital mortality of 14.7% and a median length of stay of 8 days, range 1–173 days.
Table 1.
Admissions for the periods before (August 2006–July 2007) and after (August 2007–July 2008) the implementation of the European Working Time Directive (EWTD)-compliant rotas. Figures are numbers and percentages, or median values (with range).
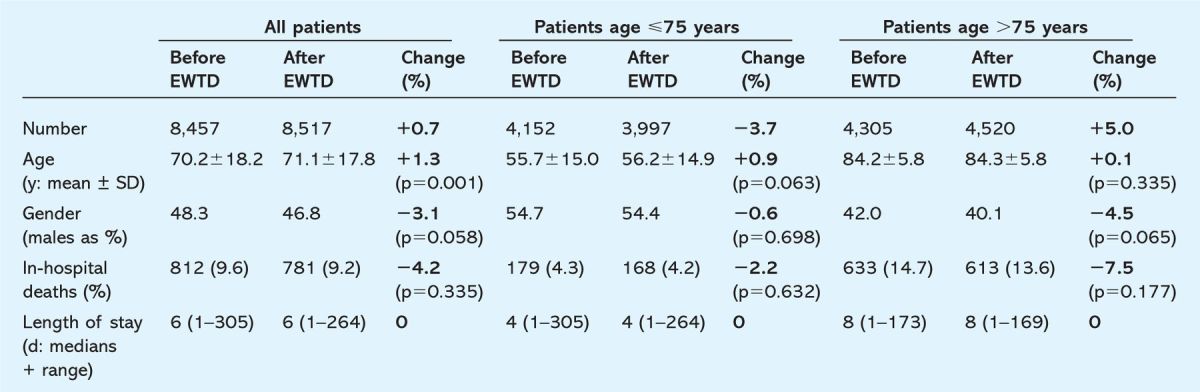
Following the implementation of EWTD-compliant rotas (year to August 2008) there were 8,517 non-elective medical admissions, an increase of 60 (0.7%) over the preceding year. The average age of these patients, increased by 0.9 to 71.1± 17.8 years (p = 0.001). The proportion of male admissions fell by 3.1% (p = 0.058). In-hospital mortality decreased from 9.6% to 9.1% (p = 0.335), the median length of stay remained unchanged. The number of patients aged ≤ slant 75 years fell by 155 to 3,997 while the number of patients older than 75 years increased by 215 to 4,520. In-hospital mortality declined to 4.2% and 13.6% for patients ≤ slant 75 years and > 75 years of age (p = 0.632 and p = 0.177 respectively). The median length of stay was unchanged for both groups.
Readmissions
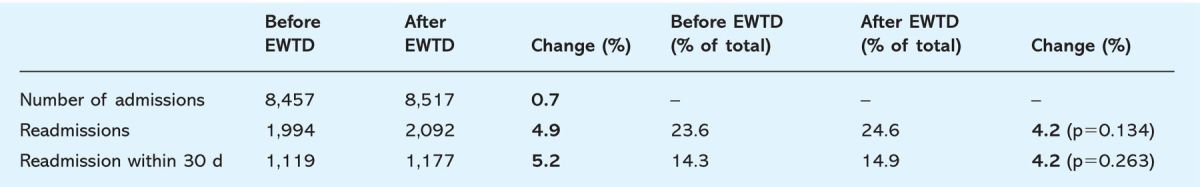
Prior to the implementation of EWTD-compliant rotas (year to August 2007) the 8,457 admissions comprised 6,463 single admissions and 1,994 readmissions. Thus readmissions represented 23.6% of all patients admitted during the year. Of these, 55% were > 75 years of age. In total, 1,119 (56%) readmissions occurred within 30 days of discharge.
Following the implementation of EWTD-compliant rotas (year to August 2008) the 8,517 admissions comprised 6,425 single admissions and 2,092 readmissions. Thus readmissions represented 24.6% of all patients admitted during the year – an increase of 4% (p?0.134) over the preceding year. The proportion of patients readmitted who were ?75 years of age and the proportion of readmissions occurring within 30 days were unchanged (p = 0.263) (Table 2).
Table 2.
Readmissions for the periods before (August 2006–July 2007) and after (August 2007–July 2008) the implementation of the European Working Time Directive (EWTD)-compliant rotas. Figures are numbers and percentages.
Junior doctor sick leave
In the year prior to the implementation of EWTD-compliant rotas, of the 58 trainee medical doctors (22 HO, 23 SHO and 13 registrars) 22 took 31 episodes of sick leave totalling 179 days.
The median number of episodes taken per trainee was 0, range 0–3. The median duration of leave was 0 days, range 0–72 days (Table 3).
Table 3.
Sick leave taken by junior doctors for the periods before (August 2006–July 2007) and after (August 2007–July 2008) the implementation of the European Working Time Directive (EWTD)-compliant rotas. Figures are numbers and median values (with range). ∗Proportionate change cannot be calculated.
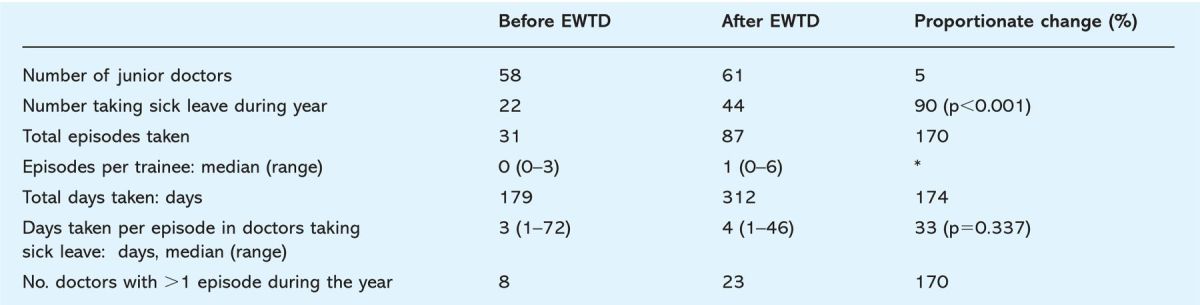
Following the implementation of EWTD-compliant rotas, 44 (72%) of the 61 trainee medical doctors (24 HO, 26 SHO and 11 registrars) took 87 episodes of sick leave totalling 312 days. The median number of episodes taken per trainee was 1, range 0–6.
Taking into account the increase in trainee numbers, the proportion of junior doctors taking sick leave increased by 90% (p?0.001), and the total episodes taken by 170% in the year following the implementation of EWTD-compliant rotas. Whereas eight trainees (14%) took more than one episode of leave between 2006 and 2007, 23 (38%) did so the following year. In those doctors taking sick leave, the number of days taken per episode rose slightly from three days, range 1–72 days, to four days, range 1–46 days (p?0.337).
Discussion
With 58 full-time junior medical doctors at the hospital between 2006 and 2007, the rotas necessary to comply with the introduction of EWTD resulted in a loss of at least 348 working hours each week, the equivalent of seven whole-time posts. Night shifts were reduced from a seven-day block, which may reduce performance, to periods of three and four nights on-call.6
Patient care (as measured by in-hospital mortality and length of stay) was not affected by these changes to working practice. The percentage of inpatients who died in hospital fell slightly but their median length of stay was unchanged. There was a small rise in readmissions.
During the study period, episodes of sick leave among junior doctors more than doubled with just over 1 in 3 taking leave in the year to August 2007 and nearly 3 in 4 the following year. The number of days taken and the number of repeated episodes of leave increased.
Reliable comparative adjusted data for admissions and length of stay for non-elective medical admissions could not be found. Fifty per cent of patients in the current study were over 75 years of age, which compares with a value of approximately 25% given in the Hospital Episode Statistics (HES) for 2006–7.7 The hospital standardised mortality ratio (2002–5) for the two local primary care trusts was 90.9 and 98.0 suggesting that the observed in-hospital mortality is unexceptional.8 Local length of stay is higher than for national comparator sites but equivalent to those areas with similarly elderly populations.9
To facilitate an even distribution of junior doctor workload, inpatient care was also partially reorganised, from an age-related (cut-off 75 year) to a ward-based system. This had no apparent effect on patient outcome.
Readmissions comprised nearly one quarter of all admissions. Although seemingly high, reported rates in other adult populations vary from 5% to 29%.10 The NHS Information Centre reported a 22% increase in readmissions within 28 days (in patients aged 16–75 years in all specialties) to 8.6 per 100 discharges, from 1998 to 2006. For patients over the age of 75 there was a 31% increase in readmissions to 13.6 per 100 discharges over the same period, a rate similar to our findings.11
Longer working hours and extended work shifts are reported to adversely influence junior doctor performance with shorter hours associated with less serious medical errors.12–14 However, the authors are not aware of any literature on the relationship between working practice and sickness in medical trainees. In factory employees, the number of sick days during the preceding six months was related to psychosomatic wellbeing, while a review of sickness in non-medical literature identified several recurrent factors.15 These included repeated absences, poor working conditions, lack of group cohesiveness, organisational behaviour and job satisfaction, use of abilities and responsibility and ‘marketplace conditions’.16
Most, if not all, of these factors may apply to medical trainees. Changes to both the organisation of care and medical training have recently occurred. In addition to the increasing emphasis on reduced length of stay on medical wards, the system of application for training has been restructured and trainee hours reduced. Both shift work and reduced working hours may contribute to a loss of the ‘group cohesiveness’ provided by the traditional medical team. These factors may exert a cumulative effect although only a tightening of the existing shift rotas, and a rearrangement of ward working specifically separate the years studied. The rotas necessary to comply with the directive reduced the numbers of doctors available on the wards at any one time, thus rising sickness levels have a proportionately greater effect on working hours lost. This is compounded by difficulties in arranging locum cover and the shortfall in trainee recruitment that has occurred in some areas.
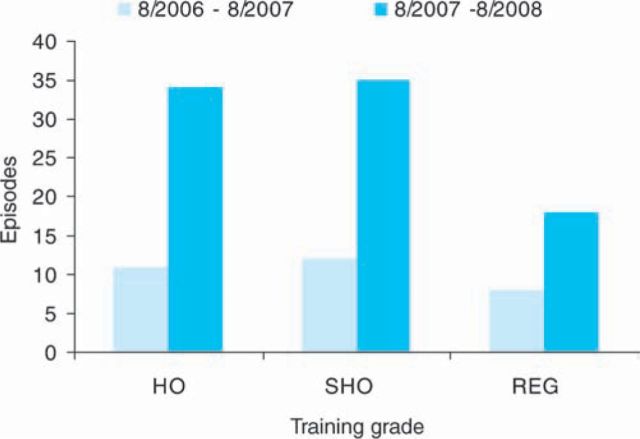
Sick leave was chosen as a measure of junior doctor welfare due to a comprehensive internal system of paper records of self-and externally certified sick leave. Although sick leave may be a weak index of trainee welfare, a more robust indicator is lacking. The pattern of leave appeared not to change, insofar as the number of days taken per episode was relatively constant, suggesting that alterations to working practice affected frequency as opposed to type of absence. While it might be expected that the burden of the reduction in hours might fall upon new trainees, the increase in sick leave was seen across all grades (Fig 1). This would also suggest a generic effect and response; not only does the loss of hours impact upon all trainees, but the response to this demand was not driven by a differing work ethic between new and more experienced trainees. It might also suggest that more senior trainees may be taking on roles previously performed by more junior grades. Finally it is salutary to note that in the space of one calendar year the average age of patients rose significantly, with an increasing number of female admissions. There are considerable implications for healthcare planning if such trends are sustained.
Fig 1.
The total number of episodes of sick leave taken, by grade, for the period August 2006–July 2007 and August 2007–July 2008. HO ? house officer; REG ? registrar; SHO ? senior house officer.
There are several limitations to this study. All patient data were extracted from the patient information system and are thus subject to the constraints of the reliability of that system. Assuming no systematic error in the local information system, the large numbers contained should, however, serve to minimise any errors in patient data. The study is a retrospective observational analysis and reflects the impact of working patterns implemented at a single site and may not be representative of other areas. Prospective data from several sites would be required to confirm the findings presented here. Data on sick leave were collected from paper forms submitted by the trainee. Underreporting is possible but unlikely to be significant since rigorous efforts were made to ensure adequate levels. Changes to the recruitment, training and working practices of junior doctors may have confounded the findings.
Conclusion
While not associated with any major effect on patient care, the changes in working practice necessary to comply with the EWTD were associated with, and may have contributed to, a detrimental effect on the welfare of doctors in training. The directive may have failed in its primary purpose: that of promoting the welfare of employees.
References
- 1.Council Directive 93/104/EC Official J. Euro Community 1993;L307:18–24 [Google Scholar]
- 2.Judgement of 12 November 1996: Case C-84/94 UK ν Council of the EU European Court Reports 1996;1–5755 [Google Scholar]
- 3.Department of Health The European Working Time Directive for trainee doctors – implementation update London: DH, 2009;www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_093939 [Google Scholar]
- 4.Pounder R, et al. Junior doctor' working hours: ‘can 56 go into 48?’. Clin Med 2008;8:126–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Warns B, editor. European Working Time Directive – time is running out. Medical News Today. Scotland: MA; www.medicalnewstoday.com/articles/131223.php. [Google Scholar]
- 6.Murray A, Pounder R, Mather H, Black C, et al. Junior doctors' shifts and sleep deprivation. BMJ 2005;330:1404. 10.1136/bmj.330.7505.1404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hospital Episode Statistics. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=193.
- 8. www.society.guardian.co.uk/guides/drfoster/quality/0,1502738,00.html?chosen=Bexhill%2520and%2520Rother&start=20&index=2&alpha=0.
- 9.Internal Consultancy Report into Trust Activity.
- 10.Hasan M, et al. Readmission of patients to hospital: still is ill defined and poorly understood. Int J Qual Health Care 2001;13:177–9 10.1093/intqhc/13.3.177 [DOI] [PubMed] [Google Scholar]
- 11.Fears over hospital readmissions. BBC News, http://news.bbc.co.uk/1/hi/health/6723767.stm.
- 12.Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med 2004;351:1829–37 [DOI] [PubMed] [Google Scholar]
- 13.Barger LK, Cade BE, Ayas N, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med 2005;352:125–34 [DOI] [PubMed] [Google Scholar]
- 14.Landrigan CP, Rothschild JM, Cronin JW, et al. Effect of reducing interns' work hours on serious medical errors among interns in intensive care units. N Engl J Med 2004;351:1838–48 [DOI] [PubMed] [Google Scholar]
- 15.Schmitt M, Dörfel M, et al. Procedural injustice at work, justice sensitivity, job satisfaction and psychosomatic well-being. Eur J Social Psychol 2002;29:443–53 10.1002/(SICI)1099-0992(199906)29:4 [DOI] [Google Scholar]
- 16.Luz J, Green MS, et al. Sickness absenteeism from work – a critical review of the literature. Public Health Rev 1997;25:89–122 [PubMed] [Google Scholar]