Introduction
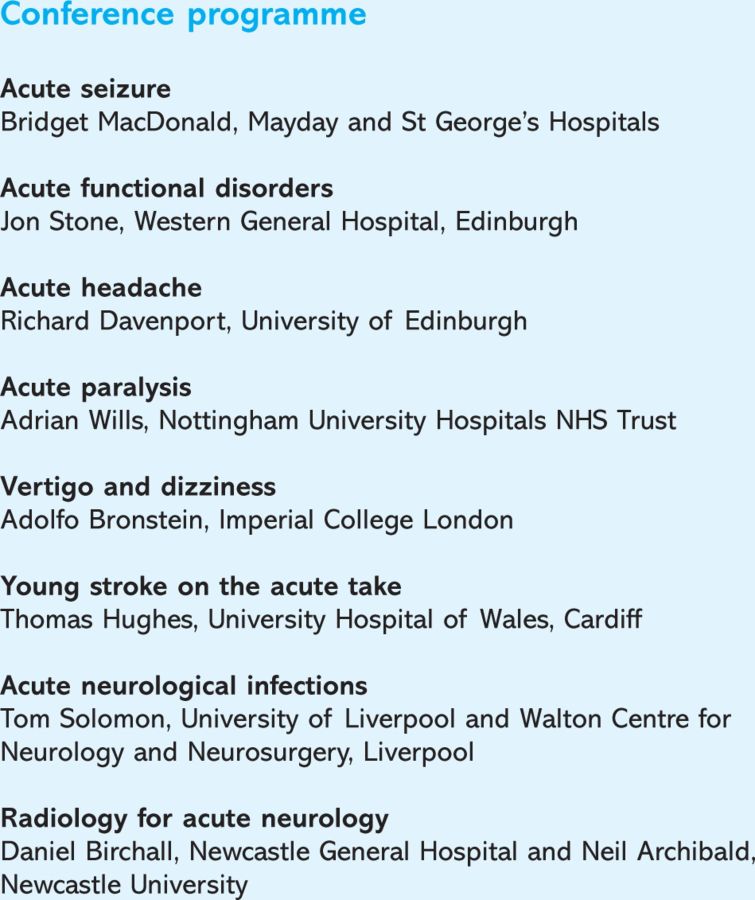
Approximately 20% of acute medical admissions have a significant neurological problem.1 One aim of the Association of British Neurologists (ABN) is that all these patients should be seen by a neurologist within 24 hours. This would require an increase in the number of dedicated neurology beds to 15 per 100,000 as well as an increase in the number of consultant sessions to cover these.2 It is hoped that the number of available neurologists in all hospitals to see patients acutely will be increased but in the meantime much neurology is managed by general physicians. The aim of this conference was to equip those dealing with these patients with the necessary information to do so with more confidence.
Fits, faints and dizzy dos
Making the diagnosis of seizure is not always straight forward and the most important investigation in these patients is always an electrocardiogram (ECG). Once confident that the patient has had a seizure, the decision becomes whether to treat and with what. Imaging is essential if the onset is focal which can be assumed in anyone over 25. Treating first seizures is not always necessary but may be important to the patient who is keen to avoid a further fit at all costs. In primary generalised epilepsy the most effective treatment is usually sodium valproate. In the case of focal onset or partial epilepsy evidence suggests lamotrigine as first line treatment with carbamazepine in close second.3 Young adults with a history of myoclonic jerks or photosensitivity require an electroencephalogram (EEG), as drugs such as carbamazepine and phenytoin can exacerbate the jerks of idiopathic generalised epilepsy.
‘There can be few physicians so dedicated to their art that they do not experience a slight decline in spirits on learning that their patient's complaint is that of giddiness’.4 Adolfo Bronstein is such a physician and he lightened the rest of our spirits too with regard to the dizzy patient. The most useful test when presented with a single episode of vertigo is the head impulse test. Ask the patient to maintain visual fixation on your nose. Turn the patients head very quickly to one side and back again. The movement need not be a large one. Repeat to either side. If the patient is able to maintain fixation then the test is intact. If the patient is unable to maintain fixation and there is a catch-up saccade then this implies an abnormal test. In practice, if this test is abnormal then it will save unnecessary magnetic resonance imaging (MRI) as the diagnosis is acute vestibular neuritis. A brain scan is only required in acute vertigo in the following situations: intact head impulse test, new onset headache, any central symptoms or signs of acute deafness.
To lumbar puncture or not to lumbar puncture?
As junior doctors' hours are cut so is their opportunity to gain experience in practical procedures. Not all medical trainees will rotate through neurology and so their experience in lumbar punctures (LPs) will come from general medicine. As Richard Davenport stated, history always comes first but if a physician has established that a patient's headache was truly of sudden onset then a computed tomography (CT) scan and, if that's negative, an LP is mandatory to exclude subarachnoid haemorrhage (SAH). There is no clinical scoring system to avoid this. Ten to 25% of patients with sudden onset headache will have SAH and 10% of SAHs present with headache alone. When doing the LP it is vital to check the opening pressure. A high opening pressure may suggest an alternative cause of acute headache, such as cerebral venous sinus thrombosis which needs to be investigated with MR or CT venogram.
The other main indication for LP in a general medical setting is in the context of infection. The clear message from Tom Solomon is that unless there are contraindications then perform an LP. There is still a lot of confusion about their safety. Raised intracranial pressure occurs in acute bacterial meningitis but it is not the raised pressure itself that makes an LP dangerous but rather a shift between compartments. There are certain clinical signs that suggest a contraindication to LP before CT which include: focal neurological signs, papilloedema and seizures. Too many patients with acute bacterial meningitis are having unnecessary CT scans causing a delay in LP. When an LP is performed ensure that the cerebral spinal fluid and serum are sent for glucose testing. Ensure that when the LP has been done that results are chased, recorded and acted upon.
Paralysis and thrombolysis
Thrombolysis for stroke has the potential to change neurology into a very acute specialty. There is a premium on giving the treatment quickly meaning that assessments and decisions have to be made rapidly. This is often tricky early in stroke when the scan may be normal and the signs still evolving. The involvement of a neurologist may be useful when it is important that stroke mimics are recognised early. Thomas Hughes would argue that the term stroke is unhelpful in itself as it lumps a group of potentially very different patients into one and puts them in a common treatment pathway. Indeed how often is a patient with any vague hint of a neurological disorder labelled as ‘?stroke’ on the post-take ward round? Understanding neuroanantomy is key to understanding each patient's individual story and enables a general physician to localise lesions in the nervous system.
Some patients who present with paralysis may have a functional disorder. The key is to think of functional disorders as a positive diagnosis, not just because the scan is normal or the patient ‘weird’. There will be clues in the history and examination as in pneumonia or angina. In the patient with paralysis, clues in the history that point towards a functional aetiology include: multiple previous episodes with complete recovery, multiple other symptoms, panic attack or physical injury followed by ‘stroke’, onset during examination, or dense arm and leg weakness with no eye or head deviation. Hoover's sign is a useful tool in diagnosis and can also be used as a way of explaining to the patient that their muscle and nerve ‘hardware’ is working but that the problem is with the ‘software’. In this test the patient's ability to extend a previously weak hip against resistance, when asked to flex the opposite hip against resistance, is demonstrated. Jon Stone would advocate an honest approach to the functional patient. Try separating the ‘why’ from the ‘how’, call it functional and try analogies such as ‘hardware’ and ‘software’. The advantage of this approach is that the patient can then be given information leaflets and access to other sources (eg www.neurosymptoms.org).
In patients with neuromuscular paralysis, either acute or chronic, the main cause of mortality and morbidity is ventilatory failure. Attention to respiratory function and the patient's ability to protect their airway is paramount. Tests often lag behind the clinical picture and early intensive care involvement is often necessary. In evaluating the patient with acute weakness and respiratory distress check use of accessory muscles and paradoxical breathing, vital capacity erect and supine and arterial blood gas but beware that deterioration on these is often late. Chronic conditions such as muscular dystrophy and motor neurone disease can present acutely, either because the condition itself has not been diagnosed or the ventilatory failure has gone unrecognised or ignored. It is preferable to discuss potential options such as non-invasive ventilation and antibiotics when the patient has time to weigh up the pros and cons of such treatments. Beware the asymptomatic patient. Investigations which help alert to those patients who may need support include oxygen saturations, vital capacity, and SNIP (sniff nasal pressure). In both acute and chronic situations any bulbar involvement will also make the patient more vulnerable.
It's all in the scan
A pragmatic session on radiology reminded the audience that scanning patients with acute neurology is about getting the necessary information to inform and guide best management. CT scanning is fast, accessible and well-tolerated. Contrast enhances the utility of CT scans immensely and should always be considered when there is a possibility of a structural lesion. CT also performs well in the posterior fossa. MRI detects more subtle lesions but it is the rapid hydrocephalus that can occur in obstruction of the fourth ventricle that can be fatal, and where CT can be life saving. A pre-test probability of how likely the chances are that the scan will be normal or abnormal is important. In a patient with focal onset seizures, for example, the chance of a focal structural lesion is high and the physician should not be satisfied with a normal CT scan – even with contrast. In some situations it is always best to phone a colleague. For example, telling the difference between infection and tumour even on MRI is difficult and highlights the danger of interpreting scans without taking into account the clinical picture and other test results.
Conclusion
As a neurology registrar the one-day conference brought together a lot of issues which are encountered on a daily basis. It is hoped that the outcome of the conference will not be to reduce the number of on-call referrals that I receive, but rather that it will help general physicians who do not have easy access to a neurologist to investigate and treat these patients, while waiting for more to appear on the shop floor soon.
References
- 1.Association of British Neurologists UK neurology: the next ten years – putting the patient first London: ABN, 2003 [Google Scholar]
- 2.Carroll C, Zajicek J. Provision of 24 hour acute neurology care by neurologists: manpower requirements in the UK. J Neurol Neurosurg Psychiatry 2004;75:406–9 10.1136/jnnp.2003.018010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marson AG, Al-Kharusi AM, Alwaidh M, et al. The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomised controlled trial. Lancet 2007;369:1000–15 10.1016/S0140-6736(07)60460-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthews WB. Practical neurology Oxford: Blackwell, 1963 10.1016/0960-8966(91)90112-6 [DOI] [Google Scholar]