Abstract
Renal specialty medical training in the UK was reformed in August 2007, with an emphasis placed on competency-based training and the publication of a new curriculum and assessment blueprint. This model of training places additional time demands on both trainees and trainers, with implications for job planning and service delivery. We evaluated the resource requirements and impact on service delivery of implementing a high-quality training programme in renal medicine. Each trainee maintained a portfolio containing details of workplace-based assessments. The change in educational environment led to improved trainee satisfaction. The mean total consultant time involved in implementing the training programme was 0.7 programmed activities (PAs) per trainee per week in the first year, which decreased to 0.5 PAs per trainee per week in the second year. This pilot study indicates that it is possible to integrate successful and high-quality specialty training in a busy clinical environment. The model outlined could form a template for postgraduate specialist training delivery in a variety of medical specialties.
Key Words: JEST, medical education, PHEEM, specialty training, workplace-based assessments
Introduction
Historically, postgraduate medical education in the UK relied exclusively on experiential training acquired in the workplace over a fixed period of time. As this educational model was increasingly difficult to justify, specialty medical training in the UK was radically reformed in August 2007. This represented a definitive move away from the traditional one-off assessment towards continuous and structured assessment of a doctor's long-term performance. The new training model is competency based and comprehensively assessed both in the workplace and by specialty examinations. Each specialty developed a detailed curriculum associated with an assessment blueprint and appropriate workplace-based assessment tools.1 The shift towards a competency-based approach specifies what is taught and, importantly, what is assessed. This model of training places additional time demands on both trainees and their educational supervisors, with unknown implications for job planning and service delivery.
The other major influence on training junior doctors has been the enforcement of the European Working Time Directive (EWTD).2 This limits the average working week to 48 hours, which has necessitatWWed a move to shift-based working patterns and potentially reduced training opportunities.
The renal specialty registrar training programme at University Hospital Birmingham Foundation Trust (UHBFT) was started in October 2008 as a direct response to the new curriculum. The objective was to develop a training and assessment structure in a very busy unit with substantial service commitment. This pilot project aimed to evaluate the resource requirements and impact on service delivery of implementing and maintaining a high-quality specialty training programme in renal medicine.
The regional unit at UHBFT is the largest provider of end-stage renal care in the West Midlands and offers comprehensive nephrology, dialysis and transplantation services. The unit provides dialysis services to 1,000 patients, provides 24,000 outpatient appointments and performs about 150 renal transplantations annually. In addition to elective work, around 500 emergency admissions due to acute kidney injury are managed each year. In parallel with the clinical service runs a very active research programme involving both clinical and laboratory research. The unit has always had experienced clinicians and enthusiastic teachers who have shaped the careers of many trainees. Before the education training pilot, trainees learnt ‘on the job’ by actively participating in clinical practice in the wards and outpatient department. Senior clinicians acted as role models for the trainees' professional thinking and attitude. Nevertheless, this form of experiential learning was disorganised and dependent on the trainee's motivation. A structure to ensure curriculum coverage was lacking and the learning objectives and expectations were ill defined. It became evident that traditional practices for delivering training had become incompatible with the organisation of a modern clinical service and the requirements of the new renal curriculum. Feedback from both trainees and trainers suggested that training and service delivery were regarded as producing conflicting demands for both parties rather than integrating into the work environment.
The process of reform
A pilot project was started in September 2008 for a period of 12 months. The UHBFT provided funding equivalent to eight consultant programmed activities (PAs) for this pilot, which was used to fund the appointment of a consultant whose duties included planning and managing the programme (the programme manager), as well as backfilling other consultants' commitments when they were engaged in training. The training programme was overseen by a committee comprising educational supervisors and a trainee representative, who met at regular intervals. This programme was limited to trainees within the organisation and was separate from deanery-delivered ‘renal training days’.
The programme manager's role was crucial in organising and facilitating the training programme. The programme consisted of scheduled workplace-based assessments (WPBAs) with designated trainers, supervised ‘training clinics’, scheduled supervised training in procedures, lunchtime teaching and trainee-delivered activities such as journal clubs. The role of the programme manager was to organise lunchtime teaching, draw up monthly rotas for case-based discussions, arrange for training clinics (described below) based on clinic schedule, develop weekly rotas for specialty training (with minimal disruption to service provision) and email these to trainees, and provide reminders and reinforcement to trainees and trainers. The programme manager also maintained an overview of the WPBAs carried out in the department, which ensured that the trainees had broad exposure to various aspects of renal medicine.
Programme content
Formal teaching sessions
A syllabus for formal teaching sessions mapped to the new curriculum was developed and the trainers were invited to provide formal teaching sessions. One hour-long lunchtime session was provided per week.
Case-based discussions (CbD)
Each trainee was required to complete at least two CbDs every month with a nominated educational supervisor. The exact timing and content of these were left to the trainee and designated supervisor.
Mini-clinical examination exercise (CEX)
Although our initial plan was to perform the mini-CEX assessment on the ward, it was difficult to do so because of pressing service commitments. We developed a model of training clinics conducted at regular intervals within the normal outpatient settings, in which a trainer sat with a trainee and carried out assessments such as the mini-CEX and CbD. Generally, the trainee and trainer are supernumerary (but may see 4–6 patients) and the programme manager had a flexible job plan to backfill the clinics that arose due to training commitments.
Acute care assessment tool (ACAT)
The ACAT was used opportunistically to assess the trainees' clinical and organisational skills during the acute take.
Procedural training
Structured procedural training was timetabled for the trainees and their competencies (directly observed procedural skills (DOPS)) were assessed regularly.
Trainee-delivered teaching
Trainees were expected to manage and deliver teaching for non-specialty grades, including journal clubs, which were timetabled.
Methods
Using Microsoft Outlook's calendar, data regarding consultant time, WPBAs undertaken and competency progression were collected prospectively. In order to implement the training model successfully, significant changes were made to the working practices of both trainees and educational supervisors. Trainees were allocated a consultant educational supervisor to ensure delivery of training and assessment in the clinical environment. The educational supervisors were involved in drawing up a personal development plan tailored to the individual trainee's needs. They reviewed the trainee's WPBAs and provided feedback on performance and career advice.
Evaluation of the education pilot
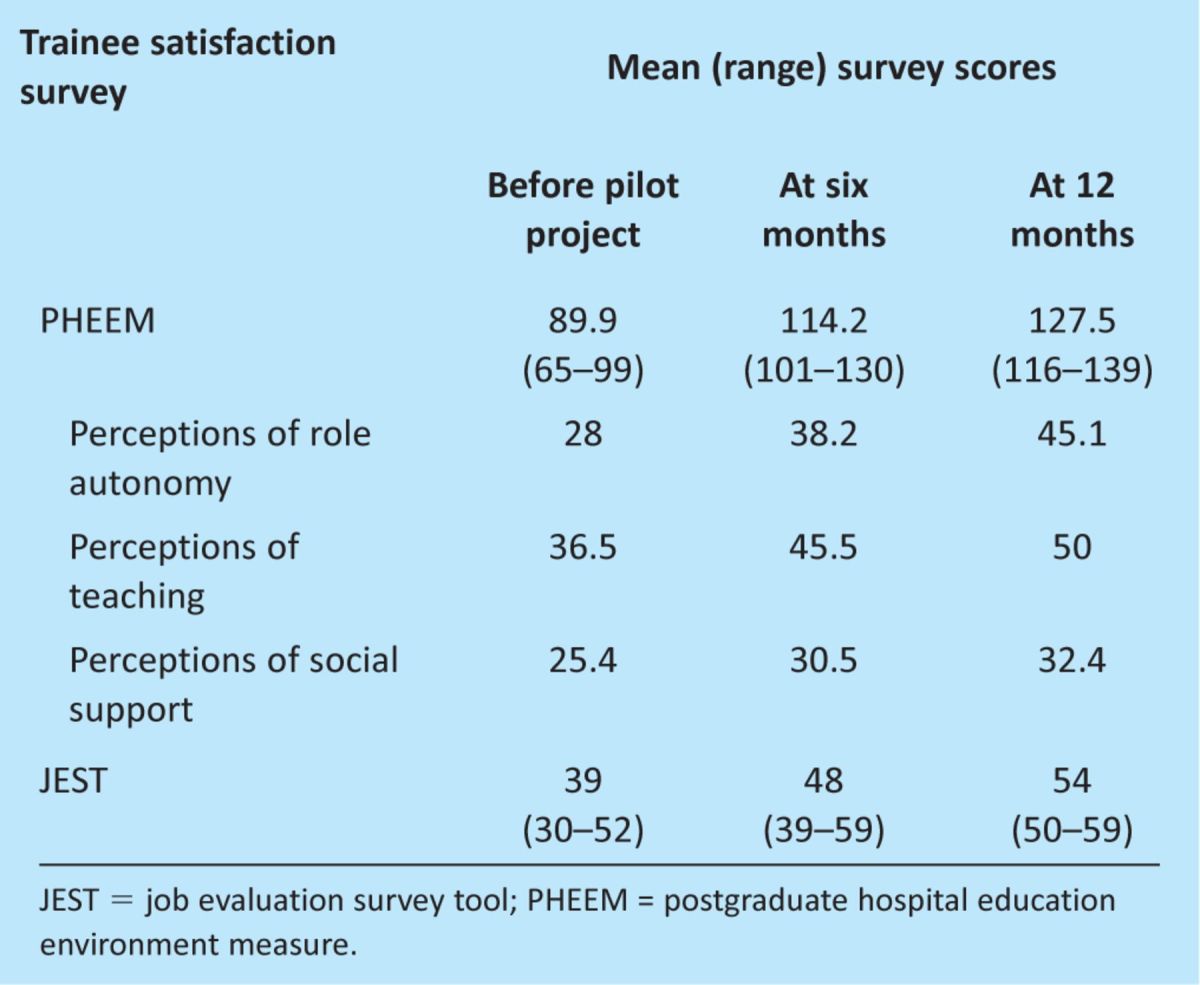
Trainees' expectations and satisfaction were evaluated using validated questionnaires (postgraduate hospital education environment measure (PHEEM)3 and job evaluation survey tool (JEST)4) administered before and at the end of the pilot study. We used the PHEEM questionnaire to measure the quality of educational environment before and after the change in the education programme. The PHEEM is a 40-item inventory, with each item scored on a scale of 0–4 under the subscales of perceptions of role autonomy, perceptions of teaching and perceptions of social support. The JEST was developed by the NHS West Midlands Workforce Deanery and focuses on 15 requirements mapped to the Postgraduate Medical Education Training Board (PMETB) generic standards for training.
Results
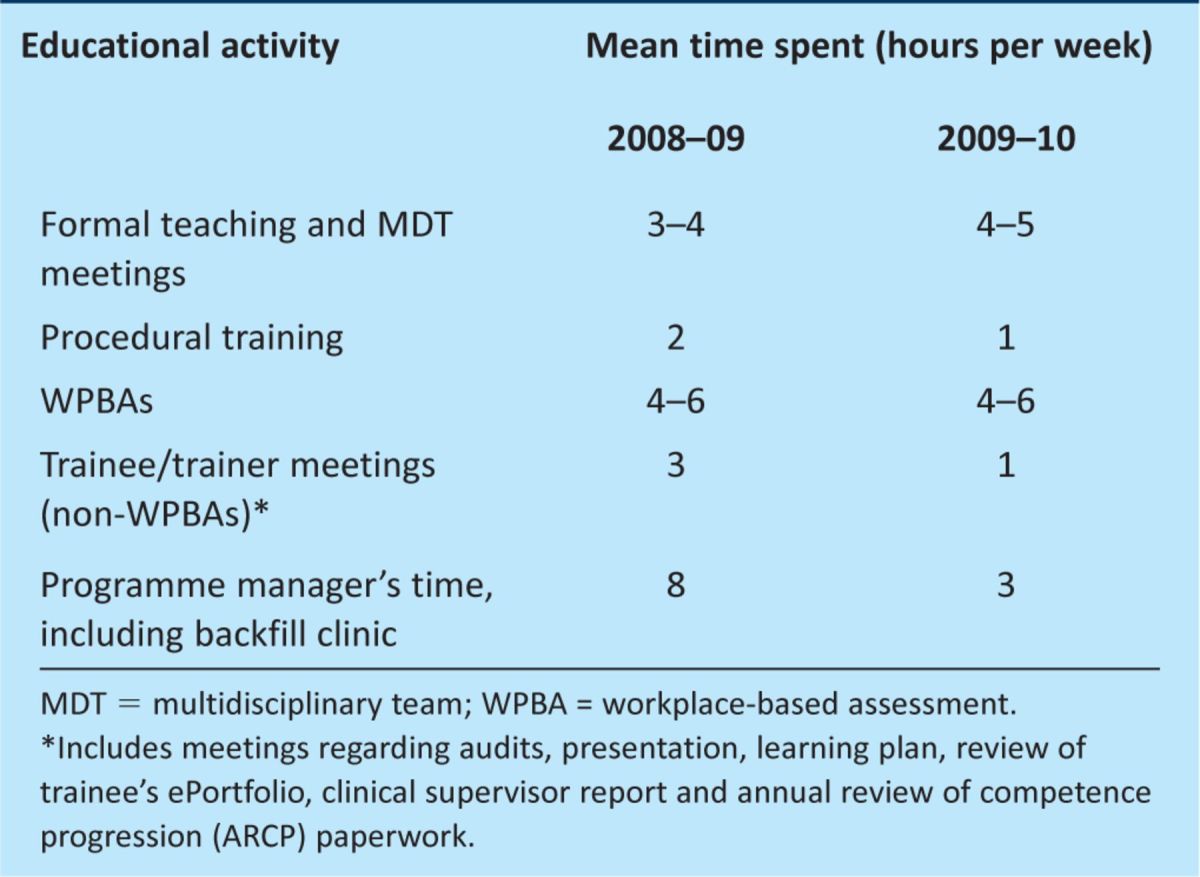
The mean total consultant time involved in setting up the training programme and in direct training activities was 5.7 PAs per week, which was equivalent to 0.7 PAs per trainee per week in the first year. Since the initial set up, the mean consultant time decreased to 3.5 PAs in the second year (0.5 per trainee per week) (Table 1). This translates to four hours of formal teaching and at least one hour of one-to-one training with a clinical supervisor for every registrar on a weekly basis. This reduction in consultant time can be attributed to better streamlining of the training process. In the first year, every aspect of the training programme was micromanaged by the programme manager. In the second year, an appreciable change in culture enabled trainees to contribute and manage some aspects of their training programme. During the initial stages of the pilot study, much of the programme manager's time was used to set up the teaching modules and the databases used to record activities and communicate the changes. Once the training programme was established, it was less time consuming to run it on a day-to-day basis.
Table 1.
Consultant time spent in training.
The change in the educational environment had a positive effect on trainee satisfaction, as suggested by the validated scores. The mean PHEEM scores prior to starting, at six months and at 12 months were 89 (range 65–99), 114 (101–130) and 126 (116–139), respectively. The mean JEST scores were 39 (30–52), 48 (39–59) and 54 (50–59), respectively (Table 2). Trainees on average undertook 30 WPBAs over the 12 months. Overall service delivery was not adversely affected by the introduction of this training programme and there was no adverse effect on compliance with the specialty trainee rota or patient care.
Table 2.
Improvement in trainee satisfaction surveys since the start of the education pilot.
Since the start of the education pilot, further amendments were made to the renal curriculum in August 2010.5 The updated curriculum incorporates generic, leadership and health inequalities competencies. Our results are still valid for the new curriculum, as it continues to place emphasis on competency-based training.
In the last three years, external organisations have commended the renal specialty training programme at UHBFT. At the PMETB-scheduled review visit in June 2010, the unit was reported to offer ‘faultless high quality training’. Furthermore, at the renal programme review conducted by the NHS West Midlands Workforce Deanery in December 2010, the committee observed that ‘University Hospital Birmingham has a notable approach to providing high quality training utilising highly supportive educational resources and supervision arrangements, promoting a learning culture which is highly valued by all trainees’. Trainee satisfaction with the programme was confirmed externally in the national training surveys conducted by the General Medical Council in 2008–09 and 2010.6 This pilot was presented as a poster at the Renal Association Conference in May 2010, where it was well received.
Conclusion
This pilot indicates that it is possible to provide successful and high-quality specialty training in a busy clinical environment. The initial set up of such a programme is time intensive, but once established, it would require around 0.5 PAs per trainee per week. This pilot was undertaken in a renal unit with eight trainees and 10 consultants. This is an unusually large unit by usual standards in the UK and therefore is not representative of units providing training in the West Midlands. However, the principal findings of this study may be applicable to smaller units or those with different clinical requirements. The importance of the programme manager is likely to be similar regardless of the scale of the training programme or the specific clinical environment involved. The model outlined in this report could therefore form a template for delivery of postgraduate medical training in a diverse range of contexts.
References
- 1.Joint Royal Colleges of Physicians Training Board. Specialty training curriculum for renal medicine 2007 and assessment blueprint. London: JRCBPT, 2010. www.jrcptb.org.uk/specialties/ST3-SpR/Documents/2007%20Renal%20Medicine%20Specialty%20Training%20Curriculum.pdf [Accessed 25 May 2012] [Google Scholar]
- 2.Royal College of Physicians. Implementation of the European Working Time Directive in 2009 – implications for UK clinical service provision and training for medical specialties. London: RCP, 2009. http://old.rcplondon.ac.uk/professional-Issues/workforce/Workforce-issues/Documents/EWTD-RCP_2009_surveys.doc [Accessed 25 May 2012] [Google Scholar]
- 3.Roff S, McAleer S, Skinner A. Development and validation of an instrument to measure the postgraduate clinical learning environment for hospital based junior doctors in the UK. Med Teach 2005;27:326–31. 10.1080/01421590500150874 [DOI] [PubMed] [Google Scholar]
- 4.NHS West Midlands Workforce Deanery. JEST (job evaluation survey tool) distribution 2012. Birmingham: NHS West Midlands Workforce Deanery, 2012. www.westmidlandsdeanery.nhs.uk/JESTSurvey.aspx [Accessed 25 May 2012] [Google Scholar]
- 5.Joint Royal Colleges of Physicians Training Board. Specialty training curriculum for renal medicine 2010. London: JRCBPT, 2010. www.jrcptb.org.uk/specialties/ST3-SpR/Documents/2010%20Renal%20Medicine%20Curriculum.pdf [Accessed 25 May 2012] [Google Scholar]
- 6.General Medical Council National Training Surveys. Outlier summaries: trainee survey 2011. Manchester: GMC, 2011. http://gmc-onlineeducationreports.org/OutlierSummaries.aspx [Accessed 25 May 2012] [Google Scholar]


