Abstract
By the beginning of July 2009 the West Midlands had seen more cases of novel H1N1 influenza (swine flu) than any other region in the UK. Over a three-week period almost 850 people presented to Heartlands Hospital with flu-like symptoms. Of those admitted 52 adults were subsequently confirmed as having H1N1 infection. Most were younger than 30 and not from traditional influenza risk groups. The main risk factor for severe disease was asthma, and to a lesser extent pregnancy and obesity. Seven patients were admitted to intensive care and five developed an acute lung injury requiring prolonged admission. Two patients required extra corporeal membrane oxygenation and one died. Despite increased workload normal clinical services were unaffected. The hospital was not closed to admissions nor was it paralysed by staff absence. With a predicted second wave expected at the end of 2009, efforts to maintain effective community assessment remain crucial.
Key Words: diabetes, H1N1 subtype, influenza A virus, obesity, pregnancy, swine flu
Introduction
Between April and July 2009 a novel strain of H1N1 influenza (swine flu) spread rapidly around the globe. The first case in the UK was reported from Scotland in April 2009 and on the 2 July it was announced that efforts at containing the spread of the virus in the UK were to be abandoned. At this time the West Midlands had 2,582 confirmed cases, more than any other region in the UK.1
Heartlands Hospital is a large teaching hospital in East Birmingham serving a relatively deprived and ethnically diverse population of approximately 300,000 people. This paper describes the impact of H1N1 influenza in adults, the strategies used to deal with it, and the clinical features seen.
Overview
The first case admitted to Heartlands Hospital was on 7 June 2009, and from 15 June there was a sudden increase in numbers of patients presenting to the emergency department with flu-like illness. Over the next three weeks 847 patients attended the emergency department with the same symptoms. Of those admitted, 52 adults were subsequently confirmed virologically as having H1N1 infection. Seven required intensive care treatment, two required extra corporeal membrane oxygenation (ECMO) and one died. Figure 1 shows the timing of adult admissions peaking at five per day on 25 June 2009. Admissions reduced dramatically after this date.
Fig 1.
Timing of adult admissions for swine flu.
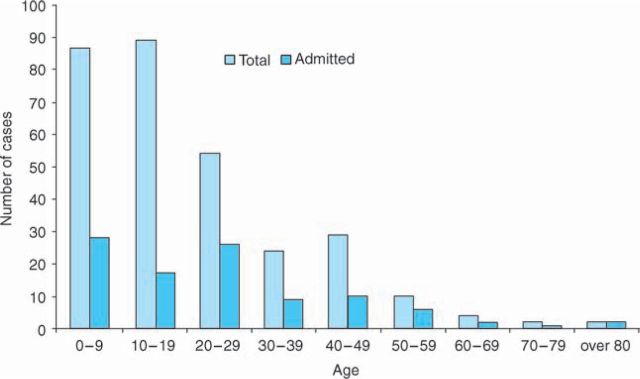
The Health Protection Agency (HPA) regional virus laboratory for the West Midlands is situated at Heartlands Hospital. Swine flu testing was performed according to a nationally agreed protocol using a pan-influenza A polymerase chain reaction (PCR), and two swine flu-specific PCRs (targeting the haemagglutinin and neuramidinase genes).2 Over the same three-week period the laboratory processed 7,650 flu swabs from the region. Of these specimens, 85% were from the city of Birmingham and 38% (3,000) were confirmed as swine flu. Figure 2 shows all positive swab results from the Heart of England Foundation Trust divided by age group. The majority of infected individuals were younger than 30 years old but only a minority of patients required hospital admission.
Fig 2.
Cases of influenza H1N1 A infection at Heart of England Foundation Trust.
Emergency department and admission policy
Over the course of a 48-hour period there was a 25% increase in attendances resulting in up to 80 extra patients a day. Significant numbers had been advised to attend by general practitioners (GPs) and NHS Direct. To deal with this surge and reduce the chance of nosocomial transmission, a dedicated flu assessment area was created within the emergency department. The main corridor became a flu waiting area with two rooms along this corridor designated for triage and assessment. Patients were assessed using a simplified version of the Department of Health (DH) criteria (Table 1).
Table 1.
Department of Health guidelines on assessing potential cases of swine flu.

Those individuals meeting inclusion criteria had swabs taken for influenza and those with markers of severity were admitted. Patients were also admitted if there was another reason for clinical concern such as persistent vomiting. This screening process was sustained for two weeks until community services for pandemic flu were fully operational. At no point did the hospital have to close to admissions. Community assessment absorbed a significant amount of the emergency department's workload and attendances declined dramatically.
Adult patients requiring admission
Following the announcement of the first cases of H1N1 in the UK, a number of side rooms were prioritised for treating suspected cases. Those meeting criteria for severe disease were admitted directly to these beds from the emergency department whenever possible. Oseltamivir was started on clinical suspicion rather than waiting for swab results, and patients received their first dose before leaving the department. Pregnant women received inhaled zanamivir. Most patients improved rapidly with antiviral treatment and were discharged early to complete their courses at home. Median length of stay (excluding intensive care unit (ICU) patients) was two days.
Infection control
Standard infection control policies were adopted with FFP2 masks, aprons and gloves. There was no evidence of any nosocomial spread. Initial efforts to offer prophylactic treatment to staff members were abandoned once the scale of the outbreak became apparent. Instead members of staff were advised to contact occupational health at the first sign of a flu-like illness. Although some members of staff did report such symptoms, there was no significant increase in total staff sickness compared to the same months last year.
Communication
Swine flu guidelines were posted on the hospital intranet homepage and briefing sessions were organised for clinical staff in relevant areas. Special efforts were made to meet with the obstetrics and gynaecology department to raise awareness of the emerging evidence of risk to pregnant women.
Demographics of confirmed cases
Table 2 shows the clinical and demographic features of all adult patients admitted with confirmed H1N1 infection. Although 52 confirmed cases were admitted only 19 met criteria for severity. The vast majority of patients were of an Asian ethnic background and were mainly from the local Mirpuri community originating from northern Pakistan. Of patients admitted, 69% were women, and 10 of these were pregnant (28% of all female admissions). Three of the pregnant women met criteria for severe disease and one pregnant woman without any other known medical problems was admitted to intensive care with respiratory failure.
Table 2.
Demographics and clinical features of adults with confirmed swine flu.
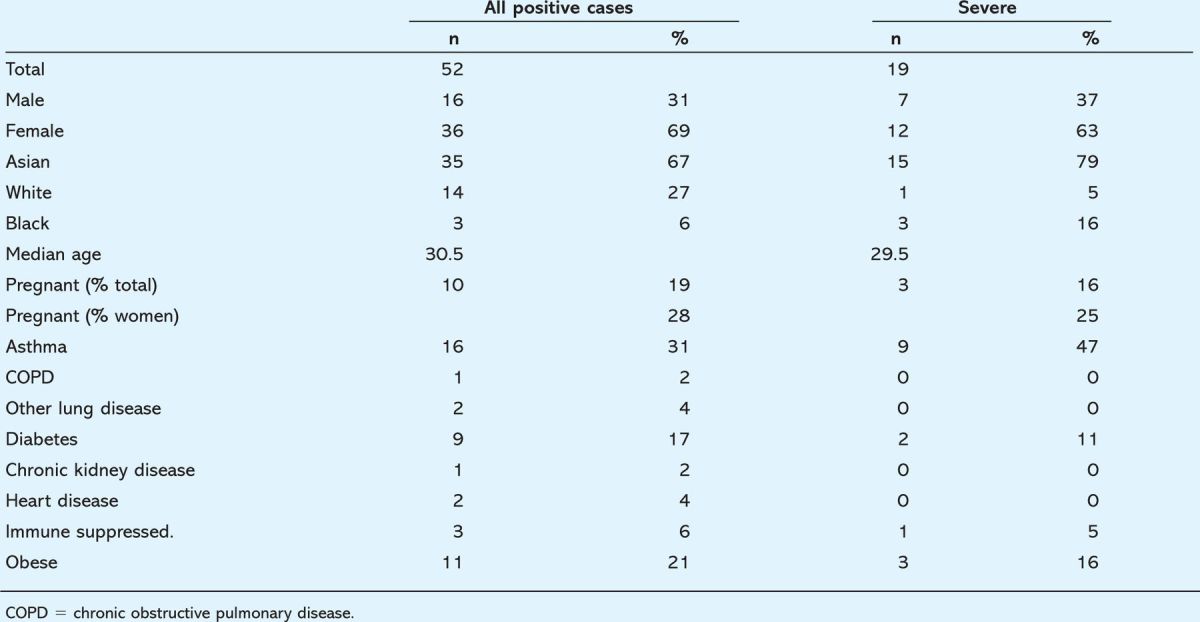
Underlying medical problems
Patients with asthma made up a third of adult admissions and almost half of the severe cases. Very few cases were seen in patients with other chronic lung conditions and those with chronic heart, kidney or neurological disease. Of severe cases 16% had been described as obese in their medical notes but body mass index was not routinely recorded.
Of those admitted, 17% had a diagnosis of type 2 diabetes. However, the prevalence in the catchment area was estimated to be up to 25%.3 Only two patients with diabetes met criteria for severe disease and both of these had underlying asthma.
Radiological features and laboratory investigations
In those patients admitted to the ward with confirmed H1N1 little evidence was found of bacterial pneumonia (only two patients had evidence of new infiltrates on chest X-ray). In 80% of cases neutrophil count was within normal limits and C-reactive protein less than 100. However, patients requiring intensive care frequently had infiltrates and consolidation on chest X-ray. It was suspected that this was secondary bacterial infection rather than a primary viral pneumonia/pneumonitis but cultures of respiratory secretions remained sterile. Unfortunately in many cases patients had received broad spectrum antibiotics prior to samples being taken.
Hypoxia and wheeze were common features in severe cases, often associated with underlying asthma. Eight individuals (15%) were hypoxic despite having normal chest X-ray and no underlying lung disease. Additionally five patients (10%) with no past history of asthma had persistent wheeze and required nebulised bronchodilators and oral steroids. These features were highly predictive of H1N1 infection.
Patients requiring intensive care
The high dependency unit was used exclusively for confirmed H1N1 cases and admitted seven patients (13% of all adult admissions). Two patients required only overnight admission, one who presented with confusion and fever who required intubation for a computed tomography scan (the agitation was subsequently attributed to an underlying psychological condition). The other had myasthenia gravis and required short-term ventilatory support but did not develop any lung infiltrates.
The remaining five all had lung infiltrates, usually bilateral, and required prolonged ventilation. Adult respiratory distress syndrome (ARDS) was a common factor and two patients required ECMO (Table 3).
Table 3.
Characteristics of individuals who required intensive care.
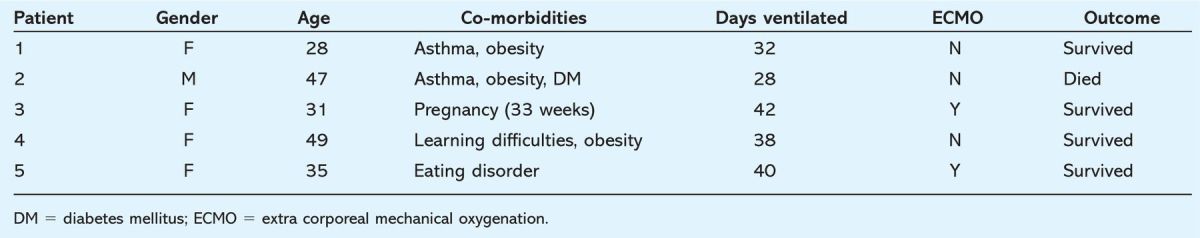
Patient 3 was 33 weeks pregnant on presentation. She was delivered by emergency Caesarean section after she developed respiratory failure and required intubation. The baby was transferred to the special care baby unit but did not display any signs of disease and was H1N1 negative.
All patients requiring intensive care were treated with doubledose oselamivir (150 mg twice daily) as is recommended by some in South East Asia for the treatment of H5N1.4 Unfortunately patient 2 died despite maximal intensive case treatment. He was later found to have H1N1 which was resistant to oseltamivir.
Discussion
The abrupt rise and fall in cases seen at Heartlands Hospital was likely to be due to the rapid spread of the H1N1 virus through the local, close-knit Mirpuri community. This community is ideally suited to the spread of respiratory infection with above average household numbers and large numbers of children.5
The majority of infections were in adults under 30 and in children. This is similar to reports from the USA and is in contrast to seasonal influenza where the elderly are mainly affected.6 The relative sparing of the older age groups is thought to be due to residual H1N1 immunity from previous influenza strains and is similar to patterns seen in previous pandemic years.7,8
The vast majority of cases appear to have been mild, with rapid improvement seen even in patients displaying signs of severity. The most common condition associated with severe disease was asthma. Reports from the USA have suggested obesity to be a risk factor for severe disease.9 In our cohort, three patients in the ICU were obese but had other co-morbidities including asthma.
There has been a great deal of discussion about the risk of H1N1 influenza to pregnant women, with cases of severe pneumonia and respiratory failure reported.10 Previous studies have shown that pregnant women have been at increased risk of developing severe disease with all strains of influenza not just H1N1.11 Ten of the studied inpatients were pregnant but there is likely to have been an admission bias as only three of these women met criteria for severe disease. The small numbers involved make it difficult to determine whether this is a significant independent risk factor for severe disease but one woman who required ICU admission and ECMO had no risk factors other than pregnancy.
Diabetes has long been described as a risk factor for severe influenza infection,12 however only two of the 19 patients who met criteria for severe disease were diabetic (11%) and both of these had asthma as well. Given the high background prevalence in these patients it was not felt that diabetes was a significant risk factor for developing severe disease with H1N1.
In addition the lack of any severe cases seen in patients with chronic heart, kidney or neurological disease suggests that the traditional putative risk factors for severe influenza do not apply in this current pandemic. This may reflect the age of those affected but it warrants more detailed prospective study.
Conclusions
In summary it is felt that Heartlands Hospital coped well with the first wave of the swine flu pandemic. It did not close to admissions and was not paralysed by staff absence. The DH criteria worked well but severity factors could be simplified further to focus specifically on hypoxia and signs of shock. Despite efforts to ensure good communication there remained problems ensuring that all relevant clinical staff were familiar with protocols.
Recommendations
-
Community assessment is essential to prevent hospitals being swamped with huge numbers of cases.
• Emergency departments should have a specific triage area for assessing suspected flu cases.
A number of side rooms should be dedicated to managing suspected cases.
The ICU should have facilities to separate swine flu cases from other ICU patients.
Protocols should be kept as simple as possible, keeping admission and severity criteria to an evidence-based minimum.
Regular briefing of key clinical staff is essential.
Data should be collected prospectively to establish who is genuinely at risk of severe disease.
Acknowledgements
The authors would like to thank clerical and medical staff in the Departments of Infection and Tropical Medicine, Virology and Emergency Medicine for their help in collecting data.
References
- 1.Health Protection Agency. Swine-lineage influenza A H1N1: UK update − 2 July 2009.
- 2.Health Protection Agency. Investigation of swine-lineage influenza A/H1N1v using the quadriplex influenza A PCR assay with swine-lineage influenza A H1 and N1 assays. www.hpa-standardmethods.org.uk/documents/vsop/pdf/vsop49.pdf
- 3.Barnett AH, personal communication, 2009.
- 4.White NJ, Webster RG, Govorkova EA. What is the optimal therapy for patients with H5N1 influenza? PloS Medicine 2009;6(6). 10.1371/journal.pmed.1000091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birmingham City Council. 2001 census: religious groups profiles. www.birmingham.gov.uk
- 6.Novel Swine-origin Influenza A (H1N1) Investigation Team. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. New Engl J Med 2009;360:2605–15. 10.1056/NEJMoa0903810 [DOI] [PubMed] [Google Scholar]
- 7.Schoenbaum SC, Coleman MT, Dowdle WR, Mostow SR. Epidemiology of influenza in the elderly: evidence of virus recycling. Am J Epidemiol 1976;103:166–73. [DOI] [PubMed] [Google Scholar]
- 8.Housworth WJ, Spoon MM. The age distribution of excess mortality during A2 Hong Kong influenza epidemics compared with earlier A2 outbreaks. Am J Epidemiol 1971;94:348. [DOI] [PubMed] [Google Scholar]
- 9.Intensive care patients with severe novel influenza (H1N1) virus infection – Michigan June 2009. MMWR Weekly 2009;58L749–52. [PubMed]
- 10.Jamieson DJ, Honein MA, Rasmussen SA. et al H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009;374:429–30. 10.1016/S0140-6736(09)61304-0 [DOI] [PubMed] [Google Scholar]
- 11.Neuzil KM, Reed GW, Mitchel EF, Simonsen L, Griffin MR. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol 1998;148:1094–102. 10.1093/oxfordjournals.aje.a009587 [DOI] [PubMed] [Google Scholar]
- 12.Stuart-Harris CH. Influenza and other virus infections of the respiratory tract. London: Edward-Arnold, 1965. [Google Scholar]