Abstract
There is little evidence to support tube feeding in advanced dementia although it is still frequently used in acute hospital settings. Patients present with complex problems and are often unable to make decisions about their healthcare needs. Multidisciplinary teams may be challenged by the difficult ethical decisions they are required to make in the best interests of their patients. This paper guides decision making in the management of patients with dementia and dysphagia in the acute hospital setting. A structured approach to information gathering, assessment and management is outlined with practical application of recent published guidelines and research evidence, which ensures appropriate individualised care.
Key Words: acute care, dementia, dysphagia Introduction
Growing numbers of patients with dementia and dysphagia are being admitted to acute medical wards with complex problems including reversible or transient medical conditions, acute stroke or other neurological aetiologies. Some patients may be approaching the end of their disease process and may present a diagnostic challenge.
Current practice in the area of dysphagia and dementia is variable, with the use of artificial feeding, nasogastric (NG) tubes, percutaneous endoscopic gastrostomy (PEG) or radiologically inserted gastrostomy (RIG) frequently being used without adequate consideration of the suitability of such procedures. Clinicians should be aware that there is little evidence to support tube feeding in advanced dementia. The National Institute for Health and Clinical Excellence (NICE) guideline on dementia advises that tube feeding should only be considered where dysphagia is a transient phenomenon and that artificial feeding should not generally be used in people with severe dementia.1
Other recent publications help guide the decision-making process.2,3
Dementia and dysphagia in acute hospital care
Swallowing problems may be caused by dementia or by other factors. Physical illness or metabolic upset may lead to acute confusional state in cognitively intact older people and those with dementia.4 Symptoms usually resolve once the acute illness has been treated. Acute confusion can impact on feeding and swallowing due to the decrease in functional skills and conscious level. It is well recognised that a decrease in swallowing efficiency and reserve in older people can result in dysphagia when acute physical illness is present.5 Certain medications have a detrimental effect on swallowing. Antipsychotics may cause Parkinsonism and dystonia.6 Antidepressants and benzodiazepines may cause drowsiness while other medications may lead to a dry mouth.
It is important to recognise and treat depression in dementia as significant improvement in mood and function is possible. Depression may lead to a range of problems including lack of appetite, reduced motivation to eat or feed oneself, abnormal ideation about food, for example that it is poison, or anxiety about eating and swallowing. In severe depression the person may have stopped eating altogether making an assessment of swallowing impossible. Neurological disorders should not be overlooked. This may be part of the process of dementia or evidence of newly acquired symptoms, such as acute stroke.
Information gathering
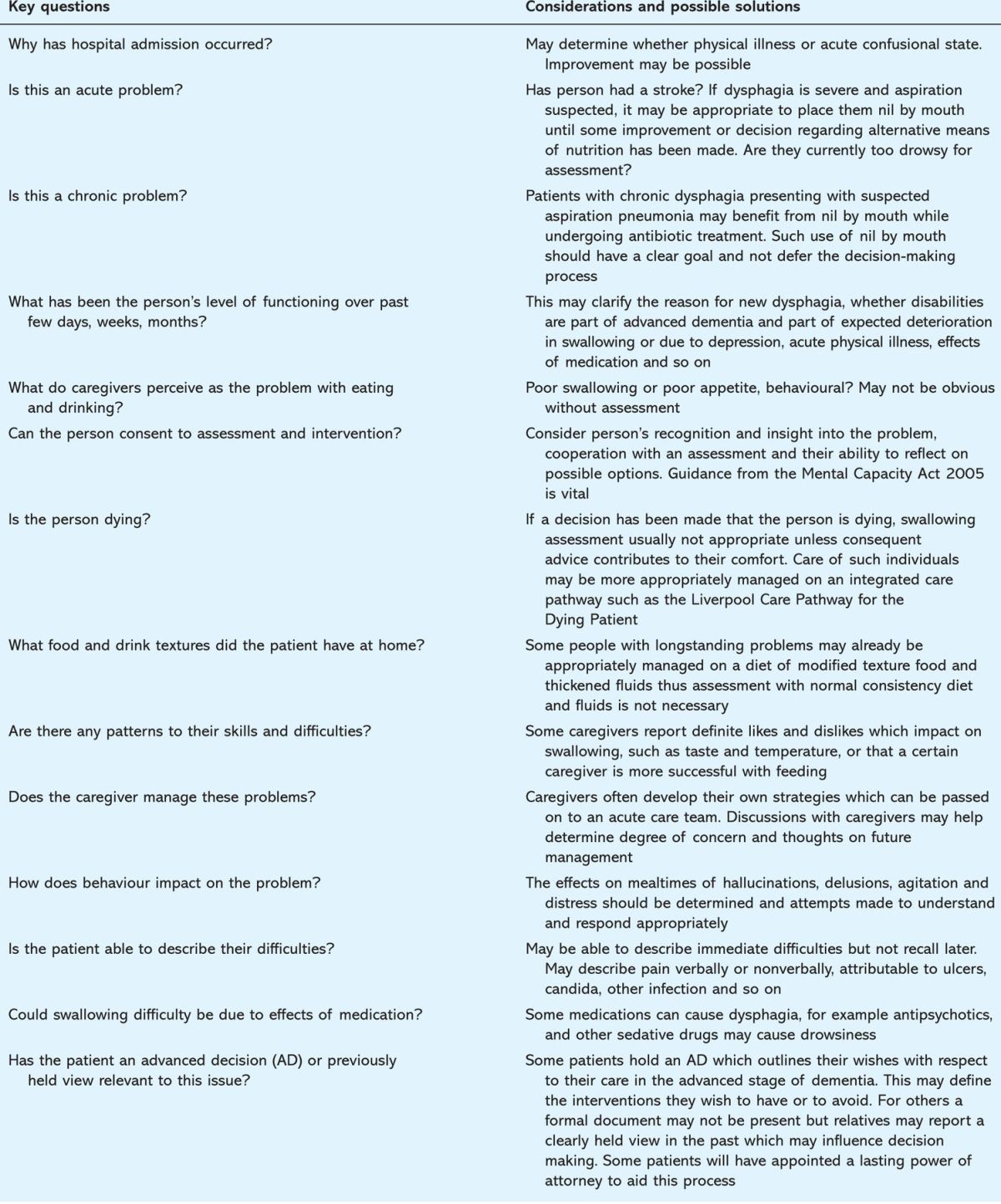
It is vital that a detailed history of the presenting problem and how it is managed is obtained to ensure that the most appropriate course of action is taken. Information may come from family members, professional caregivers from residential or nursing homes, ward or community mental health teams. Table 1 summarises questions designed to aid this process.
Table 1.
Key questions to ask as part of dementia and dysphagia information gathering.
Assessment of swallowing
Models of dysphagia assessment and management are often derived from the stroke population including bedside assessment of swallow efficiency with a variety of quantities and consistencies of food and fluid. Judgements are made as to the presence or absence of dysphagia, together with a subjective assessment of the presence or absence of laryngeal penetration/aspiration. More objective assessments such as videofluoroscopy may be considered in order to fully assess the swallow as well as to test compensatory strategies.7 Where problems of understanding and cooperation exist a more functional approach is required, such as observation of the patient while drinking or eating.8
Results of the assessment and information gathered from caregivers should be discussed within the team to ascertain if the difficulties presented are due solely to the dementia and are therefore an expected part of the disease at that stage. A dementia rating scale may aid this process.9 Those treatable and reversible causes outlined above should be clearly assessed and effectively managed and treated. If the medical team feel further specialist dementia assessment is required then a referral should be made to the older people's mental health services.
Management issues
Mild to moderate swallowing problems
If the problems with swallowing are assessed to be of a mild to moderate nature then a variety of compensatory strategies should be explored using a problem-solving approach. Difficulties may be managed by changing dietary texture, for example using thickened fluids, softer and eventually pureed foods alongside ensuring an upright posture, if possible, for eating and drinking. Smaller more frequent portions may be necessary together with favourite foods and nutritional supplements. The care plan should be realistic and achievable in the individual's care setting and should be clearly communicated to all involved. Training may be required on appropriate feeding techniques, for example appropriate pace, communication, verbal and nonverbal cues and so on. Good mouth care is vital in those at risk of aspiration to reduce oral bacteria and for those in whom food residue is present after a meal.10
Severe swallowing problems
If swallowing problems are severe, other available options should be considered. These are:
to continue with careful oral feeding
artificial hydration (temporary)
NG feeding (temporary)
PEG or RIG
to stop feeding.
Recent publications guide decision making in this area following concern as to whether tube feeding in advanced dementia is appropriate.1,2 A range of factors are cited, for example:
tube feeding does not prevent aspiration11
those with tubes do not survive any longer or may have a shorter survival12,13
the procedure is not without risk and there appears to be a worse prognosis in dementia.
It is of note that the literature generally refers to dysphagia occurring in advanced dementia. Little research exists for those individuals who experience significant dysphagia in the milder stages of dementia and for whom option analysis and prognosis may be different.
An approach which considers the individual and not solely the diagnosis is needed. This involves reflection on ethical, legal and cultural issues with respect to the individual concerned. The team should establish whether the person has capacity to consent, has made an advance decision outlining their wishes, or has appointed someone to make healthcare decisions on their behalf should they lose capacity (lasting power of attorney). If the person is not able to make a decision about tube feeding then the doctor should act in their best interests with the benefit of assessment findings and evidence. Best practice dictates that families should be consulted in this process even if no formal legal arrangements have been made as this provides valuable insight into the patient's previous wishes.14 Doctors may ask colleagues from older people's mental health, medicine for the elderly or palliative care for a second opinion.15 Benefits, risks and burdens for each individual should be evaluated with respect to oral and non-oral feeding and each option appraised. Consideration should be given to the patient's prognosis and the specific goals of care.16
It is important that the various roles and responsibilities of all concerned are clear and that once a decision has been made relevant disciplines involved in the care of the patient are not ‘out of the loop’. All concerned should agree on and understand the care plan. A date should be set to review the decisions made and whether this course of action remains appropriate. It is well recognised that not all patients will necessarily fit into clear models of care as outlined in Fig 1. However, at all times multidisciplinary team working is the key to effective communication and management. Any local guidelines for assessment and management should be part of this process.
Fig 1.
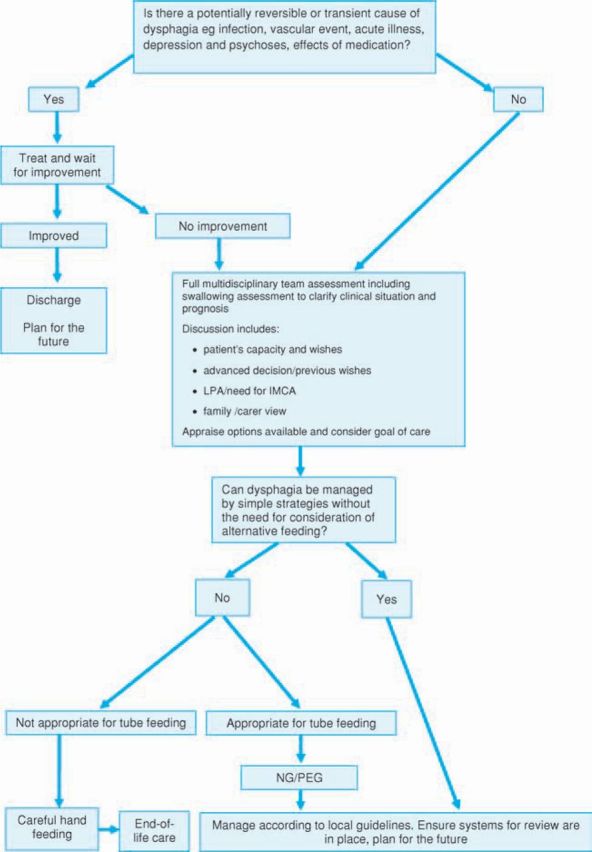
Dementia and dysphagia in acute hospital care decision-making. IMCA = independent mental capacity advocate; LPA = lasting power of attorney; NG = nasogastric; PEG = percutaneous endoscopic gastrostomy.
Palliative approaches
Approaches used in palliative care are increasingly applied to patients with dementia.17 Palliative care is delivered by all health and social care professionals with support from specialist palliative care services. Good communication between the family and healthcare team is vital as the process is designed to support carers through difficult circumstances and into bereavement. The NICE dementia guideline advocates ‘a palliative care approach from diagnosis until death to support the quality of life of people with dementia and to enable them to die with dignity and in the place of their choosing’.1 This approach considers physical, psychological, social and spiritual needs and ensures that people with dementia have the same access to palliative care services as others. An admission to acute care may provide a valuable opportunity for future care planning for people with dementia and dysphagia (Fig 1).
The dementia guideline advises encouraging people with dementia to eat and drink by mouth for as long as possible. Palliative interventions include good feeding techniques where food is offered but not forced. If the patient is dying then food and drink may not be wanted or needed. Constant and distressing attempts to encourage eating and drinking should be reviewed and if necessary discontinued. Mouth care, ice chips and artificial saliva products may be used to promote oral comfort. Pain and symptom control are essential as these are often under treated in dementia. Principles of a care of the dying pathway, such as the Liverpool Care Pathway for the Dying Patient, should be considered.18
References
- 1.National Institute for Health and Clinical Excellence. Dementia: supporting people with dementia and their carers in health and social care. London: NICE, 2006. [Google Scholar]
- 2.National Institute for Health and Clinical Excellence. Nutrition support in adults: Oral nutrition support, enteral tube feeding and parenteral nutrition. London: NICE, 2006. [PubMed] [Google Scholar]
- 3.Department of Constitutional Affairs. Mental Capacity Act Code of Practice. Norwich: Stationery Office, 2007. [Google Scholar]
- 4.Young J, Inouye SK. Delirium in older people. BMJ 2007;334:842–6. 10.1136/bmj.39169.706574.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bucholz DW, Bosma JF, Donner MW. Adaptation, compensation and decompensation of the pharyngeal swallow. Gastrointest Radiol 1985;10:235–9. 10.1007/BF01893106 [DOI] [PubMed] [Google Scholar]
- 6.Sokoloff LG, Pavlakovic R. Neuroleptic-induced dysphagia. Dysphagia 1997;12:177–9. 10.1007/PL00009533 [DOI] [PubMed] [Google Scholar]
- 7.Smith HA, Connolly MJ. Evaluation and treatment of dysphagia following stroke. Topics Geriatr Rehabil 2003;19:43–59. [Google Scholar]
- 8.Kindell J. Feeding and swallowing disorders in dementia. Milton Keynes: Speechmark Publishing, 2002. [DOI] [PubMed] [Google Scholar]
- 9.Reisberg B, Ferris SH, De Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry 1982;139:1136–9. [DOI] [PubMed] [Google Scholar]
- 10.Langmore SE, Terpenning MS, Schork A. et al Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia 1998;13:69–81. 10.1007/PL00009559 [DOI] [PubMed] [Google Scholar]
- 11.Peck A, Cohen CE, Mulvihill MN. Long-term enteral feeding of aged demented nursing home patients. J Am Geriatrics Soc 1990;38:1195–8. [DOI] [PubMed] [Google Scholar]
- 12.Mitchell SL, Kiely DK, Lipsitz LA. The risk factors and impact on survival of feeding tube placement in nursing home residents with severe cognitive impairment. Arch Intern Med 1997;157:327–32. [PubMed] [Google Scholar]
- 13.Mitchell SL, Kiely DK, Lipsitz LA. Does artificial enteral nutrition prolong the survival of institutionalized elders with chewing and swallowing problems? J Gerontol A Biol Sci Med Sci 1998;53:M207–13. 10.1093/gerona/53A.3.M207 [DOI] [PubMed] [Google Scholar]
- 14.Alzheimer's Society. Making difficult decisions. London: Alzheimer's Society, 2006. [Google Scholar]
- 15.British Medical Association. Withholding and withdrawing life-prolonging medical treatment, guidance for decision making. London: BMA Books, 2007. [Google Scholar]
- 16.Mitchell SL. A 93-year-old man with advanced dementia and eating problems. JAMA 2007;298:2527–36 10.1001/jama.298.17.jrr70001 [DOI] [PubMed] [Google Scholar]
- 17.Department of Health. End of life care strategy. London: DH, 2008. [Google Scholar]
- 18.Liverpool Care Pathway. www.lcp-mariecurie.org.uk


