Abstract
An acute medicine Royal College of Physicians report makes key recommendations. This study reviews organisational issues and consultant working patterns against these recommendations. Thirty-nine trusts in England and Wales were asked to participate in an online survey, which 27 completed. Twenty-six sites had an acute medical unit (AMU) and all had a lead consultant. Two trusts had no written operational policy. Of the 26 AMUs, 22 had at least level 1 facilities and 21 used an early warning score at point of entry to care. Ten reported a minimum of twice daily ward rounds seven days a week. Consultant of the day was the most common pattern of work. Ten trusts cancelled other clinical duties for consultants responsible for acute take. The pilot shows evidence of good practice in leadership and operational policies. Further work to standardise and improve acute care is needed including a more consistent twice daily consultant review.
Key Words: acute medicine, medical staffing, patient care management, physician's practice patterns, out-of-hours medical care
Introduction
Acute medicine has developed over the last decade in response to the increasing number of medical admissions, concerns over quality of acute care and other pressures including the European Working Time Directive.1,2 Defined acute medicine training programmes are now in place throughout the UK, with more new consultant posts to be appointed.3 Current staffing and rotas vary between hospitals and to date there has been little evaluation of the systems in place. Previously, the Royal College of Physicians (RCP) surveyed the numbers of posts in acute medicine and some elements of the systems in place but at the time this work was undertaken there were no recommended standards against which to judge the quality of services.4 In 2006, the National Institute for Health and Clinical Excellence (NICE) published a guideline on the management of acutely ill patients in hospital,5 while in 2007 the RCP published a comprehensive report on acute medicine and acute care6 and the National Confidential Enquiry into Patient Outcomes and Deaths also made recommendations for staffing and organisations of acute medical units (AMUs).7 The RCP report updated the definition of acute medicine and defined an AMU as a dedicated facility within the hospital that acts as the focus for acute medical care for patients who have presented as medical emergencies to the hospital or who have developed an acute medical illness while in hospital.6
Given the background of recent reports, the growth of acute medicine and the introduction of the new consultant contract it is an appropriate time to review organisational issues, including the role of the consultant in managing acute unselected medical admissions. This report describes the audit component of the first phase of a longer-term project designed to evaluate the role of the structure and organisation of acute medical care on patient outcomes.
Methods
A pilot project seeking information about the organisation and consultant staffing patterns of AMUs was designed for completion as an online questionnaire by a nominated senior NHS trust representative. The aim was to obtain responses from approximately 25 secondary care NHS trusts in England and Wales where the patterns of consultant cover for acute medical admissions have been stable for the 12 months from 1 April 2007 to 31 March 2008.
All secondary acute care NHS trusts in England and Wales were invited by letter to express interest in participation in the pilot study. From 112 respondents, 39 were selected to represent a range of types of trust by size, urban versus rural and geographical distribution. The nominated contact at responding trusts was approached by the study project manager, to explain the study and obtain the individual's consent to participate. The online questionnaire was constructed and hosted on a secure commercial website (www.surveymonkey.com).
Consenting nominated contacts were provided with individual login details for the pilot questionnaire. They were asked to complete the survey within two weeks of agreeing to take part. Non-responding contacts were sent an automatic email reminder two weeks after provision of their login details. Contacts who had still not responded a further two weeks after this reminder were telephoned by the study administrator and the reason for non-completion sought and recorded to inform the feasibility objective of the pilot. Where possible, any difficulty with completion (such as technical problems) was addressed and the contact encouraged to complete the questionnaire. Those who had not completed the questionnaire after a further two weeks were classed as non-responders and no further attempt was made to solicit their participation.
The study involved no change in the management of patients and no access to patient level data was required.
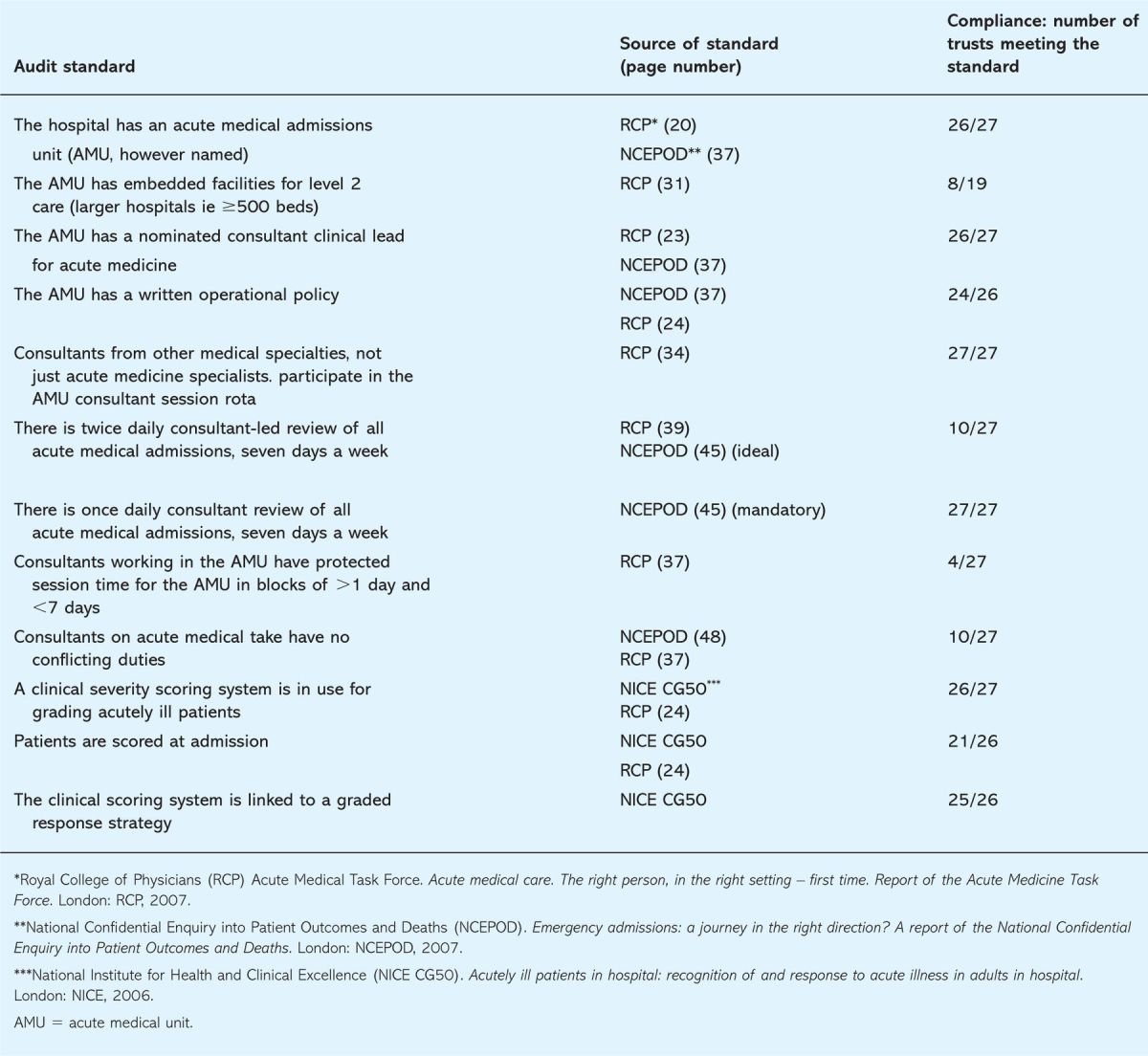
A set of audit standards (Table 1) were derived from three recently published reports which contain recommendations on the organisation and staffing of AMUs and the survey responses were compared against these standards.5–7 The responses were also used to provide additional descriptive analysis of the organisation of AMUs and patterns of consultant cover.
Table 1.
Audit standards and compliance.
Results
Twenty-seven of the 39 invited acute trusts (69%) completed the survey; all were hospitals in England and 19 were hospitals with 500 or more beds. Compliance with the audit standards is shown in Table 1. Twenty-six of the trusts have an AMU. Although the exact name may vary between trusts, all are classed as an AMU for the purposes of this audit. All 26 have designated lead consultants, 24 of which had a written operational policy. Twenty-two units had facilities for level 1 care (ie care of patients at risk of a deterioration in their condition). Of the 19 AMUs in larger hospitals (over 500 beds) eight had facilities for level 2 (high dependency unit) care embedded within the unit. Twenty-three AMUs admitted patients directly from general practice, bypassing the accident and emergency (A&E) department, though in 15 the AMU capacity was exceeded at least weekly resulting in redirection of patients. Eleven units had dedicated arterial blood gas analysers located within the unit. Twenty-six trusts used an early warning score to monitor patients, with 25 linking it to a graded response strategy, and 21 used the score at the point of entry to care.
Consultants from other specialties besides acute medicine are responsible for acute medical admissions in all 27 trusts surveyed, with the most common rota frequency being 1 in 12, and 19 of the trusts operating a rota between 1 in 5 and 1 in 15. Specialties most often reported as participating in the rota included: care of the elderly (n=22 trusts), gastroenterology (n=21), respiratory medicine (n=21), endocrinology/diabetes (n=21) and cardiology (n=12). Eighteen trusts reported employing acute physicians (mean 2.3 per trust with acute physicians and 1.5 for all trusts surveyed). In seven of these trusts the acute physicians are not part of the routine consultant on-call rota, either because they are never the primary consultant on-call (four trusts) or have a different on-call pattern (three trusts). Twelve trusts reported that acute physicians cover zero hours at the weekend. Nine trusts did not have a continuous admitting consultant presence.
Consultant ward rounds are conducted at least once daily, including at weekends, in all 27 trusts surveyed, but twice daily consultant review of patients on seven days a week was reported by only 10 of the trusts. In 15 trusts twice daily review is conducted on weekdays but not weekends. ‘Consultant of the day’ is the most prevalent pattern of work midweek, with 21 of the trusts operating this system on weekdays and the remaining two operating a ‘consultant of the week’ system. Continuous weekend cover by the same consultant or team of consultants is operated in 17 trusts.
Only 10 trusts reported the routine cancellation of other clinical duties and responsibilities for consultants with responsibility for acute medical admissions. Eight stated that additional duties were regularly undertaken at the same time as responsibility for acute medical admissions and nine stated that additional duties were sometimes undertaken. The most common of these duties were outpatient clinics (n=12), elective endoscopy (n=11), elective bronchoscopy (n=9) and elective angiography (n=6).
Discussion
Although this is a pilot survey and generalisation from the results should be made with care, some patterns seem to be emerging. In relation to current national recommendations and guidelines there is good adherence in some areas but in others the results indicate marked variation between hospitals.5–7 These areas, in particular will require further clarification to understand the implications for patient care and clinical practice. The results of the audit against the predefined standards indicate that the vast majority of hospitals (26/27) surveyed had an established AMU, that all had a designated clinical lead for acute medical take and that the majority had written operational policies in place.
Current recommendations support direct admissions to AMUs to reduce waits and delays for patients and offer general practice prompt opinion. The majority of AMUs in the study offered this service but the capacity of nearly half (48%) of the units accepting direct admissions is exceeded at some point in the average week. This results in patients being redirected to other units such as A&E and would suggest these trusts need to review their processes and capacity planning to resolve this to improve patient flow.
Four hospitals with AMUs stated that they did not have level 1 facilities embedded within the unit which potentially raises an issue about these units’ ability to monitor this group of acutely unwell medical patients. In contrast eight of the larger hospitals had level 2 facilities embedded within the AMU. Therefore for a small number of units admitting acutely unwell patients, monitoring and associated staffing levels are likely to be inadequate for the case mix and illness severity of patients admitted. Equally, less than half have an arterial blood gas machine within the AMU, which means that agreed rapid turnaround times from laboratories must be in place to meet current recommendations.
Only two sites do not appear to have an early warning score system in place. In the majority of sites this is now part of the routine first hospital assessment and is linked to a response protocol in agreement with national recommendations. All AMUs had direct involvement in the acute take from the main medical specialties, although this was less common for cardiology, nephrology and neurology. Support medical specialty input was much less common at weekends with the exception of care of the elderly and cardiology.
Midweek consultant patterns of working still reflect ‘consultant of the day’ in most trusts rather than the recommended ‘consultant of several days’. The recommended duration of continuous cover provided by consultants for acute medical patients, of more than one but less than seven days is adhered to in only four of the trusts surveyed. However, continuous cover by the same consultant(s) is more likely at weekends (66% of sites) with ‘consultant of the week’ being the least common working pattern. Unfortunately in 37% of the hospitals surveyed the first on-call consultant still undertakes other routine clinics or procedures while managing the acute take and in only 30% of hospitals do consultants routinely cancel other duties in line with recommendations. In only 10 hospitals are all patients within the AMU routinely seen twice per day, seven days a week.
Two thirds of the surveyed sites now employ acute physicians and on average these sites have 2.3 in post, which is still short of the recommended numbers although increasing numbers of trainees will complete their Certificate of Completion of Training in 2009. Most commonly acute physicians work extended days in the AMU. In 12 trusts acute physicians are covering weekend periods and in 11 sites they are integrated into the same on-call system as other participating consultants. A concern is the fact that few appear to have first-line responsibility for managing patients.
This pilot audit of acute medical care shows that some of the key recommendations are being met, particularly in relation to leadership and operational policies, including the use of an early warning score system. However, in structuring the consultant patterns of work, recommendations are less often met; many patients are only seen once per day in the acute phase of their illness and in up to a third of hospitals consultants are still undertaking simultaneous duties. A small number of units appear to a have poor monitoring or staffing facilities to manage acutely unwell medical patients.
The lack of input of some acute physicians at weekends is a potential area of concern given the data surrounding poorer weekend outcomes for patients.8,9 Equally, it is unclear why in a small number of the surveyed hospitals they have no first-line responsibility for care. Areas such as this need to be further explored to assess how this relates to outcomes and unit governance.
Another finding from this audit is that the use of an online survey tool was a practical and efficient means of obtaining responses from a large proportion of those invited to participate. It involved a minimal administrative burden in both the collection and analysis of results. The full pilot study report may be viewed on the RCP website (www.rcplondon.ac.uk).
This pilot audit suggests that progress is being made in the development of acute medicine, but highlights areas for further study in relation to acute medical care. It has confirmed the feasibility of the methodology and highlights the areas to be explored in a larger national survey, to test the emerging patterns seen in the pilot results.
References
- 1.Seward E, Greig E, Preston S. et al A confidential study of deaths after emergency medical admission: issues relating to quality of care. Clin Med 2003;3:425–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cullinane M, Findlay G, Hargraves C, Lucas S. An acute problem? London: National Confidential Enquiry into Patient Outcome and Death, 2005. [Google Scholar]
- 3.Joint Royal Colleges of Physicians Training Board. Acute medicine curriculum. www.jrcptb.org.uk/Specialty/Pages/AcuteMedicine.aspx
- 4.Mather H, Pounder R. Coping with problems in acute medicine in the post-WTD era: a survey of RCP College Tutors in December 2004. London: Royal College of Physicians, 2004. www.rcplondon.ac.uk/professional/spr/spr_ewtd05.htm
- 5.National Institute for Health and Clinical Excellence. Acutely ill patients in hospital: recognition of and response to acute illness in adults in hospital. London: NICE, 2006. [PubMed] [Google Scholar]
- 6.Acute Medicine Taskforce. Acute medical care. The right person, in the right setting – first time. Report of the Acute Medicine Task Force. London: RCP, 2007. [Google Scholar]
- 7.National Confidential Enquiry into Patient Outcomes and Deaths. Emergency admissions: a journey in the right direction? A report of the National Confidential Enquiry into Patient Outcomes and Deaths. London: NCEPOD, 2007. [Google Scholar]
- 8.Bell CM, Redelmeier DA. Mortality among patients admitted to hospital on weekends as compared with weekdays. N Engl J Med 2001;345:663–8. 10.1056/NEJMsa003376 [DOI] [PubMed] [Google Scholar]
- 9.Kostis WJ, Demissie K, Marcella SW. et al Weekend versus weekday admission and mortality from myocardial infarction. New Engl J Med 2007;356:1099–109. 10.1056/NEJMoa063355 [DOI] [PubMed] [Google Scholar]


