Abstract
Weekend handover is vital for patient safety–poor handover is a cause of avoidable adverse events. This study evaluated whether the quality of information handed over for patients requiring weekend review was adequate. Two external doctors imagined themselves as the doctor on-call and judged whether the handed-over information was adequate for each case. Of the 1,130 handovers evaluated, 867 were handed over using a computerised proforma and discussed at the handover meeting, 148 using the computerised proforma but not discussed, 30 handovers were handwritten. Of handovers of patient details and background information, 87.3% were judged of adequate quality by the first auditor and 86.0% by the second. Similarly 70.6% and 75.8% of handovers of action plans were of adequate quality. Use of computerised proforma and discussion at a handover meeting gave the highest percentage of handovers of adequate quality, however, there was room for improvement. Training in handover may improve communication.
Key Words: communication, handover, patient safety, sign-out
Introduction
Handover of patients is of critical importance in good clinical care. With new working time directives, junior doctor shift work has increased.1 Often doctors on-call at the weekend will be unfamiliar with patients needing review,2 relying on information on handover sheets. Handovers need to be clear and time efficient–communication failure as a cause of preventable adverse events and deaths has been a major concern of health systems for many years.3–5 One study found 24 adverse events arising from 503 patient night handovers.6 Common causes of such events were inadequate description of current patient condition, deficient anticipatory guidance and lack of explanation of rationale for management plans. Omitted content from handover was the most common cause of deleterious communication failure in another study.7 Illegible handwriting can also be a problem.
Queen's Hospital, Romford, is a large district general hospital with 340 general medical inpatient beds, 22 general and acute medical consultants and an average of 330 medical admissions each week. At the weekend there are nine junior doctors covering the acute medical take and the medical wards. It is only feasible to review a selected proportion of medical inpatients over the weekend. Given the importance of safe handover, a service evaluation of the quality of information handover for medical inpatients needing weekend review was conducted.
Method
Phase 1–Entering of information
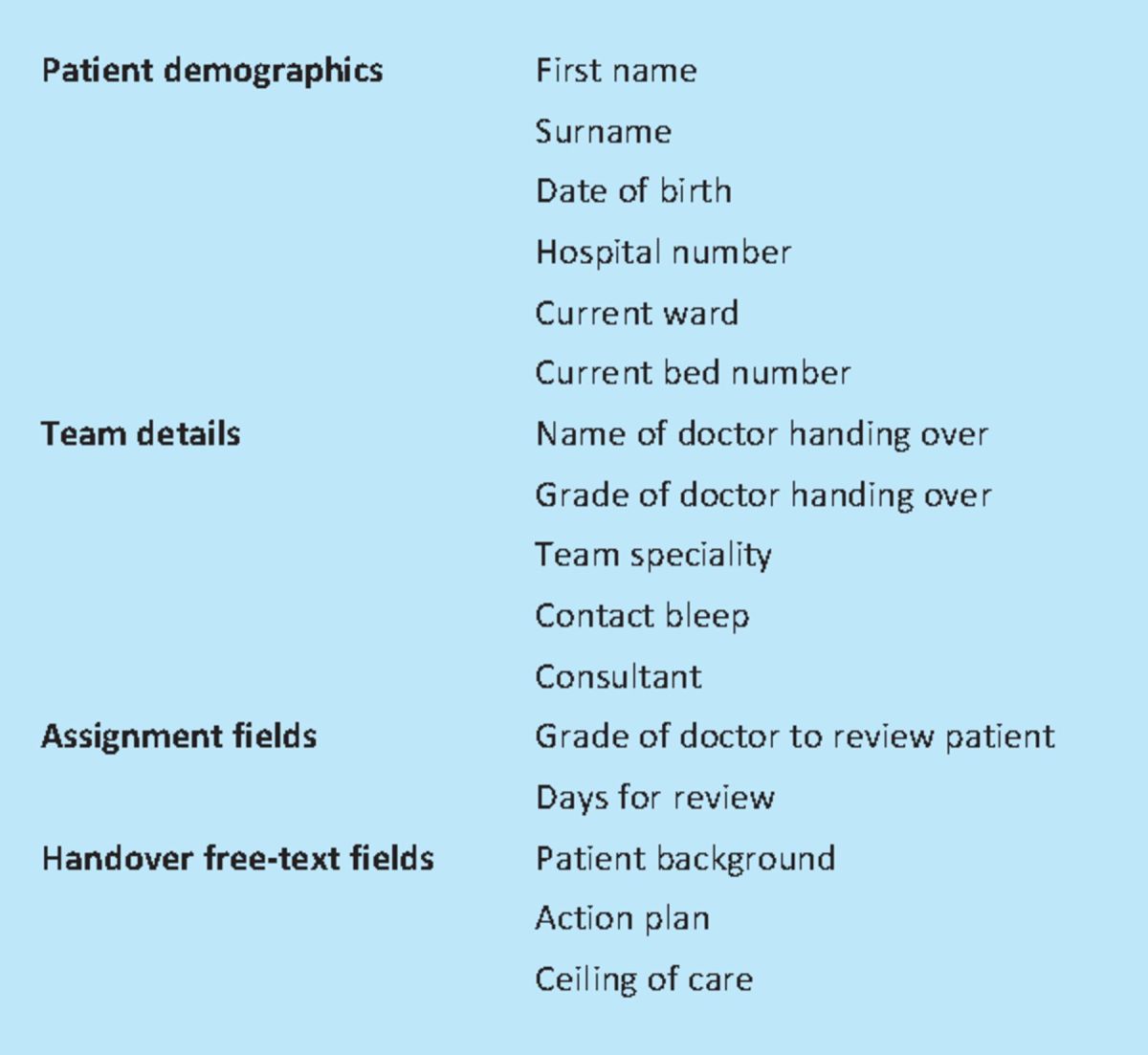
Patients needing weekend review were identified by their routine weekday team and their information entered onto an electronic database tool before 4pm on a Friday. Data fields included patient details, clinical background and action plan (Table 1).
Table 1.
Fields for data entry on the electronic proforma.
Phase 2–Reviewing information at a handover meeting
A meeting was held at 4pm the same day–during the meeting all weekend handovers were discussed, clarified and database entries updated. Specific attention was given to the handover action plan and ceiling of care for each patient as they were discussed. It was attended by the weekend on-call team and the outgoing weekday teams.
Phase 3–Accomplishing the handover tasks
The weekend handover list was printed from the database and distributed to all the weekend doctors on Saturday morning. During the weekend, the handover team would use the list and work through the tasks.
Exceptions to the handover method
Some handovers did not follow all three phases of the handover model. A number of patient handovers were entered onto the database but not discussed as the referring doctor was unable to attend the meeting. Also a small number of patients were handed over on handwritten sheets, not entered onto the database before the weekend and not discussed at the meeting. These handwritten handovers were added retrospectively to the electronic database for audit purposes (by copying any handwritten handovers found at 6pm on Friday in the handover room onto the database).
Evaluation
To assess the quality of the data used in the weekend handover process two doctors-in-training (a registrar in respiratory (with general) medicine and a registrar in acute medicine) who had never worked at Queen's Hospital were asked to retrospectively score patient handovers for quality of information. All handovers were anonymised and auditors were blinded to manner of handover for each entry (whether originally via computerised proforma and whether discussed). The handwritten handovers were reviewed as they appeared on the electronic proforma to which they had been retrospectively added.
Six months of inpatient weekend handovers were evaluated. The independent doctors separately reviewed each handover entry on the database. They imagined themselves to be an on-call doctor receiving the handover sheets. The following aspects of each handover were evaluated to assess if they were of adequate quality:
patient details and background information
the handover action plan for the doctor on call attending the patient.
Each aspect was scored on a Likert scale as follows: 1–very poor quality, 2–poor quality, 3–acceptable quality, 4–very good quality. The target was for 95% of handovers of background information and 95% of handovers of action plans to be of acceptable or very good quality. The reason for each patient to be seen over the weekend was also characterised.
Differences in the percentages of handovers being of inadequate quality (poor or very poor quality) when computerised handovers were discussed at the meeting compared to when they were not discussed were calculated, along with 95% confidence intervals. The degree of agreement between the two auditors was assessed with the kappa statistic (Stata, version 11.1, Stata Corporation, College Station, Texas, USA). The kappa statistic was interpreted using previously defined guidelines.8
Results
In total, 1,130 weekend patient sequential handovers were reviewed. They occurred between February 2009 and August 2009. Of these, 919 handovers were of unstable patients needing weekend review and 82 were potential discharges. The remaining handovers related to routine care for stable patients (eg re-prescribing of intravenous fluids).
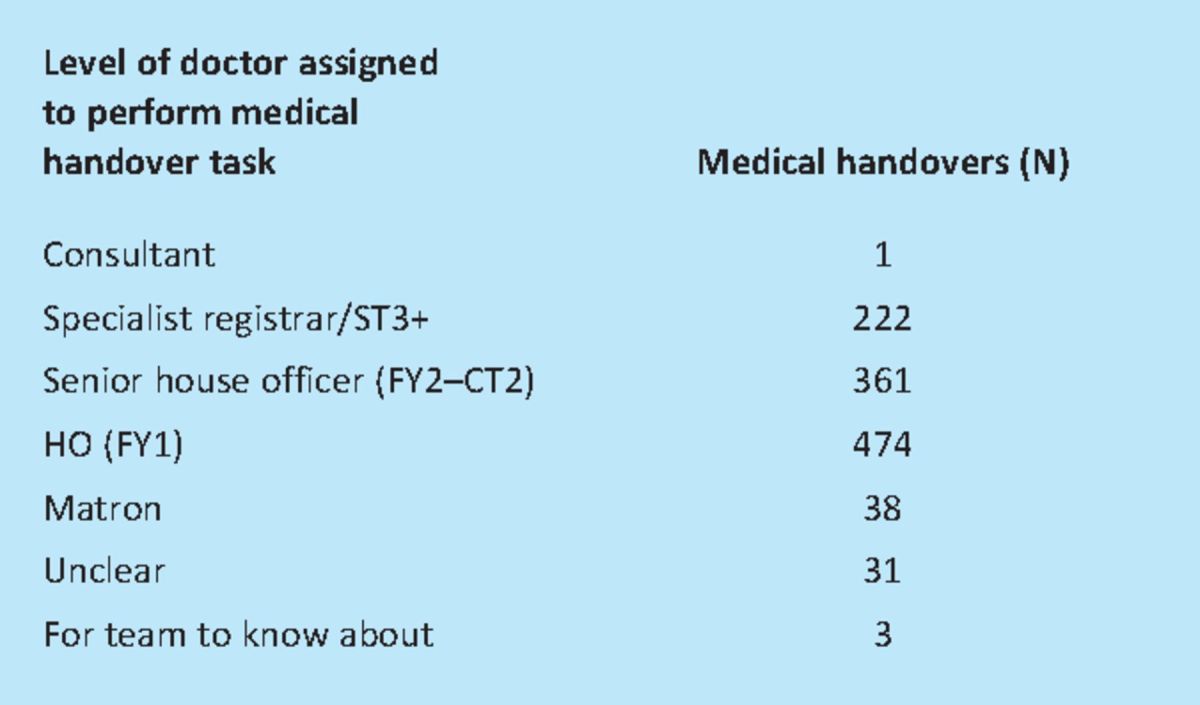
The medical conditions and problems of the patients to be reviewed by the general medical on-call team over the weekend were diverse, covering different medical specialties, and many patients had multiple medical problems covering more than one organ system (Table 2). The handover tasks were distributed between the grades of junior doctors (Table 3).
Table 2.
Number of medical handovers by specialty of problem to be reviewed. General medicine/multi-speciality indicates handovers not specific to a particular speciality (eg warfarin or urinary tract infection) and patients with problems across several organ systems (eg a patient with decompensated cardiac failure, pneumonia and acute on chronic kidney injury).
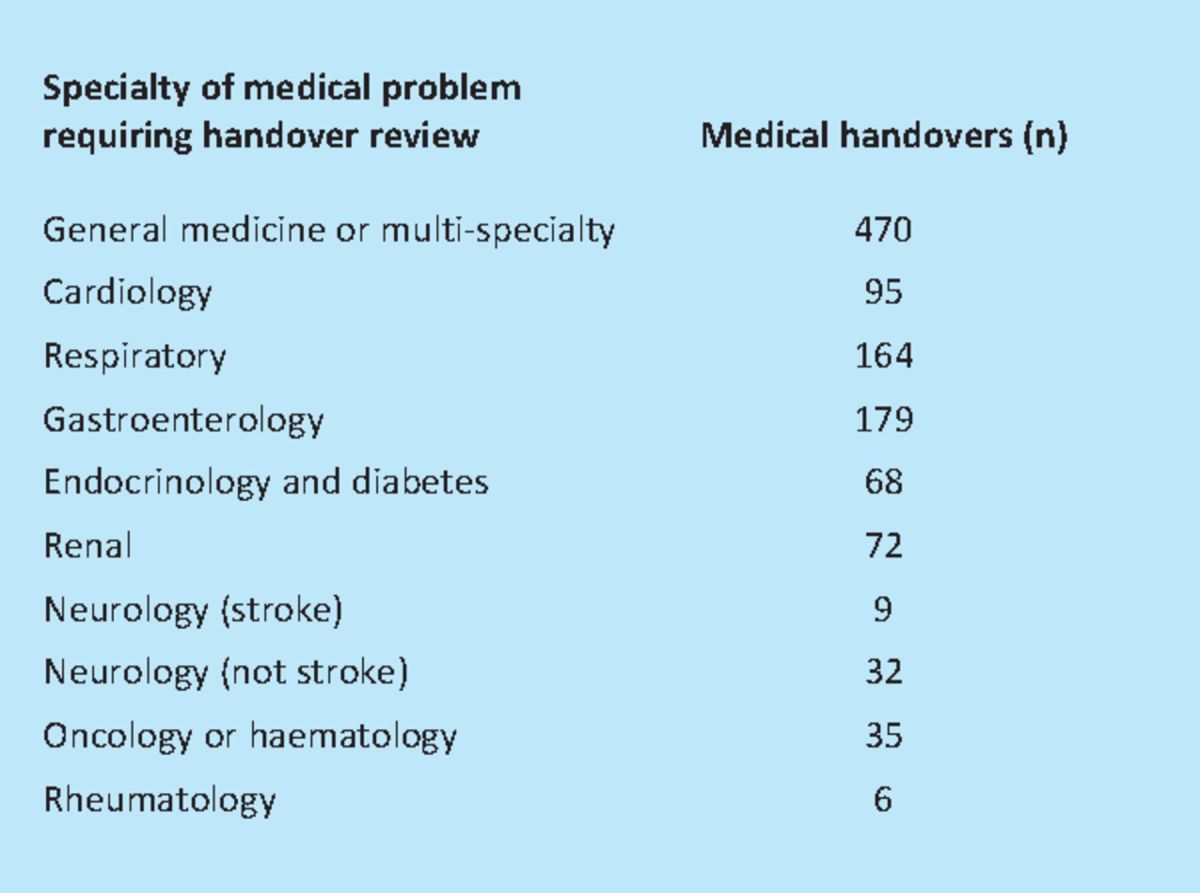
Table 3.
Number of handovers by grade of clinician requested to see patient. FY = foundation year; CT = core medical training; HO = house officer; ST = specialty training.
Details of 867 (76.7%) handovers were entered using a computerised proforma onto the database and discussed at the handover meeting; 148 (13.1%) were via the computerised proforma but not discussed; 30 (2.6%) were hand-written (and not discussed). The remaining 85 patient handovers were entered onto the database but it was not identified whether they were discussed at the meeting.
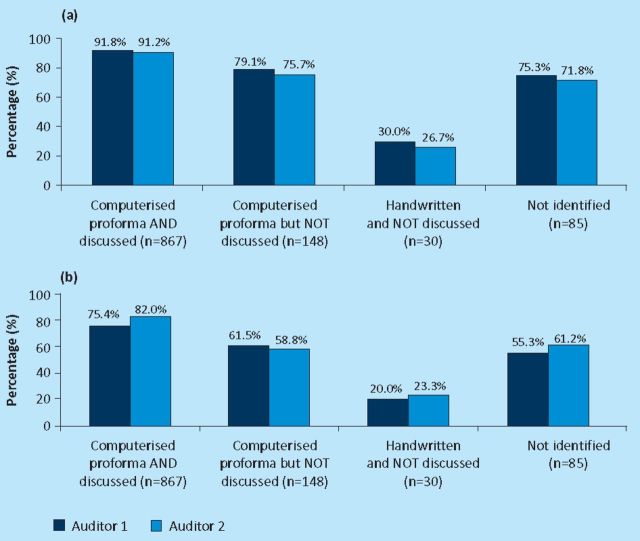
Auditor 1 judged only 87.3% of patient handovers of patient details and background information and only 70.6% of handovers of action plan to be of adequate (acceptable or very good) quality. Auditor 2 judged the handovers similarly at 86.0% and 75.8% respectively. The proportion of handovers of acceptable or very good quality was highest in patients handed over using the computerised proforma and discussed at the handover meeting (over 90% for handover of patient background and over 75% for handover of action plan) compared to other handover methods with both auditors (Table 4 and Fig 1). Less than a third of handwritten handovers were judged of acceptable or very good quality (Fig 1).
Table 4.
Numbers of handovers by scored quality and method of handover.
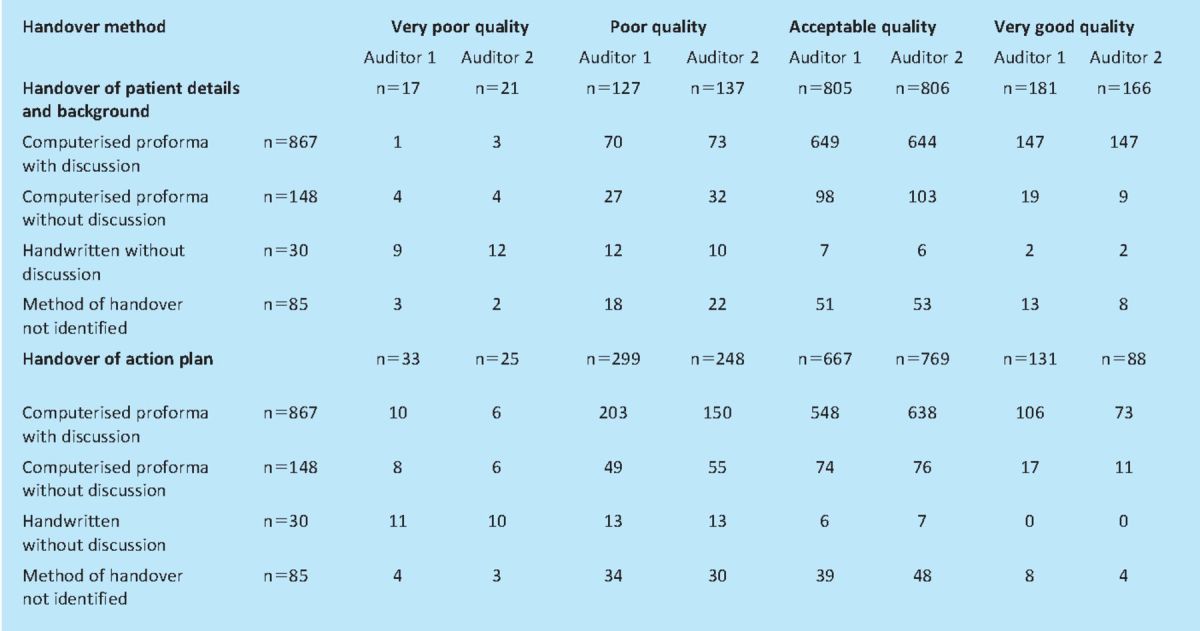
Fig 1.
Percentage of handovers judged to be of acceptable or very good quality by handover method. (a) patient details and background; (b) action plan.
The likelihood of inadequate quality handover was significantly lower when the handover was computerised and discussed at a meeting, compared to when the handover was computerised but not discussed. The differences in the percentage of handovers of inadequate quality (95% confidence interval (CI)) for handover of patient background were 12.8% (CI 6.0–19.6%) and 15.6% (CI 8.4–22.7%) for auditors 1 and 2 respectively. For action plan, the differences in the percentages were 13.9% (CI 5.6–22.3%) and 23.2% (CI 14.9–31.6%).
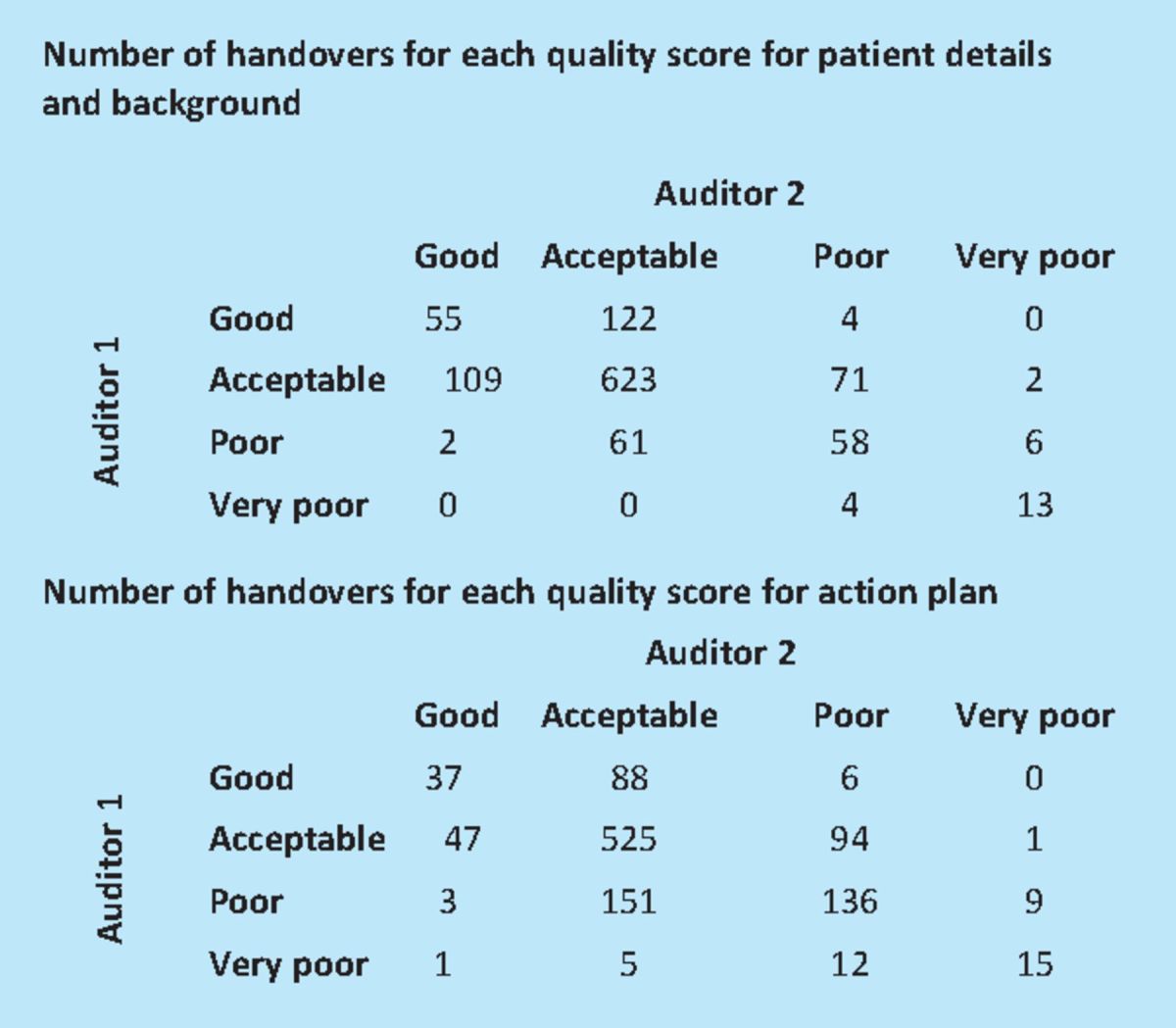
There was moderate agreement as to whether individual handovers were of acceptable or very good quality (as opposed to poor or very poor quality) between the two auditors for both patient background and action plan–kappa statistics (95% CI) of 0.465 (CI 0.390–0.540) and 0.413 (CI0.354–0.472)–using previously defined interpretations of the kappa statistic.8 Table 5 shows how the quality scoring for handovers compared between auditor 1 and auditor 2. Although there is only moderate agreement for individual handovers, most importantly there was agreement between the scoring of both auditors in both showing that the risk of inadequate handover was lowest when the handovers were computerised and discussed, and highest when handed over by handwritten notes (Fig 1).
Table 5.
Comparison of quality scores between auditor 1 and auditor 2 for handovers. Grouped by the quality scored by auditor 1.
Discussion
This evaluation shows that use of an electronic proforma for weekend patient handover together with discussion at a meeting is the best method for achieving an adequate quality handover, ensuring good continuity of care and improving patient safety. Handwritten undiscussed handovers as a group scored badly, however there was large variation in quality for handwritten handovers. A limitation of this evaluation is that many verbal and some handwritten handovers were likely never collected and added to the database for retrospective audit. Overall, the target of 95% of handovers being of adequate quality was not reached, although the group of handovers using the computerised proforma and discussed, approached this target.
Compared to other aspects of medicine, there is a relative paucity of evidence to guide effective patient handover.9 Bhabra et al have shown, using simulated patient handovers, that verbal-only handover leads to considerable loss of information compared to verbal handover with written notes.10 When information loss was analysed, important and less important information in patient handover were lost at a similar rate. Ferran et al studied the use of standardised proformas to improve patient handover, auditing information handover for trauma patients before and after the introduction of a proforma.11 Standardised proformas led to significantly less information loss, however, some information was still poorly handed over even with the proformas. Grainge et al have shown a standardised weekend handover form can improve documentation, for example of resuscitation decisions.12 Raptis et al looked at handover of patients to hospital at night teams before and after introduction of electronic handover.13 Prior to introduction, their hospital used verbal handover with entry onto a handwritten proforma. The handwritten proforma contained the same entry fields as their new electronic proforma. They compared completeness of information fields for the verbal-written handover method and the electronic handover method over the transition period. They found a significantly greater percentage of completed fields with electronic handover. However, field completion rates are a poor surrogate marker for quality of handover. Fields can be filled with unclear information. That is why, in this study, each handover entry was judged based on the actual content of the information fields. The Health Informatics Unit of the Royal College of Physicians (RCP) has used a questionnaire followed by a pilot study to develop an evidence base for the fields to use in handover proformas.14,15
Use of a proforma encourages entry of all the information necessary for reviewing the patient and displays this information in a structured manner that is easy to follow. However, a proforma does not stop unclear and unrealistic plans being handed over. A handover meeting provides a good opportunity to clarify any unclear handover entries and amend any unsuitable plans (for example plans to request investigations not available over the weekend). Handover meetings may require a significant amount of time on a Friday afternoon and so it is important that they are time efficient. Training may improve the quality of the meetings.16,17 Handover is more than just relaying patient details–it requires assessing what information might be needed by the on-call team without handing over excessive amounts of distracting information. It needs to be relayed in a structured and succinct manner. It gives the opportunity to explain the rationale for plans so that the on-call team can respond to any unanticipated events.18 Many patients at the weekend needed review of conditions particular to a medical
specialty with which a junior doctor on call may not be familiar–the meeting provides a valuable educational opportunity to discuss management of a diverse range of medical conditions. Given the importance of handover, the Academy of Medical Royal Colleges, the British Medical Association and the National Patient Safety Agency have published guidelines for safe medical handover.19,20 Handovers should be face-to-face with the involvement of senior clinicians and written or electronic proformas. Verbal discussion should highlight anticipated problems and clarify management plans. Patient handovers need to contain patient location, unique identifiers, responsible consultant, aims and limitations of treatment, outstanding tasks and the reasons for requested tasks. Recently the RCP has developed a toolkit and templates to help hospitals improve their handover arrangements.21
Although this study has shown that an electronic handover tool together with a dedicated handover meeting were favourable for handover quality compared to other methods, the proposed 95% target was not met. Changes have therefore been made:
further education should be provided to all clinicians on the importance of a dedicated handover meeting
principles of medical handover should be part of the induction programme for new doctors
a new electronic handover programme to allow patients to be handed over even after the handover meeting, should be introduced.
The last of these will improve handover by allowing information to be updated at any time as out-of-date information has been found to be a cause of poor handover.18 Additionally, many patients whose cases were handed over on handwritten notes and not discussed at the meeting were recognised as being unwell after the meeting.
Handover is an integral part of good medical practice. Healthcare professionals have been slow to recognise its importance. This is reflected by the very limited number of published studies evaluating the clinical effectiveness of handover models in acute hospitals. The results of our service evaluation have shown the importance of handover meetings and, locally, led to changes designed to improve our handover. We have now brought in structured handover meetings for all of our daily clinical handovers and will further evaluate these changes.
References
- 1.Jones GJ, Vanderpump MP, Easton M, et al. Achieving compliance with the European Working Time Directive in a large teaching hospital: a strategic approach. Clin Med 2004; 4: 427–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pounder R. Junior doctor's working hours: can 56 go into 48? Clin Med 2008; 8: 126–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zinn C. 14,000 preventable deaths in Australia. BMJ 1995; 310: 1487. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health. Organisation with a memory. Report of an expert group on learning from adverse events in the NHS 2000London: DH [Google Scholar]
- 5.McCann L, McHardy K, Child S. Passing the buck: clinical handovers at a tertiary hospital. N Z Med J 2007; 120: U2778. [PubMed] [Google Scholar]
- 6.Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. Consequences of inadequate sign-out for patient care. Arch Intern Med 2008; 168: 1755–60 10.1001/archinte.168.16.1755 [DOI] [PubMed] [Google Scholar]
- 7.Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 2005; 14: 401–7 10.1136/qshc.2005.015107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005; 37: 360–3 [PubMed] [Google Scholar]
- 9.Raduma-Tomas MA, Flin R, Yule S, Williams D. Doctors' handovers in hospitals: a literature review. BMJ Qual Saf 2011; 20: 128–33 [DOI] [PubMed] [Google Scholar]
- 10.Bhabra G, Mackeith S, Monteiro P, Pothier DD. An experimental comparison of handover methods. Ann R Coll Surg Engl 2007; 89: 298–300 10.1308/003588407X168352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferran NA, Metcalfe AJ, O'Doherty D. Standardised proformas improve patient handover: audit of trauma handover practice. Patient Saf Surg 2008; 2: 24. 10.1186/1754-9493-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grainge C, Traer E, Fulton J. Do weekend plan standard forms improve communication and influence quality of patient care. Postgrad Med J 2005; 81: 524–5 10.1136/pgmj.2004.030064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raptis DA, Fernandes C, Chua W, Boulos PB. Electronic software significantly improves quality of handover in a London teaching hospital. Health Informatics J 2009; 15: 191–8 10.1177/1460458209337431 [DOI] [PubMed] [Google Scholar]
- 14.Carpenter I, Bridgelal Ram M.Handover and discharge record content structure standards for hospital practice: consultation questionnaire report 2008London: Health Informatics Unit, Royal College of Physicians [Google Scholar]
- 15.Carpenter I, Bridgelal Ram M.Handover and discharge record content structure standards for hospital practice: pilot report 2008London: Health Informatics Unit, Royal College of Physicians [Google Scholar]
- 16.Lyons MN, Standley TDA, Gupta AK. Quality improvement of doctor's shift-change handover in neuro-critical care. Qual Saf Health Care 2010; 19: e62. [DOI] [PubMed] [Google Scholar]
- 17.Cleland JA, Ross S, Miller SC, Patey R. ‘There is a chain of Chinese whispers …’: empirical data support the call to formally teach handover to prequalification doctors. Qual Saf Health Care 2009; 18: 267–71 [DOI] [PubMed] [Google Scholar]
- 18.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (inhospital handover of care)–a prospective survey. Qual Saf Health Care 2008; 17: 6–10 [DOI] [PubMed] [Google Scholar]
- 19.Academy of Medical Royal Colleges. A clinican's guide to record standards–part 2 2008London: AoMRC [Google Scholar]
- 20.BMA Junior Doctors Committee, National Patient Safety Agency, NHS Modernisation Agency. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers 2005London: BMA [Google Scholar]
- 21.Royal College of Physicians. Acute care toolkit 1: handover 2011London: RCP; www.rcplondon.ac.uk/sites/default/files/acute-medicine-toolkit-may-2011.pdf [Google Scholar]