Abstract
Alcohol misuse is a common reason for hospital admission. While there is considerable evidence from other areas that provision of specialised alcohol services can reduce alcohol intake, there is currently less evidence for medical departments in an acute hospital setting. Nottingham hospitals initiated such a service in 2002–3 based around two nurse specialists who provided input to inpatients with alcohol-related physical disease and provided links to community-based services for alcohol misuse. This service assessed 3,632 patients over five years and has seen a reduction in hospital admissions, violent incidents against staff and primary care attendances. It is believed that this model of care is an effective means of intervening in people with alcohol-related problems.
Key Words: alcohol, hospitalisations, intervention, nurse
Background
An interim analytical report prepared by the Prime Minister's Strategy Unit estimated that between 15,000 and 22,000 deaths per year were in some way associated with alcohol misuse at a cost of £15 billion.1 Between 1987 and 1991, and between 1997 and 2001, cirrhosis mortality in men in Scotland rose by 104% and in England and Wales by 69%.2 The Department of Health has published recommendations for commissioning of alcohol services which focus on whole system approaches to identification and treatment of alcohol problems.3
Nottingham is fortunate in that its alcohol services are well developed with a day hospital focus and a range of available facilities. This service provides facilities accessed from primary care, where alcohol excess is well established to be a significant factor in increased levels of attendance.4 Provision of alcohol services in the emergency department has been shown to be effective but there are a substantial number of patients with serious alcohol-related illnesses who are repeated attendees at hospital medical services, usually presenting via medical assessment units.5 Many have potentially life threatening illnesses and consume substantial amounts of NHS resource. Alcohol excess is a major contributor in many violent incidents against NHS staff. Despite this potentially huge impact on services, there is little information on the effect of provision of alcohol specialists to try and address the needs of this patient group.
Traditionally, the management of alcohol problems has been divided between the psychiatric services, drug and alcohol teams or liaison psychiatry, and the acute hospital services. These services have worked independently of each other, with few formal links between them. A nurse-led alcohol liaison service based in the medical department of a large teaching hospital in an urban area was therefore introduced and evaluated.
Aims
This study aimed to determine the impact on primary and secondary care services of the introduction of a nurse-led assessment service linking to Nottingham Substance Misuse Service. Two registered nurses who were previously trained in the alcohol services underwent training in the recognition of physical disease related to alcohol. The service was established with the following aims:
to formally assess hospital inpatients who were identified by the general nursing or medical staff as having an alcohol problem (which could either be the cause of admission or unrelated to it) and to provide brief interventions in patients where this was appropriate
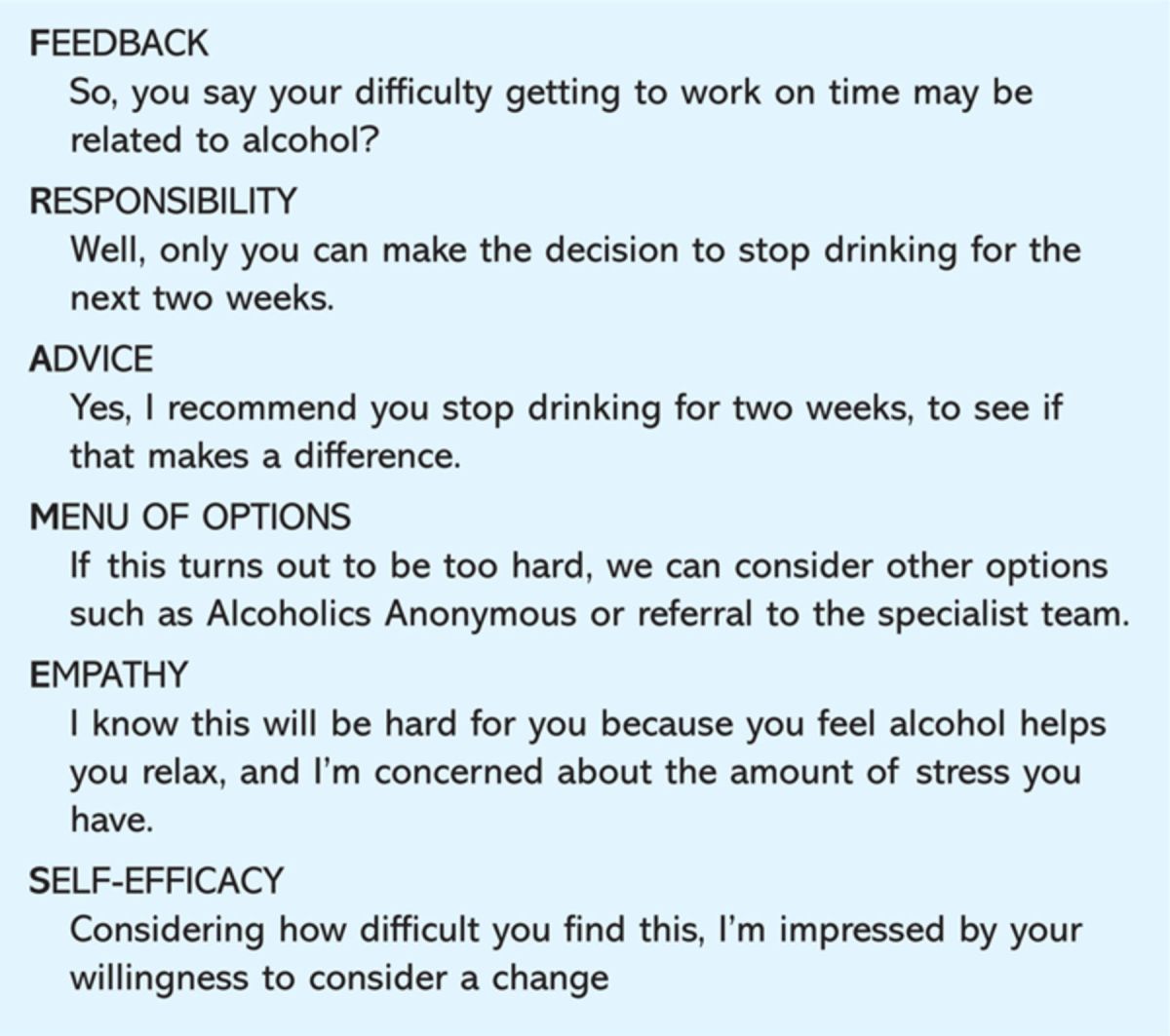
to provide ongoing follow-up for patients identified as having greater needs either by directly accessing community-based substance misuse services (SMS) or by follow-up to SMS protocols by the nurses in a hospital outpatient setting in a weekly clinic. The principles of the interventions used were based on the use of the AUDIT tool, brief advice for low dependency patients (score 8–15) using the FRAMES principles (Table 1) and extended brief advice for those with higher dependency scores (Appendix 1)6
to provide a clinic in the acute trust, run in parallel with physicians with an interest in liver disease allowing immediate assessment
to provide access to services for patients requiring detoxification from alcohol, either in the community or supervised detoxification on an outpatient basis on the acute hospital site
to develop protocols for the management of alcohol withdrawal and vitamin therapy for prevention of neurological damage and act as an advice resource for problems with detoxification occurring within the acute trust
to maintain links with SMS with a weekly clinic session based at a day hospital site and through this link to provide support to SMS in the assessment and diagnosis of physical disease in heavy drinkers within the SMS setting.
Table 1.
FRAMES counselling approach.16
Methods
The service was audited from its inception with details of referrals and source, AUDIT data, physical diagnosis and outcome. In addition, there were specific studies initiated to address specific patient populations.
Study 1
Admissions for alcohol detoxification were identified from the trust's clinical coding dataset on a three-monthly basis during introduction of the service.
Study 2
Forty patients with multiple admissions to Queens Medical Centre (QMC) with significant alcoholic liver disease and more than two admissions to hospital in the six months prior to introduction of the service were identified prospectively. Following intervention, admissions were recorded for the subsequent six months. Total bed days used and daily self-reported alcohol intake were recorded. An additional five patients identified as fitting the admission criteria were not included in this analysis as they died before the six-month follow-up period was completed.
Study 3
Self-reported alcohol intake was established in two groups of patients. One hundred consecutive patients admitted with an alcohol-related diagnosis prior to the introduction of the nurses were assessed by a consultant physician (SDR) and 100 patients with identical ICD diagnostic codes were seen by the liaison team. Intervention in the index group was limited to counselling by a consultant physician that alcohol was implicated in the hospitalisation, standard brief intervention information about consumption and provision of telephone information about outside agency contacts. Alcohol intake was recorded at the time of admission and by telephone follow-up six months and 12 months after the admission. Data were collected in units drunk in the week prior to the contact.
Study 4
Impact on primary care was established in a further group of consecutive patients identified by consultant physicians in the six months prior to introduction of the service as having a short (<48 hours) alcohol-related admission to hospital (n=20) given the same intervention described above. In the six months following this, the number of appointments made and attended was recorded by their general practitioner. An identical group, matched for primary diagnosis (n=20), was identified and seen by the alcohol liaison nurses in the first six months of the service and similar attendance data established from primary care records.
Study 5
Violence against staff in two clinical areas (the admissions unit and the gastroenterology ward at QMC) was established before the introduction of the service and six months after using the computerised incident reporting system which captures all clinical incidents at the trust (DATIX). This allows analysis of each individual incident and establishes the potential role of alcohol or alcohol withdrawal.
Results
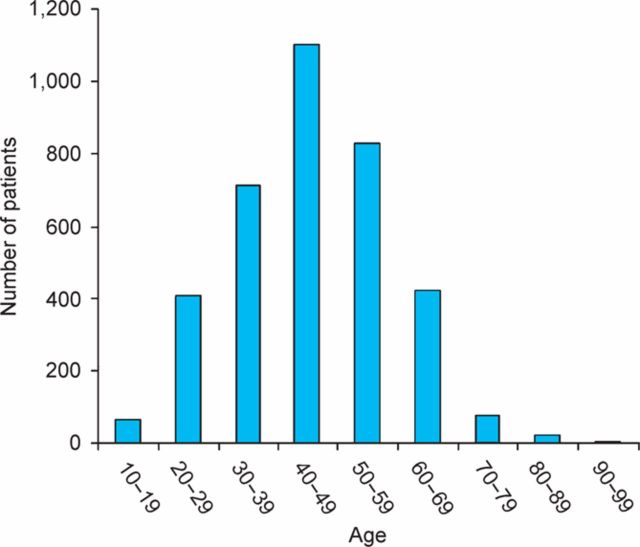
The service was introduced at QMC in April 2002. From April 2002 to March 2007, 3,632 new referrals from 55 different clinical areas were received (a mean of 61 patients per month). Seventy-eight per cent were male and 22% female, 93% were white, 3% Asian and 0.7% black. This is comparable to the East Midlands population as a whole in 2007, where 90.9% were white, 5% Asian, 1.5% black, 0.7% Chinese and 1.4% mixed race.7 Most patients were in the age range 30–59 years (Fig 1). Over the five years that the service has been in place, the proportion of women referred has increased (in 2003 16% females versus 27% in 2007).
Fig 1.
Age of patients referred to alcohol liaison nursing service.
Analysis of the referrals to the service shows that 18% were previously known to SMS, and only 3.9% of those admitted to QMC and assessed by the service were currently within one of the programmes of care run by SMS.
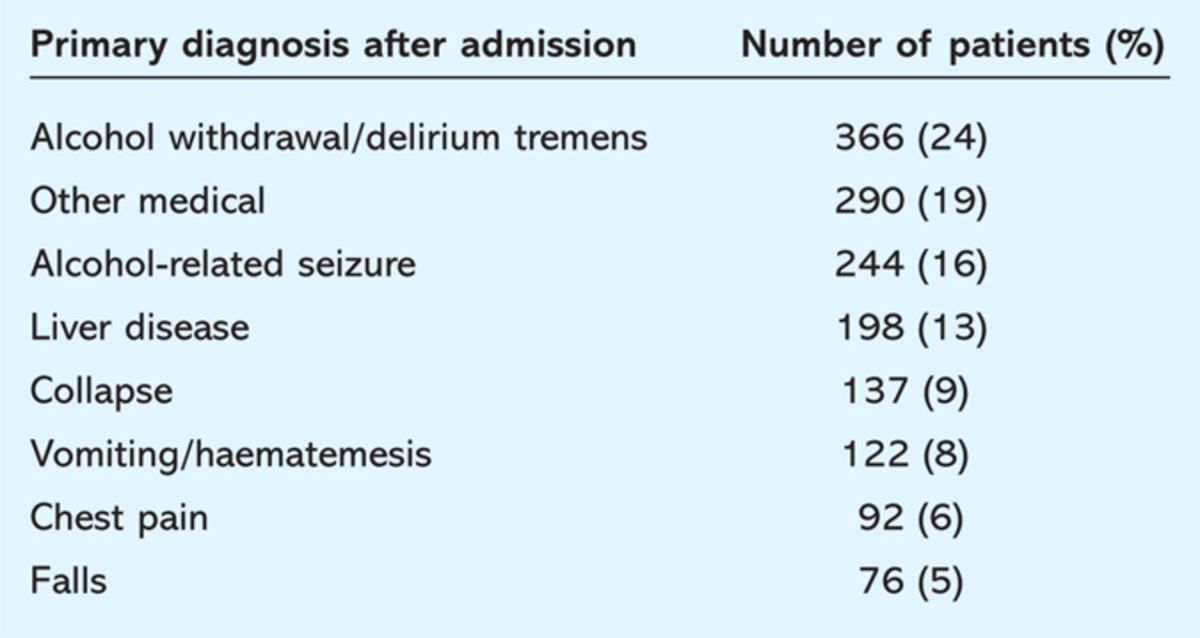
The average number of consultations with the alcohol liaison nurses was 2.5 during the admission. The main clinical areas using the service were the acute medicine unit and the short stay medical ward, together accounting for 42% of referrals. There was a wide range of reasons for admission to hospital in this group (Table 2) but it is of note that only 24% listed alcohol withdrawal as the primary reason. Over time, the proportion of patients with an obviously alcohol-related illness has fallen; in 2002, 75% of referrals had alcohol withdrawal, fits or liver disease compared to 43% in 2004. This change may suggest a greater awareness of alcohol as an issue in medical patients with diseases not directly related to alcohol excess as the service has developed.
Table 2.
Medical diagnosis in patients referred to the liaison nurses by the acute medicine unit or fast track medical ward.
One third of inpatient consultations were followed by liaison nurse clinic follow-up. Of 596 outpatient appointments offered overall from 2003 to 2006, 66% of patients attended. Attendance was more likely at the liver disease clinic (238/326, 73%) than at the extended brief intervention clinic (157/270, 58%) (p=0.0002). Ten per cent of patients were referred on to SMS services in the community.
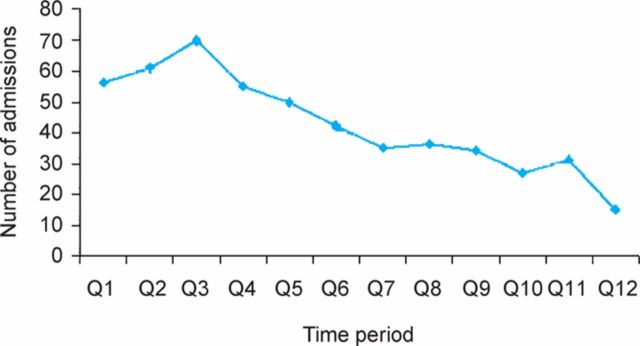
Study 1
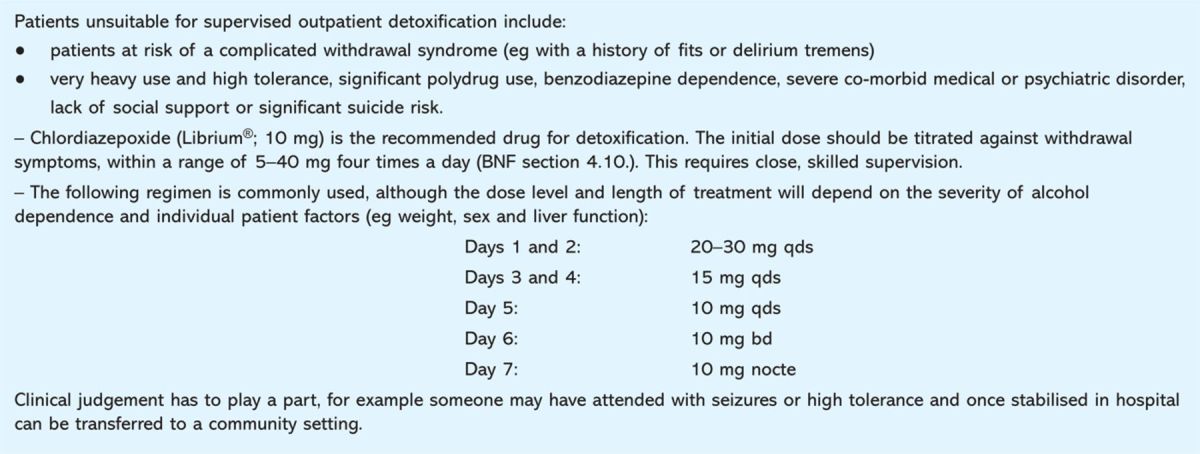
A decrease in numbers of patients admitted for alcohol detoxification was seen (Fig 2). The average hospital inpatient stay for alcohol detoxification was 4.2 days. This suggests that the number of bed days saved per month by the service was 36.4. Traditional inpatient detoxification was replaced in appropriate cases by supervised outpatient detoxification (Table 3). Patients had a median of three visits each. Attendance rate was 93% (for at least one appointment).
Fig 2.
Reduction of admissions for alcohol withdrawal. Q1 etc refer to three-month periods from 2002. Q1 represents January to March 2002 with sequential three-month periods thereafter. The alcohol liaison nurse posts were initiated in April 2002 (in Q2)
Table 3.
Patients who are unsuitable for supervised outpatient detoxification from alcohol and the regimen used.17.
Study 2
In the 40 cirrhotic patients (32 male, 8 female, mean age 51 years) (Child–Pugh score median 6, range 3–12) a high level of alcohol dependency was present (mean AUDIT score 32, range 17–40). Bed days used in the six months post-intervention fell from 6.3 per month to 3.2 per month. Fifty-one per cent had fewer bed days after intervention and there was a significant relationship with reduction in self-reported alcohol intake, overall this fell from 8.4 units (mean +/− SEM) per day to 4.6 units per day after intervention and in the group with fewer bed days there was a greater reduction (1.7 units per day).
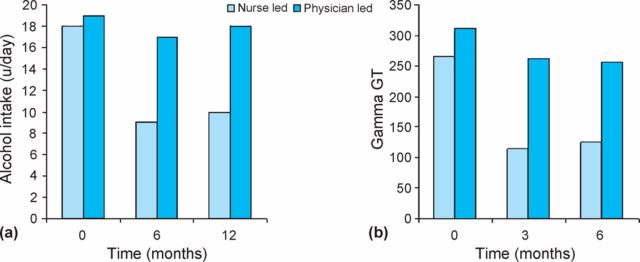
Study 3
The two cohorts showed no substantial differences in alcohol-related disease codes or levels of alcohol dependence as assessed by AUDIT (Table 4). A comparison of physician counselling versus nurse input showed that self-reported alcohol intake showed a greater decline in patients accessing the alcohol liaison nurses. In the group with no specialist intervention, baseline intake was 19 units per day (range 6 to 67), at six months this was 17 (range 0 to 78) and at one year 18 units/day (range 0 to 66). In the cohort who had not had any intervention from the alcohol liaison nurses alcohol intake at baseline was 18 units (range 11–68), at six months nine units (range 0–49) and at one year 10 units (range 0–44) (p=0.001 at one year)(Fig 3). The reduction in alcohol intake was corroborated by falls in gamma-glutamyl transferase (GGT) levels, in the nurse-managed cohort GGT levels fell by a mean of 53% at a three month follow-up point and by 57% at six months versus 16% and 18% for physician counselling.
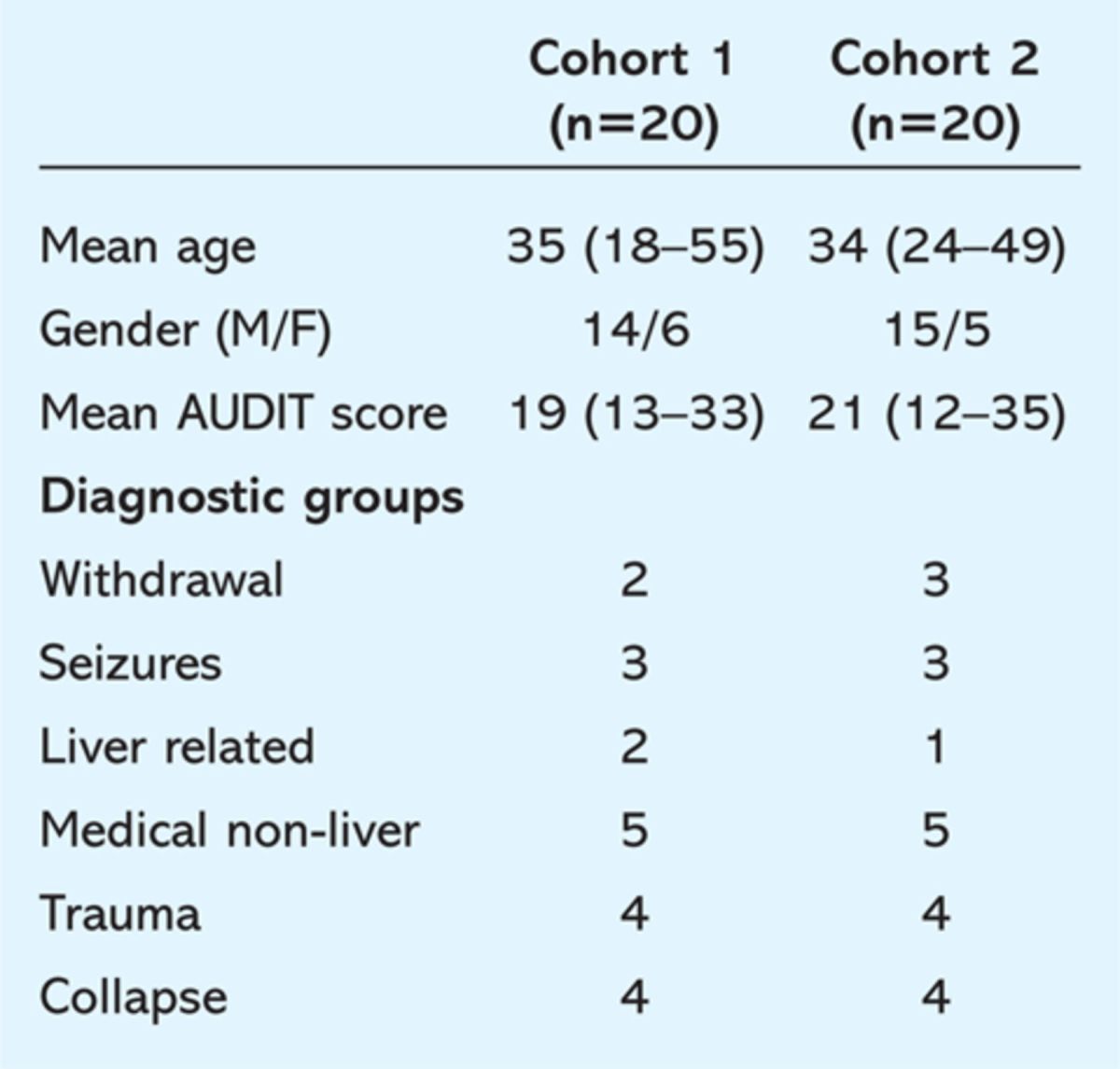
Table 4.
Demographics and AUDIT scores in two cohorts of patients with alcohol-related hospital admissions who received interventions.
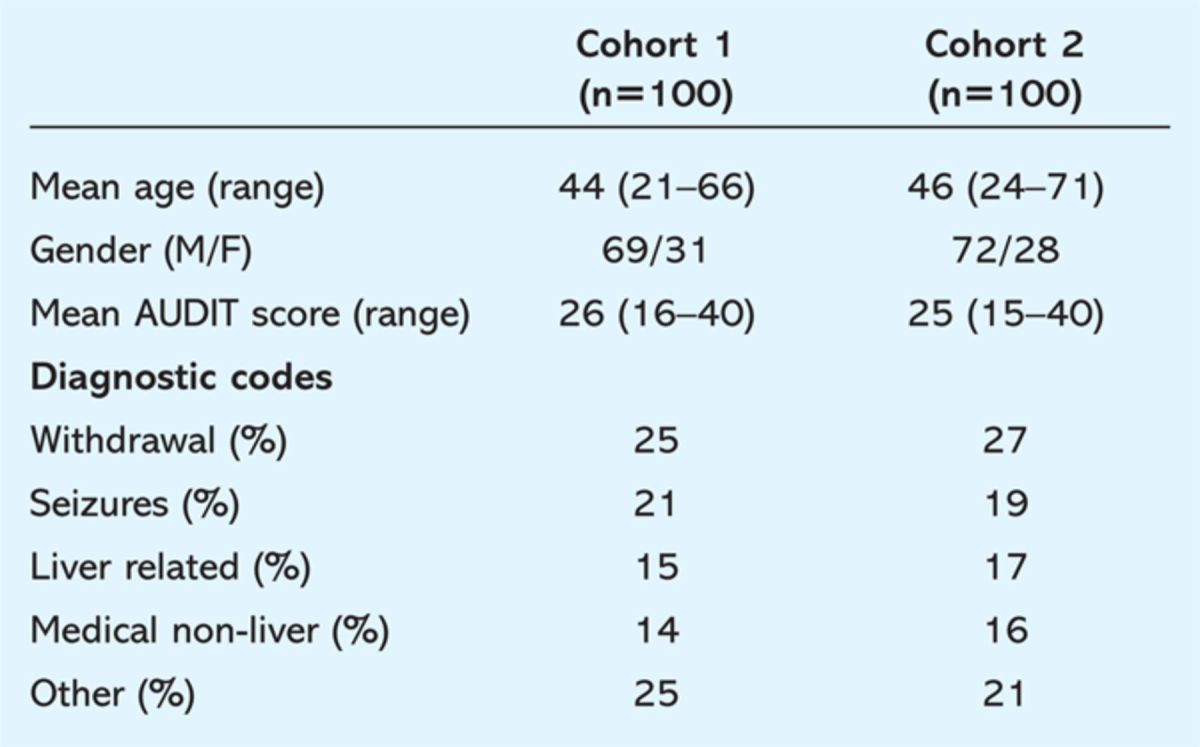
Fig 3.
(a) Self-reported daily alcohol intake in two cohorts (n=100) with either physician- of nurse-led intervention. (b) Gamma glutamyl transpeptidase levels in the two cohorts with either physician- or nurse-led intervention.
Study 4
Demographics are shown in Table 5. Primary care attendances were lower in the group seeing the nurse team, a mean 3.7 attendances in six months, than those seeing a consultant physician only, mean 8.1.
Table 5.
Demographics and AUDIT scores in patients attending primary care after an alcohol-related hospital admission. Cohort 1 physician only intervention, cohort 2 nurse intervention.
Study 5
Violent incidents where alcohol was a significant factor against staff fell following the introduction of the service. In the six months prior to its onset there were 1.7 incidents per week overall on the two wards, this fell to 0.45 per week in the second six months of the service. Analysis of the incidents suggested that most of this fall was related to better management of withdrawal from alcohol on the admissions unit.
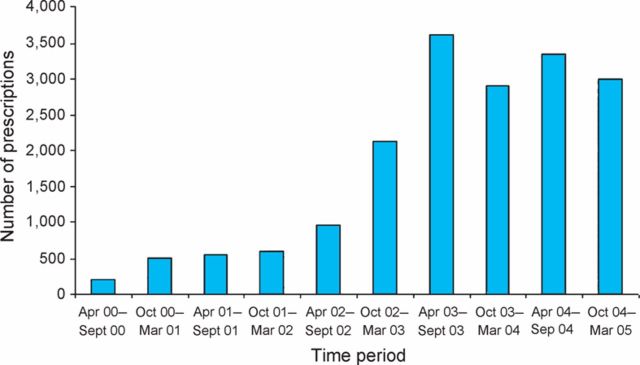
Additional physical disease was detected by the alcohol liaison team (hepatitis C in 25 patients and hepatitis B in four patients). Prescribing of intravenous B vitamins increased over time following introduction of the liaison team (Fig 4). This followed the introduction of a formal policy by the alcohol liaison team and regular updates and monitoring of implementation.
Fig 4.
Prescribing of intravenous B vitamins to inpatients at Queens Medical Centre.
Discussion
Alcohol is the direct cause of 10% of all hospital admissions and is implicated in an even larger proportion.8 This population has traditionally been regarded as a difficult one to access for alcohol support services. Provision of appropriate support and counselling in the accident and emergency setting or in primary care can reduce alcohol intake by approximately 30% and if hospital inpatients are screened for excess alcohol use then brief interventions are effective in reducing alcohol intake.5,9 Brief interventions have been shown to be effective in primary care in patients of all ages although all these populations showed relatively low levels of alcohol dependence.10,11
The populations of patients encountered by hospital medical and particularly hepatology teams, however, are likely to have established physical disease with long drinking histories. Despite this, previous evidence has suggested that patients with alcohol-related liver disease may have a lower level of dependence than those attending alcohol services.12 This was not evident in this study with high levels of dependency seen in the cohort of repeated attendees to hospital with cirrhosis, perhaps reflecting a different population from the Southampton study where most patients were surveyed at their first presentation with liver disease. Brief interventions in this population have not been extensively studied and there is still debate about the role of brief or extended brief intervention in the treatment of highly dependent drinkers. In a large US study of pharmacological and behavioural interventions in a population with high levels of dependency, a programme of behavioural interventions combined with placebo pills produced a similar significant decrease in alcohol intake than pharmacological intervention.13 In the current study, interventions in this group were based on an extended series of interventions and seem to show that reductions in alcohol intake and, perhaps more importantly, hospital admissions as a result of physical disease can be impacted by such interventions. It is important to stress, however, that provision of a relatively small service has limited impact. The data for overall hospital admissions for alcohol-related disorders in Nottingham City primary care trust (PCT) rose by 9% from 2007/8 to 2008/9 (1,778 to 1,944).14 Nottinghamshire County PCT, by contrast, showed a fall of 8% (1,350 in 2007/8 to 1,230 in 2008/9). City PCT is the main referrer to the acute trust and has a high level of deprivation emphasising the need for community wide actions to tackle the increase in alcohol-related disease.
The links between SMS and the acute trust seem important, 10% of patients identified by the team went to SMS services in the community and a further 33% were engaged in SMS activity taking place in an acute hospital outpatient setting. There were a number of reasons for the choice which were not systematically studied here, patients with serious physical disease could be seen in the same location for both medical and alcohol intervention, some patients did not wish to access community services as they had already built a relationship with the nursing team during their inpatient stay and preferred follow-up with that person.
These data suggest that provision of expert assessment for medical inpatients has a considerable impact. Uptake is good with education of medical and nursing staff allowing identification of patients at risk where evidence-based brief interventions can be given.
In the specific groups where more detailed data were obtained, evidence has been provided that intervention by trained staff in a highly alcohol dependent group with serious physical disease has a substantial impact on alcohol intake and can reduce hospital admissions and bed stays. Reduction in admissions to hospital and reduced bed days occupied for detoxification would save as similar sized trust approximately 550 bed days per year. The reduction in readmissions for patients with significant liver disease is potentially even greater as they have an average length of stay considerably in excess of the average and have a high utilisation of medical resources. While the experience of this study cannot directly quantify such benefits it is clear that the potential is considerable.
A significant proportion of violent incidents in hospitals have alcohol as a substantial factor. Data suggest that provision of alcohol withdrawal information and protocols do have an impact on such incidents to the obvious benefit of patients and staff. The increase in prescribing of B vitamins is a strategy well established to reduce the risk of neurological catastrophe in heavy drinkers and therefore is likely to be highly beneficial both to the individuals concerned and to all providers of healthcare.15
The positive impact is not confined to secondary care. Heavy drinkers are heavy consumers of all forms of healthcare and attend in primary care up to four times more frequently than other groups.4 Provision of the nurse-led service can have a significant impact on primary care attendance, and this study is the first hospital-based intervention of this type to show such an effect. The major risk of this service's introduction has been that it has identified a group of people drinking at risk and often with significant physical disease who were not previously known to the drug and alcohol services. This has had a substantial impact in terms of new referrals to SMS.
There are a number of specific factors which have been essential for the success of this service and therefore may not be applicable to other hospitals. Nottingham has a well developed day hospital-based alcohol service which can provide for the differing needs of large numbers of people with alcohol problems. This ranges from key worker assessment and follow up through a range of alcohol harm reduction programmes through to inpatient facilities for detoxification. The availability of resources outside the acute trust setting was vital in two regards, an existing structure into which clients could be referred and managed but also the presence of interested and expert staff in Nottingham alcohol team who could support the liaison service. A further vital factor in the success of the service was that all the key individuals shared a common view of the nature of problem drinking. The team does not believe that the disease-based nature of habitual drunkenness is summed up by the term ‘alcoholic’. Instead, drinking is considered fundamentally a behaviour over which individuals exercise choice and services are configured to reflect this with, for example, controlled drinking programmes available for those without serious medical consequences where abstinence is less vital. If such commonality of view was not present within the team this could lead to considerable conflict in both direction and delivery of service.
Although there are wide variations across the UK in availability and potential to access alcohol services and therefore local needs will vary, this type of secondary care interface service is likely to be cost effective. The initiation of this service has relied on close collaboration between all the healthcare organisations involved and funding via a partnership with contributions from the acute and community healthcare trusts is acknowledged.
Acknowledgement
The authors are grateful to Lynn Wynstanley (then director at Nottingham Health Authority) who initially commissioned this service.
References
- 1.Prime Minister's Strategy Unit Interim analytical report. London: Prime Minister's Strategy Unit, 2003. [Google Scholar]
- 2.Leon DA, McCambridge J. Liver cirrhosis mortality rates in Britain from 1950 to 2002: an analysis of routine data. Lancet 2006;367:52–7. 10.1016/S0140-6736(06)67924-5 [DOI] [PubMed] [Google Scholar]
- 3.National Treatment Agency for Drug Misuse Models of care for alcohol misusers (MoCAM). London: National Treatment Agency for Drug Misuse, 2006. [Google Scholar]
- 4.Little P, Somerville J, Williamson I, et al. Psychosocial, lifestyle, and health status variables in predicting high attendance among adults. Br J Gen Pract 2001;51:987–94. [PMC free article] [PubMed] [Google Scholar]
- 5.Crawford MJ, Patton R, Touquet R, et al. Screening and referral for brief intervention of alcohol-misusing patients in an emergency department: a pragmatic randomised controlled trial. Lancet 2004;364:1334–9. 10.1016/S0140-6736(04)17190-0 [DOI] [PubMed] [Google Scholar]
- 6.Saunders J, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption. Addiction 1993;88:791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- 7. UK National Statistics, www.statistics.gov.uk.
- 8.Royal College of Physicians Alcohol: can the NHS afford it?. London: RCP, 2001. [Google Scholar]
- 9.Holloway AS, Watson HE, Arthur AJ, et al. The effect of brief interventions on alcohol consumption among heavy drinkers in a general hospital setting. Addiction 2007;102:1762–70. 10.1111/j.1360-0443.2007.01968.x [DOI] [PubMed] [Google Scholar]
- 10.Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst Rev 2007;18(2):CD004148. 10.1002/14651858.CD004148.pub3 [DOI] [PubMed] [Google Scholar]
- 11.Fleming MF, Manwell LB, Barry KL. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract 1999;48:378–84. [PubMed] [Google Scholar]
- 12.Smith S, White J, Nelson C, et al. Severe alcohol-induced liver disease and the alcohol dependence syndrome. Alcohol Alcohol 2006;41:274–7. 10.1093/alcalc/agl014 [DOI] [PubMed] [Google Scholar]
- 13.Anton RF, O'Malley SS, Ciraulo DA, et al. Combined pharmacotherapies and behavioural interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 2006;295:2003–17. 10.1001/jama.295.17.2003 [DOI] [PubMed] [Google Scholar]
- 14. Local alcohol profiles for England, www.nwph.net/alcohol/lape/download.htm.
- 15.Cook CHC, Hallwood PM, Thomson AD. B Vitamin deficiency and Neuropsychiatric syndromes in alcohol misuse. Alcohol Alcohol 1998;33:317–36. 10.1093/oxfordjournals.alcalc.a008400 [DOI] [PubMed] [Google Scholar]
- 16.Miller WR, Sanchez VC. Motivating young adults for treatment and lifestyle change. In: Howard G, Issues in alcohol use and misuse by young adults. Notre Dame, Indiana: University of Notre Dame Press, 1993:55–82. [Google Scholar]
- 17. World Health Authority, www.whoguidemhpcuk.org/page_view.asp?c=16&did=1845&fc=005015.