Abstract
Lyme disease is rare in the UK but there is evidence of an increase in both prevalence of, and patient concern about, the infection. There are no published data characterising Lyme disease as it is seen in the UK. The clinical and laboratory features of 65 patients diagnosed with the disease between 2002 and 2007 were recorded and their clinical presentation and response to treatment documented. In total, 34% of patients acquired the infection in the UK, 20% in North America and 46% in Europe. Exposure to ticks was reported by 58% of patients. Erythema migrans was seen in 91%, systemic upset in 62%, headaches in 31%, arthralgia or arthritis in 28%, radiculitis in 11% and cranial nerve palsies in 4.6%. Screening enzyme immunoassay tests were negative in 39% and reference laboratory immunoblots were negative in 31% of patients, principally those with early infection. The majority of patients were cured with one course of antibiotic treatment, three patients had evidence of persistent infection after treatment and two required intravenous therapy. No cases of chronic Lyme disease were seen.
Key Words: Borrelia burgdorferi, clinical features, laboratory features, Lyme disease
Introduction
Lyme disease is an infectious disease which can affect several body systems. It is caused by the spirochaete Borrelia burgdorferi which is transmitted by hard ticks of the Ixodes ricinus complex. Its clinical manifestations include skin lesions, neurological abnormalities, musculoskeletal symptoms, cardiac dysrhythmias and systemic upset.1 Patients with the infection may therefore present with varying clinical features to doctors of a range of specialties at various times after infection has occurred.
Lyme disease has a fairly low incidence in the UK. The annual reported incidence of laboratory-confirmed cases in England and Wales increased from around 270 cases between 1997 and 2000 to 797 in 2006.2 Rising reported incidence in the UK may relate in part to increasing awareness of the condition and to changes in laboratory tests and surveillance methods over the 10-year period. Additionally there is some evidence for an increase in recreationally-acquired infections, through activities in the UK and abroad. Tick populations appear to have increased in some parts of the country, possibly related to increased deer numbers and changes in land management.
In the UK presently recognised Lyme disease-endemic areas include the New Forest, other southern wooded and heathland areas, Exmoor, Dartmoor, Thetford Forest, the Lake District and the Scottish Highlands and Islands.3 It is less frequently seen outside these areas. Lack of familiarity by doctors with the infection may lead to delay in diagnosis and treatment. The Hospital for Tropical Diseases, London, has seen increasing numbers of patients presenting with, or referred for, assessment of possible Lyme disease over recent years. This is reflected in increasing numbers of Lyme serology tests requested; 229 samples in 2005 and 432 in 2007. The proportion of positive tests, around 7%, has not changed significantly over that period. Factors such as increasing travel and leisure time exposure in rural areas in Europe and North America as well as the UK, and increased public awareness of Lyme disease may have contributed to the increase in referrals.
There is significant and increasing public concern about Lyme disease and this may be propagated by the large number of Lyme disease websites, many of which contain alarming and inaccurate misinformation about the clinical features, treatment and prognosis of the disease.4,9
Our clinical experience of Lyme disease has been reviewed and an analysis of the clinical and epidemiological details of the patients seen in an urban hospital setting is presented. Such studies are available from Europe and the USA,7,8 and a recently published study sets out clinical features encountered with Lyme disease in an endemic focus in the south west of England.5 However, it is known that the clinical presentations of the disease can vary in different areas due, in part, to the various genospecies of B. burgdorferi sensu lato which may cause different clinical syndromes.1 The clinical studies of Lyme disease from the UK are generally from endemic areas and based only on patients with positive antibody tests.5 The patients in this study presented a more varied range of clinical features, often with presentation early in the course of infection when antibody testing is negative and can remain negative after effective treatment.
Methods
This study took place in an infectious diseases service of a London teaching hospital, which accepts referrals from general practitioners and hospital clinicians. Patients are seen at booked clinic appointments. Patients who present without referral are also seen at a walk-in clinic. The Hospital for Tropical Diseases clinical database, which records patients' final and working diagnoses, was used. Patients from the six-year period from January 2002 until the end of 2007 who had a final diagnosis of Lyme disease were included and their notes reviewed. A case definition which is based on the guidelines of the Infectious Diseases Society of America (IDSA) was used.6 To fulfil this, patients had to have either:
erythema migrans (EM), an expanding, red, flat, roughly circular lesion which was more than 5 cm in diameter, without features of cellulitis (hotness, tenderness, swelling and induration), with or without central clearing and which appeared more than three days after exposure to a tick in, or travel in, an area considered endemic for Lyme disease and considered by a physician experienced in infectious diseases to be erythema migrans
clinical features consistent with Lyme disease (which could include EM, though this was not a prerequisite), an appropriate exposure history and positive Lyme serology reported by the reference laboratory as being consistent with infection with B. burgdorferi after using standardised, two-stage, serological testing.6
Importantly, to meet our case definition, patients with EM did not have to have positive Lyme serology if they had definite EM as EM is seen early in the course of infection, when serological tests are often negative. Prompt and early antibiotic treatment may prevent an antibody response from developing.
Twelve cases which did not fit the case definition were excluded from the analysis as there was no EM and a negative lyme serology, and therefore no objective evidence of Lyme disease was found in these patients.
Case records were reviewed to identify the location where infection was acquired and whether patients had seen ticks on their skin. The possible duration of tick attachment was noted, when available from the record. The interval between exposure to ticks and the development of symptoms or signs was determined and, where no tick was seen, the time between their leaving the endemic area and the date of development of symptoms was recorded to give a minimum incubation period. Clinical features noted at history taking and physical examination and the results of electrocardiograms, where these were performed, were also registered.
Local screening for antibodies to B. burgdorferi was carried out using a combined IgM + IgG enzyme-linked immunosorbent assay (ELISA) and results were noted together with reference laboratory serology results for those whose tests were positive or equivocal. Where a piece of information was missing from the medical records, patients were contacted (necessary in five cases). Details of antibiotics prescribed, including dose and duration, were obtained from the clinical record, together with observations on the patient's response and results of repeat antibody testing after treatment.
Results
In total, 77 patients with a diagnosis of Lyme disease were identified from the patient database over the six-year period. Of these, 65 met the case definition. The clinical details of these are set out below. The other 12 patients were excluded from the case series as noted above.
Likely site of acquiring infection
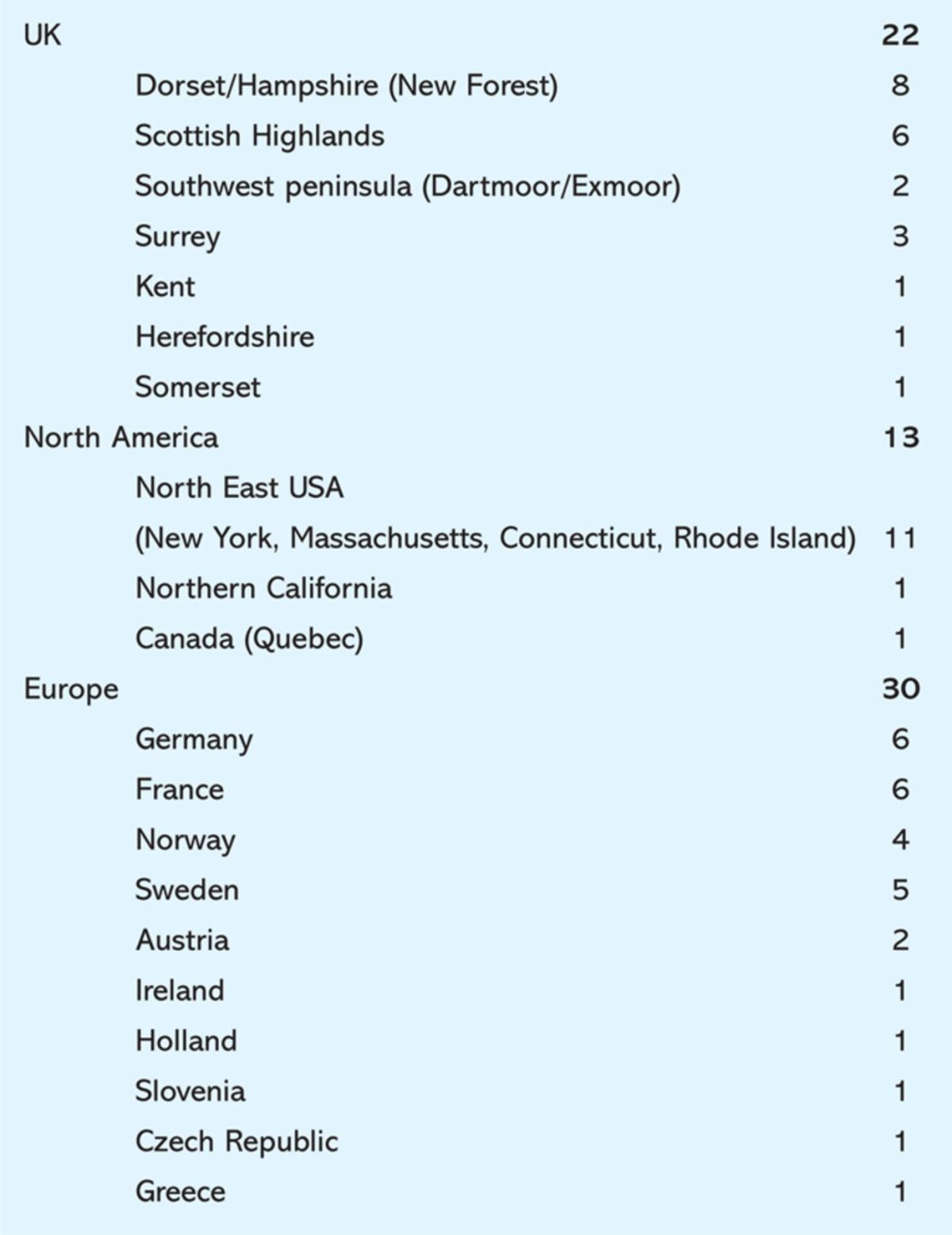
The geography of infections is detailed in Table 1. Overall, 34% of patients acquired the infection in the UK, 20% in North America and 46% in Europe.
Table 1.
Geography of probable sites of acquisition of Lyme disease of patients presenting to the Hospital for Tropical Diseases.
Sex and age
The mean age was 43.2 years (range 20 to 80) and with equal numbers of male and female patients.
Tick bites
Of the 65 patients, 38 (58%) had seen ticks attached to their skin with 14 able to estimate the duration of attachment; six (9.2%) thought that the tick had been attached for more than three days. Only one patient with Lyme disease presented a tick to us for identification. This was identified as Ixodes sp.
Incubation period
The mean time between exposure to ticks and development of symptoms was 21 days (range 3–82).
Clinical features
Erythema migrans. Of the 65 patients, 59 (91%) had EM at presentation, described EM or showed a photograph of a rash consistent with EM. Among those who did not require EM for diagnosis, that is those who had positive serology, appropriate symptoms and exposure, 41 out of 47 patients (87%) had EM. Six patients did not have EM, and five of these had neurological symptoms other than headache alone.
Headaches and meningism. Twenty patients (31%) had a headache, which in eight cases had no meningitic or other neurological features. Headache was associated with neck stiffness in four cases, with photophobia in four cases, and with both neck stiffness and photophobia in four.
Cranial nerve palsies. Three patients (4.6%) had cranial nerve palsies. Two had isolated palsies of the facial nerve and one had a combined palsy of the facial, abducens and vestibulocochlear nerves plus radiculitis, lymphocytic meningitis and ankle swelling. All three of these patients had acquired their infection in North America.
Nerve root and peripheral nerve disturbances. Seven patients (11%) had an area of numbness or paraesthesia or pain in a dermatomal distribution. One patient had an area of numbness and intermittent pain in the distribution of a peripheral nerve, the lateral cutaneous nerve of the thigh. Two patients noted visual blurring and two dizziness.
Systemic symptoms. Forty patients reported systemic upset (62%) with 20 reporting fevers and sweats, 27 experienced lethargy, tiredness or malaise, four experienced nausea and anorexia, one experienced a sore throat and one lymphadenopathy.
Musculoskeletal symptoms. Thirty-three patients (51%) experienced musculoskeletal symptoms. There were four patients with arthritis. They had acquired their infections in the New Forest, North America, Sweden and the Isle of Jura. Knee and ankle joints were affected. Fourteen patients had arthralgia without swelling or tenderness of the affected joints and 18 experienced myalgias.
Cardiac symptoms. Only five patients (7.7%) reported cardiac symptoms – all of them reported palpitations. In only one case was there an abnormality in the resting electrocardiogram (ECG), which showed first degree heart block. The remaining four patients had normal ECGs.
Treatment
Treatment was started on the basis of clinical features in 52 patients, of whom 51 had EM. Treatment included:
doxycycline in 50 patients, at a dose of 200 mg per day for 14–21 days
amoxicillin in one patient, 500 mg three times a day for 21 days
amoxicillin-clavulanic acid in one patient, 625 mg three times a day for 21 days.
Treatment was deferred until the results of serological tests were obtained in 13 patients. Seven of these had EM. Nine were treated with doxycycline at a dose of 200 mg a day for 14–21 days. Four patients with neurological features, either cranial nerve palsy or radiculitis, were treated with ceftriaxone 2 g intravenously daily for 21 days.
Treatment failures
Three (4.6%) patients had either no resolution or a worsening of their symptoms at follow-up six to eight weeks after treatment. In all three cases more strongly positive antibody responses on repeat testing confirmed primary treatment failure. All three patients had previously received an initial 21-day course of doxycycline. All were given a further 21-day course, to which one responded. The other two patients had continuing symptoms and evolving antibody tests and were treated with a 21-day course of intravenous (iv) ceftriaxone, to which they responded.
No cases in which Lyme disease was refractory to iv antibiotic treatment were recorded. No cases had residual features compatible with the disputed entity described as chronic Lyme disease.
Antibody tests
Testing for the presence of B. burgdorferi antibodies used an ELISA (enzyme-linked immunosorbent assay) that detects IgG and IgM antibodies. The results of this test were available within one day in 70% of cases and within three days in 88% of cases. The total number of tests that were positive in the last three years was 78. As the laboratory serves a number of different hospitals and many patients were tested more than once, this case series includes the majority of patients with a positive Lyme antibody test.
Positive and equivocal samples on the immunoassay were sent to the Lyme Borreliosis Diagnostic Unit of the Health Protection Agency at Southampton, where immunoblots are performed to assess reactivity to a range of B. burgdorferi antigens.
In this cohort, Lyme antibodies were tested for in 64 out of 65 patients with the screening ELISA; this was positive in 28 and equivocal in eight. Immunoblots on both the ELISA positive and equivocal samples were all positive at the reference laboratory. ELISA was negative in 25 patients. Eleven ELISA negative blood samples from patients thought to have the infection clinically were sent to the reference laboratory at the specific request of the responsible clinician, and six of these had positive immunoblots. Overall 44 out of 64 patients had Lyme disease serologically confirmed on immunoblot.
In 24 patients, serum was tested for Lyme antibodies at a follow-up clinic visit usually six to eight weeks after the initial appointment. In one patient, Lyme antibodies were negative, having been positive initially while in 18 patients the strength of antibody responses declined following treatment. In three patients, antibody responses were unchanged or were stronger and this was taken to indicate treatment failure as noted above.
Discussion
The studied patients largely had typical clinical features – 91% of patients had EM and those who did not often had characteristic neurological abnormalities. The diagnosis should therefore have been straightforward in most cases.
Apart from EM, the main symptoms were systemic upset in 62% of cases, arthralgia/myalgia in 51%, neurological symptoms other than a simple headache in 28% and cranial nerve palsy in 5%.
The clinical features differed from other studies from the UK and Europe. This was expected as a clinical, rather than a serological, definition of infection was used. In a study of patients from the UK based on positive serological tests, Lovett et al saw EM in only 65% of cases, arthralgia or myalgia in 27%, neurological features other than a simple headache in 25% of cases and cranial nerve palsies in 7%.5 In a study from 15 European countries including 3,317 cases, based on questionnaires sent to physicians, Cimmino saw EM in 60% of cases, neurological involvement in 34% and joint symptoms in 15%.8 Cardiac conduction abnormalities were rare, which is in keeping with findings reported in Cimmino's study where electrocardiographic abnormalities were present in only 2% of patients.8
Patients had acquired their infection in a wide range of geographical locations reflecting the known areas of Lyme disease endemnicity. Most of those infected in the UK had been to recognised endemic areas in the south west of England, the New Forest area and the Scottish Highlands. The occurrence of occasional cases elsewhere including Herefordshire, Surrey and Kent indicates that with time knowledge of the range of endemic areas in the UK may expand. Other European countries were the source of infection in almost half of the studied cases, with northern Europe and Scandinavia especially prominent. One case occurred in a man who visited Greece hinting at the need to consider Lyme disease among visitors to the countries of southern Europe. Just under a quarter of cases acquired the infection in the USA with the north-eastern seaboard prominent. Cases in visitors to Slovakia and the Czech Republic stress the importance of Lyme borreliosis in Eastern Europe.
Tick exposure was recalled by only 58% of patients. Lovett et al noted that tick exposure was only recalled by 64% of patients. The estimated duration of attachment was not helpful for diagnosis.
The majority of patients were cured with a standard course of oral antibiotics. In the few cases where treatment failures did occur, this was supported by serological tests and patients responded to second line treatment.
Lyme disease, as it presents in the UK, is relatively straightforward to diagnose although it is important to be aware of the range of endemic areas. Awareness of EM as a presenting feature is particularly valuable, whether it is seen on the patient or illustrated by them using digital photography. Treatment with oral antibiotics is effective in the majority of patients with infrequent need for iv ceftriaxone. Laboratory serology is used to support clinical suspicion. Cases of treatment failure are rare and can be confirmed by serological tests at a reference laboratory. Chronic Lyme disease (implying persistent active infection despite appropriate antibiotic treatment), a condition that causes much consternation to some patients, the existence of which is doubted, was not seen in any of the 64 patients.9,10
References
- 1.Steere AC. Lyme disease. New Eng J Med 2001;345:115–25. [DOI] [PubMed] [Google Scholar]
- 2.Health Protection Agency Epidemiology of Lyme borreliosis. www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/LymeDisease/EpidemiologicalData/lymEpidemiology/ [Google Scholar]
- 3.Health Protection Agency Lyme borreliosis in England and Wales: 2008. www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1195733837876 [Google Scholar]
- 4.Cooper JD, Feder HM., Jr. Inaccurate information about lyme disease on the internet. Pediatr Infect Dis J 2004;23:1105–08. [PubMed] [Google Scholar]
- 5.Lovett JK, Evans H, O'Connell S, Gutowski NJ. Neuroborreliosis in the South West of England. Epidemiol Infect 2008;136:1–5. 10.1017/S0950268808000472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wormser GP, Dattwyler RJ, Shapiro ED, et al. The clinical assessment, treatment, and prevention of lyme disease, human Granulocytic Anaplasmosis, and Babesiosis. Clin Infect Dis 2006;43:1089–134. 10.1086/508667 [DOI] [PubMed] [Google Scholar]
- 7.Tibbles CD, Edlow JA. Does this patient have erythema migrans. JAMA 2007;298:1159–60. 10.1001/jama.297.23.2617 [DOI] [PubMed] [Google Scholar]
- 8.Cimmino MA. Relative frequency of lyme borreliosis and its clinical manifestations on Europe. Infection 1998;26:298–300. 10.1007/BF02962251 [DOI] [PubMed] [Google Scholar]
- 9.Poison Plum www.poisonplum.com. [Google Scholar]
- 10.Feder HM, Jr, Johnson BJB, Jr, O'Connell S, et al. A critical appraisal of ‘chronic Lyme disease’. N Engl J Med 2007;3571422. [DOI] [PubMed] [Google Scholar]


