Background
Early recognition and treatment of sepsis is well recognised to reduce morbidity and mortality. Appropriate intervention with antibiotic agents and the potential involvement of intensive care specialists are key management elements.1–3
Aims
The aims of this study were to ascertain:
the level of knowledge among foundation year 1 (FY1) doctors of the criteria for diagnosing systemic inflammatory response syndrome (SIRS), sepsis and severe sepsis, as well as their knowledge of basic initial management of septic patients
whether a targeted brief intervention using an attachable laminated data card could improve FY1 knowledge.
Methodology
A standardised questionnaire was completed by 26 FY1 doctors at the Royal Berkshire Hospitals NHS Trust prior to one of their mandatory teaching sessions. The questioned topics included:
which four parameters constitute the SIRS criteria
what the abnormal values actually are
which other organ systems are involved in severe sepsis
how to investigate for a source of sepsis
initial management steps of sepsis, including time to first antibiotic dose.
The questionnaire was repeated after the doctors had received a sepsis guideline data card that could be clipped to their lanyard or name badge.
Outcomes
There was a 100% response rate. Prior to giving out the cards only seven of the 26 doctors knew all four parameters for diagnosing SIRS, whereas after issuing the card 100% of the trainees knew the criteria. Nobody at first knew the necessary degree of abnormality in all the values that are required to diagnose SIRS, but after intervention over 80% of the doctors knew the actual values. Notably 70% of respondents initially thought that blood pressure was a parameter for diagnosing SIRS.
In response to the question ‘What are the six organ systems whose dysfunction may indicate severe sepsis?’ no participant could initially identify more than four. After the cards had been given out, more than 90% of respondents recognised all six.
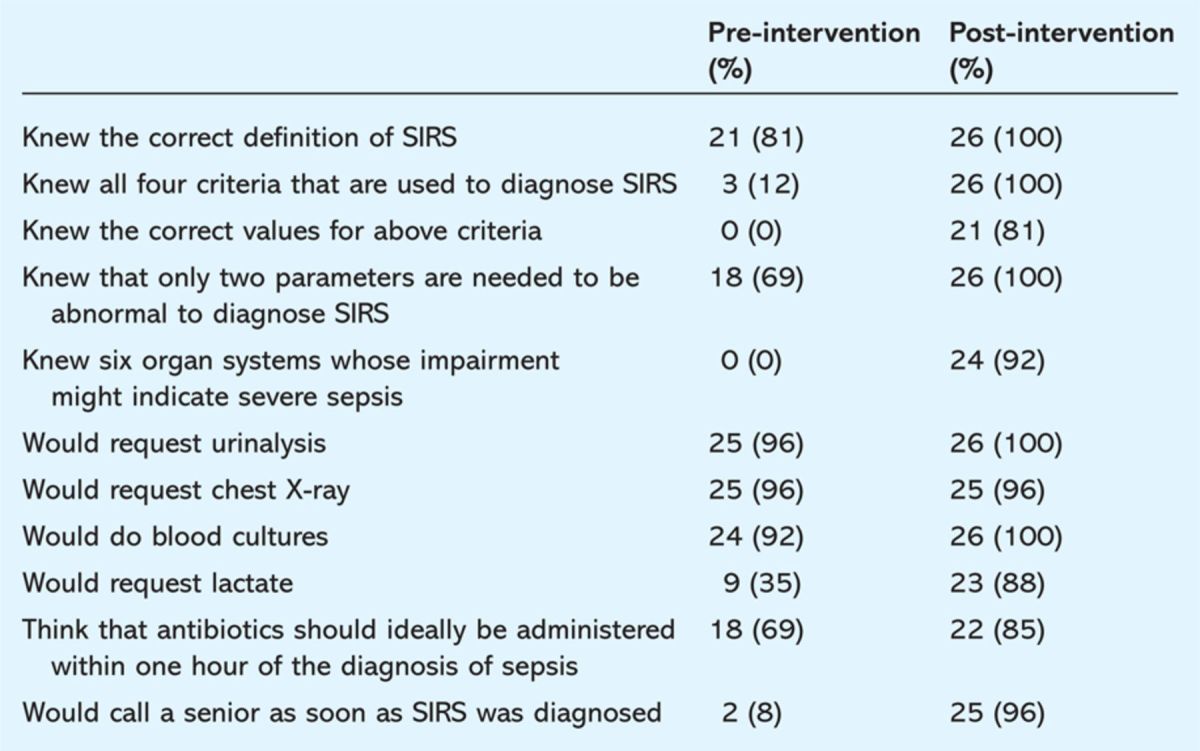
Among other management questions, only one-third of FY1 doctors would have requested a lactate in a suspected septic patient, whereas following the brief intervention 23 of the 26 would have ordered one (Table 1).
Table 1.
Results of questionnaire administered before and after foundation year 1 doctors were issued with a sepsis guideline data card.
Conclusion
This study demonstrated that the ability to recognise sepsis among FY1 doctors is poor and there are dangerous gaps in their investigation and management of such patients. The use of a brief intervention card designed to remain with the doctor at all times should increase their ability to recognise, investigate and begin suitable initial management for the septic patient. This includes early and appropriate use of lactate levels, targeted antimicrobial agents and involvement of senior support, including intensivists.
As well as reducing admissions to the intensive care unit, this should reduce morbidity and mortality from sepsis among hospital inpatients. All junior doctors involved in ward cover or emergency admissions should be given not only teaching on sepsis, but also an aide-memoire to facilitate the timely recognition and treatment of this common and dangerous condition.
References
- 1.Dellinger RP, Levy MM, Carlet JM. et al Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008; 36:296–327. [DOI] [PubMed] [Google Scholar]
- 1.Kumar A, Roberts D, Wood KE. et al Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34:1589–96. 10.1097/01.CCM.0000217961.75225.E9 [DOI] [PubMed] [Google Scholar]
- 2.Gaieski DF, Pines JM, Band RA. et al Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 2010; 38:1045–53. 10.1097/CCM.0b013e3181cc4824 [DOI] [PubMed] [Google Scholar]


