Abstract
Ambulatory emergency care (AEC) is an essential component of any acute medical unit (AMU). This statement is predicated on the clinical and financial benefits it confers. In this article, the author outlines the implementation of the Ambulatory Care Unit at Derriford Hospital and the first 6 months of service provision. The initial data collated demonstrates the impact the service has had locally on patient care and experience. It recommends ambulatory care as driver of better patient flow and enhanced patient experience within the AMU.
KEYWORDS : Ambulatory emergency care, ambulatory care unit, acute medical unit
Introduction
Ambulatory emergency care (AEC) refers to the care of the group of patients who have developed an acute problem that can be feasibly managed outside the traditional bed base. It is defined by the Royal College of Physicians (2007) as:
Clinical care which may include diagnosis, observation, treatment and rehabilitation, not provided within the traditional bed base or outpatient services and can be provided across the primary/secondary care interface.1
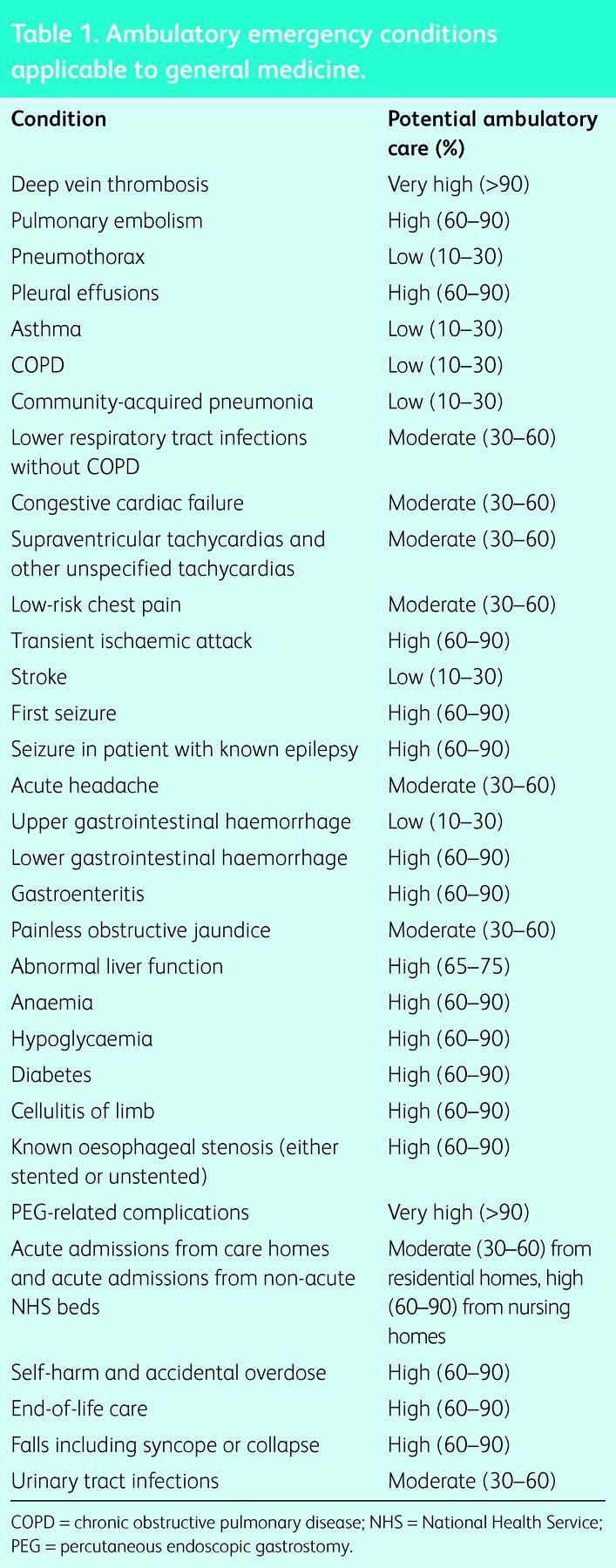
The National Health Service (NHS) Institute has recently published a revised ambulatory emergency care directory, which cites 49 clinical presentations that can be managed as emergencies on a same-day basis.2 Those applicable to general medicine are highlighted in Table 1.
Table 1.
Ambulatory emergency conditions applicable to general medicine.
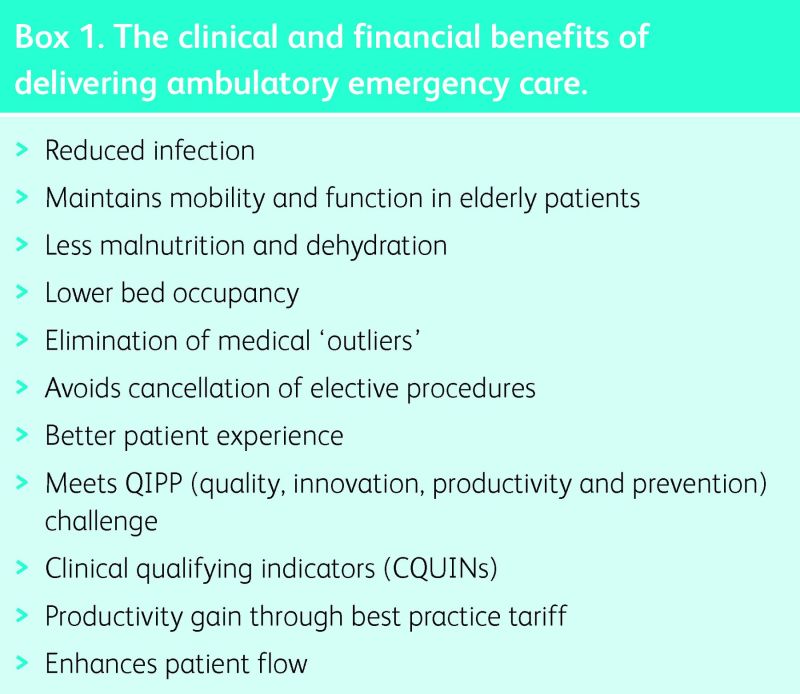
An ambulatory care unit (ACU) is an essential component of an acute medical unit (AMU); this is predicated on both the clinical and the financial benefits that it confers (Box 1).
Clinical benefits
Ambulatory care-sensitive conditions (ACSCs) account for one in every six hospital admissions.3 In the past, such patients have been managed in an inpatient setting, with the inherent risks of nosocomial infection, loss of mobility, delirium, malnutrition and dehydration, ever more poignant in light of the recent Francis report.4 Avoidable admissions consume a vast number of bed days in an already stretched service. Ambulatory care offers the ability to manage a vast array of medical conditions outside the traditional bed base and moreover the patients need not be ambulant. Additional benefits are derived through a lower bed occupancy (aim 85–90%), the elimination of medical ‘outliers’, and hence the avoided cancellation of elective procedures, all of which promote higher-quality care and a better patient experience.
Box 1. The clinical and financial benefits of delivering ambulatory emergency care.
Financial benefits
There are also economic drivers for change in the way in which we handle the high volume of medical admissions. In 2010 the Department of Health published the NHS quality, innovation, productivity and prevention (QIPP) challenge;5 it informed clinicians that the NHS needed to find £20 billion of efficiency savings, and the operating framework of 2010–11 would restrict income that could be derived from emergency activity to that contracted in 2008. All activity exceeding this would be remunerated at 30% of the tariff. The implications were profound for all AMUs. The author's unit has seen acute admissions rise from approximately 50 per 24 hours to 80 per 24 hours during this time. Ambulatory care supports the QIPP agenda. Furthermore, there are nationally agreed clinical quality indicators (CQUINs), which may also be negotiated locally with commissioners.3
Best practice tariffs have also been introduced as enablers; they are intended not only to promote high-quality care but also to deliver productivity gains in this time of financial austerity. In 2013 12 ambulatory best practice tariffs were been introduced to incentivise the delivery of ambulatory care6 with the aim of providing additional revenue if patients with certain conditions could be discharged with a length of stay (LOS) of 0 days.
Poor patient flow is a potent catalyst for change; it jeopardises both patient safety and patient experience. Flow problems cannot be solved by working harder or creating additional beds. An ACU challenges the traditional model of how a patient moves through the emergency system and prevents multiple layers in a patient's journey. General practitioner (GP) or emergency department (ED) triage to the ACU means that consultant review, with results of diagnostics, is achievable within 2 hours. An audit of process before the development of the ACU at Derriford demonstrated a 40% discharge rate on the post-take ward round, yet most of these patients had required a night's stay in hospital. The ACU allows us to challenge the variability in flow because ‘acute’ AEC cases can be booked into the system to be seen at non-peak times.
The setting
Derriford Hospital is a 1,100-bed teaching hospital serving Plymouth and its environs. The busy AMU sees over 20,000 acute medical referrals per year, which equates to between 60 and 80 patients per 24 hours. It is a 52-bed unit with separate male and female wards: Tavy is the female and Thrushel the male section of the AMU.
The ACU at Derriford Hospital opened in September 2012. The impetus for its inception was a number of factors relating to patient care, flow and financial influences. It is a consultant-delivered service run jointly by the AMU and the acute GP service (AGPS) that resides on the unit.
The vision at Derriford had originally been the design of a purpose-built clinical area that would accommodate the AGPS, acute physicians and emergency physicians in an ambulatory microcosm. This would enhance collaborative working and the efficient flow of ambulatory patients through the system. However, financial and physical constraints prevented this and hence the original ambition was replaced by a stubborn determination to ‘just do it’. The 55-bed AMU thus received a trim as one bay was transformed into an ACU with eight treatment chairs and four consultation rooms. The service currently runs from 8am–8pm and is staffed by a GP, two nurses and a healthcare assistant. A consultant physician is present between 10am–5pm, 5 days per week. It is further supported by a ‘hospital-at-home’ team which covers Cornwall and district nurses in the Plymouth area.
Results
Ambulatory care unit: initial 6-week review
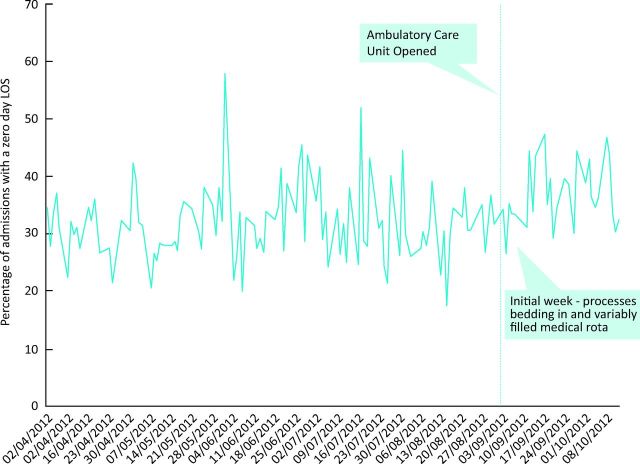
Within 6 weeks of its inception, an audit demonstrated a convincing impact on admission reduction and patients with an LOS of 0–1 day. Fig 1 illustrates the marked improvement in the proportion of patients with a 0 day LOS rate. Before the ACU, on average 32% of the acute medical take or 19 patients per day experienced an LOS of 0 days; this improved to 37%, or 27 patients per day, only 6 weeks after its development.
Fig 1.
Ambulatory emergency care – initial 6-week review (3 September to 12 October 2012). LOS = length of stay.
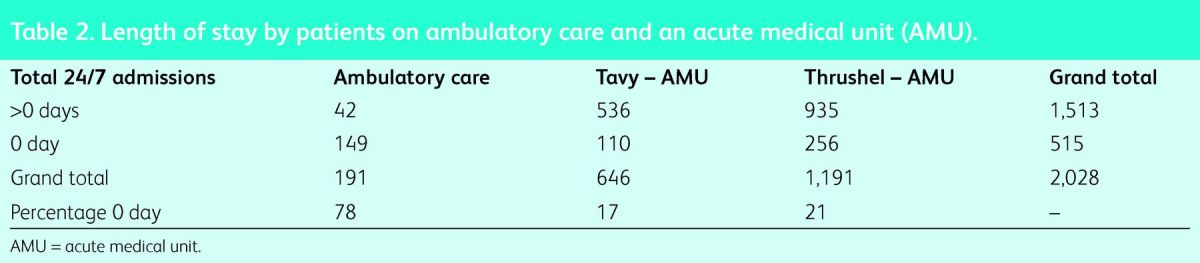
From the initial 6-week review Fig 1 shows that the current same-day ambulatory rates and LOS across the AMU and ACU demonstrate a 78% discharge rate from the ACU, with just over 20% requiring conversion to inpatient care (Table 2). It does, however, highlight a significant proportion of ‘ambulatory’ activity being treated through AMU beds. The initial, relatively high proportion requiring inpatient care probably reflects a naivety in identifying ambulatory care patients in the early stages. Indeed, experience has allowed better identification of patients and this is reflected in a discharge rate of 98.7% in a recent audit.
Table 2.
Length of stay by patients on ambulatory care and an acute medical unit (AMU).
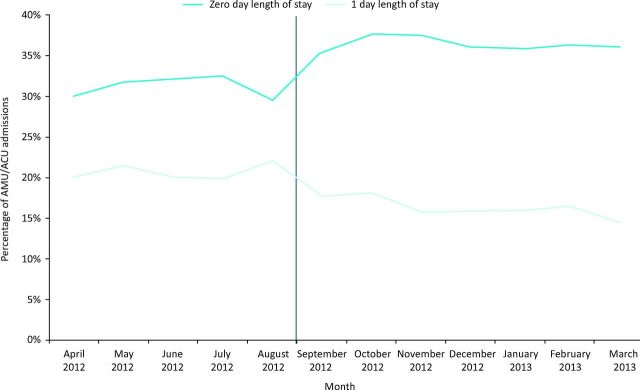
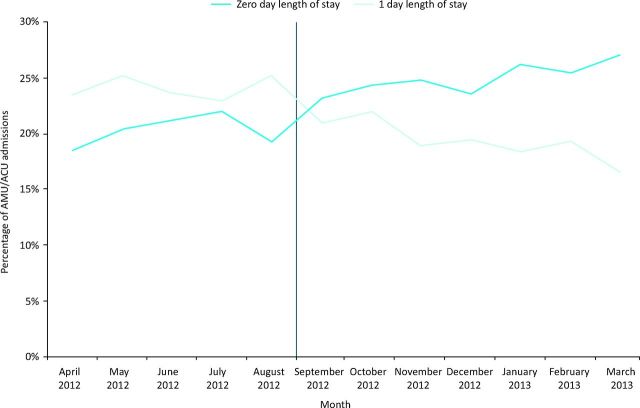
Ambulatory care unit: 6-month review
The same review at 6 months illustrated a more impressive impact on admission avoidance (Figs 2 and 3). Almost 37% of the acute medical take was managed with an LOS of 0, compared with 30% before the implementation of the ACU or an average of 30 patients per day. A recent audit has shown that only 1.3% of ACU patients have required conversion to inpatient status, highlighting the improved ability to identify patients with ACSCs. The same audit demonstrated that, through the use of the Amb score7 to identify appropriate patients, we now fail to identify fewer than 10 patients per week. Moreover the 30-day readmission rate is negligible; only 4 ACU patients have been readmitted in the last 6 months. We believe that this may be due to patients feeling more supported by the ‘open access’ policy (on discharge patients are given a number to call to initiate an appointment should their condition change).
Fig 2.
Acute medical unit/ambulatory unit emergency admissions (including acute GP service) by length-of-stay banding. ACU = ambulatory care unit; AMU = acute medical unit.
Fig 3.
Acute medical unit/ambulatory care unit emergency admissions, emergency department-referred only by length-of-stay banding. AMC = ambulatory care unit; AMU = acute medical unit.
Lessons learnt
Effective patient management as a medical day case is clinically rewarding and yet relies on a number of factors.
Identifying ambulatory care patients
This requires skill and experience on the part of the clinician. It challenges the mind-set that admission is safe and will ensure that diagnostics are prioritised accordingly. A wander around the ward would often identify patients who had been ‘admitted’ to a bed. This has been addressed in a number of ways, often simple, eg asking the ambulance crew to request that patients attend hospital in their clothes and by asking GPs, at the point of referral, whether their patients would be suitable for ambulatory care. The service was directed at ‘all comers’ rather than defined by conditions set out in ambulatory care pathways. This may engender concerns about patient safety, especially with presentations such as chest pain, but experience and application of the Grace score have allowed safe triage of a subpopulation of patients with low-risk chest pains who were previously condemned to a hospital bed.
Despite vigilance, a significant proportion of patients were not identified (about 20%) in the early days, resulting in ‘ambulatory care’ at the bedside. A recent audit applying the ambulatory score4 to all patients ‘admitted’ to a bed demonstrated that, on average, the staff were failing to identify only eight patients a week suitable for ACU. Referral or ‘signposting’ of patients to ambulatory care is the combined responsibility of the referring GP, ED and front-door triage team. The author's groups has found that this ‘open-door’ policy increases yield. Furthermore, in an attempt to release beds earlier in the day, the author's group has found ambulatory care to be a useful setting for the completion of investigations. In the same vane, patients can be discharged early from the ward with follow up in the ACU.
Collaborative working
Across primary, secondary and social care, collaborative working has been promoted by joint working with the AGPS on the AMU. Despite this, the success of the ACU at Derriford Hospital relied on recruitment of specialty involvement. All too often, admission is the path of least resistance and patients are admitted for specialist review. A separate neurology take has been exploited and their engagement in the service development has been crucial. First, fits, headaches and transient ischaemic attacks are all reviewed in the ACU. Daily input from gastroenterology and respiratory specialties has facilitated rapid access to endoscopy and outpatient management of pleural effusions. Cardiology is also on hand and bedside echocardiograms easily obtained. More recently the national directive regarding acute oncology services8 has triggered daily input to the ACU. Acute oncology has been driven by the NHS cancer action team to provide ambulatory assessment of oncological problems, hence avoiding admissions. This has not only permitted more timely clinical assessment of oncology patients, but also obviated the need for admission for conditions such as post-chemotherapy hypomagnesaemia, hypercalcaemia of malignancy, blood transfusion and pleural drainage, all of which can be managed in the treatment area. The ED adopted an ‘ambulatory care passport’, which conferred the essential clinical information and allowed a seamless passage to the ACU. The engagement of ED physicians has been not only invaluable but also a catalyst for the next stage in developing urgent care services at Derriford.
Patient experience
This has been mapped out using the evidence-based design (EBD) approach as recommended by the National Institute for Improvement and Innovation. This sets out to understand and capture the experiences of the patient and carer as they progress through the system. The feedback is then used to redesign and improve the system. A recent patient survey revealed >95% patient satisfaction and 100% would recommend the ACU to friends and family. This might be attributable to the fact that 76% were seen and discharged within 2 hours.
Timely diagnostics
These are essential to efficient clinical care. The initial concern that supply (of the ACU) would increase the demand for diagnostics has not been evidenced. All investigations are prioritised as ‘inpatients’, which is important to patient experience. As a minimum this includes computed tomography (CT), magnetic resonance imaging (MRI), echocardiography, ultrasonography, pulmonary function tests and endoscopy. The imminent acquisition of another CT scanner will permit same-day CT coronary angiography.
Conclusions
Ambulatory care is an essential component of the AMU. It offers unquestionable clinical and financial benefit to the AMU and indeed the NHS. The key feature of timely triage, ‘at the front door’, by a senior clinician improves patient care and experience, carves out queues and reduces unscheduled admissions. At Derriford Hospital, a significant proportion (40%) of acute medical referrals have been identified that can be managed in an ambulatory fashion, and furthermore need not be ambulant. Its success here must be attributed to a combination of proactive clinicians, an innovative ward manager, a facilitative management team, and the dissolution of silos and specialty engagement.
This vibrant initiative has yielded a note of optimism at Derriford Hospital. Although the hospital faces a rising number of admissions, the staff have been forced to review the anachronistic way in which they practise medicine. The ACU challenges the pervasive disillusionment faced by patients and clinicians in the NHS today. It exploits the need for change in the face of financial austerity, offers excellent patient experience and is clinically rewarding. It is ‘the best in the best of all possible worlds’; we all have the ambulatory ability to ‘cultivate our garden’.9
References
- 1.Royal College of Physicians Acute Medical Care – the right person, in the right setting – first time. Report of the Acute Medicine Task Force RCP: London, 2007. www.rcplondon.ac.uk/sites/default/files/documents/acute_medical_care_final_for_web.pdf [Accessed 13 May 2014]. [Google Scholar]
- 2.NHS Institute Directory of Ambulatory Emergency Care, 3rd edn London: NHS Institute, 2012. www.institute.nhs.uk/ambulatory_emergency_care/…ambulatory_emergency_care/directory.html [Accessed 16 January 2014]. [Google Scholar]
- 3.The King's Fund. Data Briefing Emergency Hospital Admission for Ambulatory Care Sensitive Conditions: Identifying the potential reductions. London: The King's Fund, 2012. [Google Scholar]
- 4.Francis R. The Mid Staffordshire NHS Foundation Trust Public Inquiry. London: HMSO, 2013. www.midstaffspublicinquiry.com/report [Accessed 19 March 2014]. [Google Scholar]
- 5.Department of Health NHS Reference Costs 2009–2010. London: DH, 2011. www.gov.uk/government/publications/nhs-reference-costs-2009-2010 [Accessed 16 January 2014]. [Google Scholar]
- 6.Department of Health Update to Best Practice Tariffs. London: DH, 2011. www.gov.uk/government/news/update-to-best-practice-tariffs [Accessed 16 January 2014]. [Google Scholar]
- 7.Ala L, Mack J, Shaw R, et al. Selecting ambulatory emergency patients from the medical in-take; the derivation and validation of the Amb score. Clin Med 2012;12:420–6. 10.7861/clinmedicine.12-5-420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health Improving Outcomes: A strategy for cancer. London: DH, January 2011. www.gov.uk/government/publications/the-national-cancer-strategy [Accessed 16 January 2014]. [Google Scholar]
- 9.Voltaire Candide, ou L’Optimisme. 1759. [Google Scholar]