Abstract
Hypernatraemia is a common finding among patients presenting to hospital. The aim of this observational study was to discover what types of patients presented with hypernatraemia and whether they were appropriately managed. The management of hypernatraemia was audited against common standards of care. Hypernatraemia at presentation carries a poor prognosis and in this study management of hypernatraemia was found to be done poorly, possibly because for many patients aggressive management was deemed inappropriate. The majority of patients who present with hypernatraemia are older, dependent and/or suffer from cognitive impairment. Many of these patients do not have a reversible cause for their hypernatraemia. These patients need to be recognised, ideally in the community, so that inappropriate admission can be avoided, but also on presentation to hospital so that appropriate care, which may be end-of-life care, can be provided.
KEYWORDS : Hypernatraemia, sodium, dementia
Introduction
Hypernatraemia is a common finding among patients presenting to the medical admissions unit or hospital, especially older patients.1–3 Having observed that patients presenting with hypernatraemia to the Frenchay Hospital, Bristol, tended to be older or from care homes, and that the management of these patients was inconsistent, I undertook this study to determine the types of patient who were being admitted with hypernatraemia, and whether their management was appropriate.
Hypernatraemia results most often from unreplaced water that is lost from the gastrointestinal tract (vomiting or osmotic diarrhoea), skin (sweat) or urine (eg diabetes insipidus or an osmotic diuresis because of glycosuria in uncontrolled diabetes mellitus).1 Excessive water loss seldom leads to hypernatraemia because the resulting increase in plasma osmolality stimulates thirst, which leads to increased intake of fluids that lowers the serum sodium into the normal range. Thus, in patients who have access to water, hypernatraemia primarily occurs in those who are unable to sense or respond to thirst normally. This is most commonly seen in infants and in adults with impaired mental status, particularly older patients.2,3 Older patients might also have a diminished thirst response to osmotic stimulation via an unknown mechanism.4,5
Hypernatraemia is often poorly managed. Recently, a signal from the National Patient Safety Agency was issued concerning the potential risk of central pontine myelinolysis (CPM) syndrome following rapid correction of sodium.6 A search of incident reports to the National Reporting and Learning System between January 2008 and June 2011 identified 15 incidents of CPM. Three incidents were associated with severe harm. These incidents were caused by errors in the strength, volume or rate of sodium chloride infusions administered to patients.
The aim of this observational study was to see what types of patient were admitted with hypernatraemia and whether they were appropriately managed. The details of patients with hypernatraemia at presentation to the medical admissions unit, over a 12-month period from April 2010 until March 2011, were noted. The management of hypernatraemia was audited against common standards of care.1,6,7
Method
The case notes of all patients whose serum sodium was >150 mmol/l at presentation were reviewed retrospectively. Demographic data were recorded, including age, sex and from where the patient was admitted. The presenting complaints, final diagnoses, and outcome at discharge and 1 year later were also noted.
Management of these patients was audited by collecting the following data: rate of correction of serum sodium; type of fluids prescribed; evidence that the rate of infusion was calculated by estimating the water deficit; and frequency of serum sodium measurement.
The appropriateness of management was audited against the following standards:
In patients with hypernatraemia that has developed over days, or is of unknown duration, the serum sodium concentration should be reduced at a maximal rate of 0.5 mmol/l per hour. A targeted fall in the serum sodium of 10 mmol/l per day is recommended for all patients with hypernatraemia, except those for whom hypernatraemia has developed over hours.1,6,7
Only hypotonic fluids are appropriate (pure water orally, glucose 5% intravenously, 0.45% sodium chloride intravenously), unless there is frank circulatory collapse, when sodium chloride 0.9% might be appropriate.1
The rate of infusion should be set by estimating the water deficit.6
Serial measurements of serum sodium concentration should be performed: in patients who have large ongoing water losses the serum sodium should be measured approximately every 4 hours during the first day of therapy, while in patients without ongoing losses measure serum sodium at 6 hours, and if the serum sodium is falling at the desired rate, then every 8–12 hours.6,7
Results
Notes reviewed
In total, 79 patients presented to the Frenchay Hospital over a 12-month period with hypernatraemia (serum sodium >150 mmol/l). Of these, 55 sets of notes were available for review (70%).
Demographic data
Patients presenting with high serum sodium were in the age range 43–94 years (mean age 81 years, median 84 years). Forty-five patients (89%) were aged 65-years or over. Only 12 (22%) were admitted from home where they were living independently, whereas 8 (14%) came from home with carers, and 35 (64%) from care homes. Of the patients, 29 (53%) had previously been found to have dementia. Overall, 38 of 55 (69%) patients died within 1 year of their admission to Frenchay Hospital; 28 of these (51%) of patients died during that admission.
Presenting complaints and diagnoses
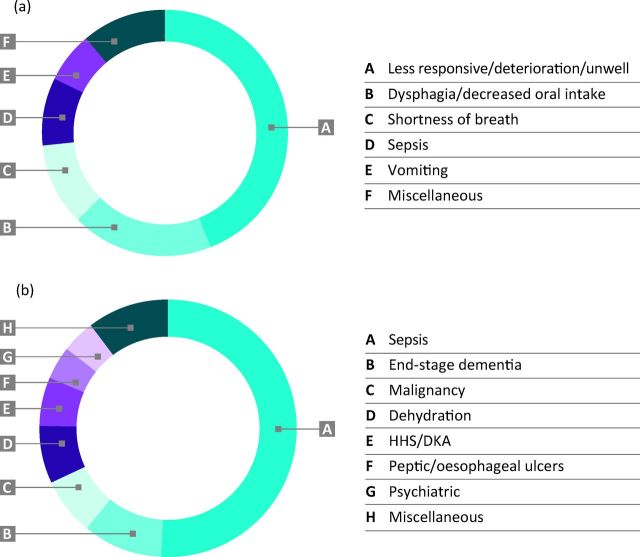
Fig 1a depicts the presenting complaints, and Fig 1b the final diagnoses, of patients with hypernatraemia on presentation to Frenchay Hospital.
Fig 1.
Presenting complaints (a) and final diagnoses (b) of patients presenting with hypernatraemia to Frenchay Hospital over a 12-month period from 2010 to 2011.
Management
Not all patients had their hypernatraemia treated. Three patients were discharged back to their nursing homes for palliative care. Seven patients did not have their serum sodium rechecked, either because they died, or were deemed to be dying when blood tests might have been done. One hypernatraemia result was a spurious result that was normal on rechecking. Of the serum sodium levels that were rechecked, the rate of correction of hypernatraemia was appropriate in only 24 of 43 patients (56%). However, in 47 of 51 (92%) of treated patients, appropriate fluids were used. In only one set of notes was there evidence that the rate of infusion was calculated by estimating the water deficit.
Sodium was measured once daily in most patients. In four patients, it was measured every 12 hours, but in no patients was it measured more frequently.
Case study 1
Mrs MB was an 87-year-old woman who was admitted from home, where she had carers four times daily. She was admitted after being found unresponsive by her carers. They reported that she had had difficulty in swallowing over the preceding few days. Although she had an extensive past medical history, including ischaemic heart disease, previous strokes and severe osteoarthritis, she did not have dementia.
On admission, her serum sodium was 163 mmol/l. Her blood glucose was normal at 5.2. A diagnosis of sepsis secondary to a lower respiratory tract infection was made. She was treated with intravenous antibiotics and fluids, initially sodium chloride 0.9% because she was hypotensive, and then glucose 5%. She was too drowsy to take oral fluids. Despite these intravenous fluids, her sodium level did not change. She remained very unwell, and showed no improvement with intravenous antibiotics. The decision was made, after discussion with family, that escalation of care was not appropriate. She died peacefully approximately 48 hours after admission.
Case study 2
Mrs ES was a 93-year-old woman who was admitted from a nursing home with ‘general deterioration, and not eating or drinking’. In the home, she required all care, was bedbound and doubly incontinent. She had severe dementia.
On admission, her serum sodium was 159 mmol/l. She was seen by a care of the elderly consultant, who diagnosed end-stage dementia. After discussion with her family and her care home, she was discharged back to the home for palliative care. She spent 14 hours in hospital, initially in the emergency department and then in the medical assessment unit. She died 2 days after returning home.
Discussion
This study confirms that patients admitted with hypernatraemia are more likely to be older (the mean age of the study patients was 81 years, with 89% being 65-years old or more). The findings also suggest that being dependent or less mobile contribute to hypernatraemia (only 22% of patients were living at home independently, whereas 64% were admitted from care homes) as does having dementia (53% of patients). Previous studies have shown that electrolyte imbalances are more prevalent in older people,2,3,8 those living in institutions9 and those with Alzheimer's dementia.10
Only 12 of the 55 patients who were admitted lived independently at home. These included three patients who presented in a hyperosmolar hyperglycaemic state (HHS) or with diabetic ketoacidosis (DKA), two patients who had a psychiatric reason for not drinking (psychotic depression and bipolar disorder), two patients who had severe oesophageal and peptic ulcers, and a patient with a blocked oesophageal shunt. These patients either had an endocrine cause for their hypernatraemia, or a medical explanation for why they had been unable to take water orally. These causes of hypernatraemia are treatable and so future hypernatraemia is preventable. All these patients were treated and discharged home.
The patients who presented with hypernatraemia secondary to HHS or DKA were well managed, but in most other patients, hypernatraemia was poorly managed. Despite suitable fluids being used in over 90% of cases, the rate of correction of hypernatraemia was appropriate in only 56% of cases. Other studies have shown similar results: a retrospective review of 131 patients with severe hypernatraemia found that, although the rate of sodium reduction was as recommended (<0.5 mmol/l/h) in 90% of patients, hypernatraemia was corrected in only 27% of patients after 72 h of treatment.11 Explanations for the current results might be that the rate of fluid infusion was not calculated or that sodium levels were not rechecked often enough. Improving the management of patients with hypernatraemia will require education of frontline junior staff, and an accessible and straightforward protocol, which ideally incorporates the water deficit formula in a simple calculation.
However, it is likely that, in many patients, hypernatraemia was not managed according to best practice guidelines because such management was deemed inappropriate. For most patients who presented with hypernatraemia, the final diagnoses (sepsis, malignancy or dehydration) would not be expected to increase serum sodium unless the patient had been unable to take oral fluids; therefore, these patients did not have a reversible cause for their hypernatraemia. Explanations for this presentation in these patients include that they were older, less mobile or dependent and or had dementia. The fact that most patients were older and dependent, did not have reversible causes for their hypernatraemia and, in some cases, were dying, could explain why hypernatraemia was not managed according to best practice guidelines, given that aggressive management might often have been inappropriate. I propose that every older patient who presents to hospital with hypernatraemia should be referred for a specialist geriatric assessment so that appropriate levels of care can be determined. I also suggest that guidelines for the management of patients with hypernatraemia should have as an initial step, the question: ‘Does your patient have end-stage dementia or are they in the final stages of another illness?’ If the answer to this question is yes, then supportive care only should be given.
Hypernatraemia is a poor prognostic finding: of the 55 patients who had hypernatraemia at presentation, 69% had died within 12 months of their presentation. Over half died during that admission. This poor prognostic factor has been identified previously. One study of 2,894 patients admitted over 5 years found that mortality is positively related to serum sodium levels, with mortality rates of 71.4% in subjects with serum sodium levels >154 mEq/l. Both serum sodium levels and age were independent risk factors for mortality.12 Another study reported an overall mortality rate of 48.6% for inpatients with hypernatraemia.8 Similarly, in a recent study, nursing-home residents with advanced cognitive impairment who underwent multiple hospitalisations for dehydration were found to have poor survival.13
Given that most patients admitted with hypernatraemia do not have a reversible cause for their hypernatraemia, and that hypernatraemia is a poor prognostic factor, this raises the question as to whether the admission of such patients is appropriate. Patients with end-stage illnesses, including dementia, who are dehydrated because they are unwilling or unable to eat and drink, could be more holistically managed in the community. It is imperative that such patients are identified early to enable discussion with families and carers as to the appropriate management when the patient declines oral intake. Patients with hypernatraemia can be difficult to detect using clinical signs,14 but any variation in conscious level, or a refusal of oral intake, should alert carers.
Such patients in care homes who appear to be becoming dehydrated should be brought to the attention of their general practitioner early, so that blood chemistry can be measured in the community if necessary and, if appropriate, plans for end-of-life care made. One might then be able to prevent unnecessary and distressing admissions for these frail patients at the end of their lives.
Conclusions
Patients who are admitted with hypernatraemia are more likely to be older, immobile or have dementia, and often do not have a reversible cause for their hypernatraemia. Admission with hypernatraemia carries a poor prognosis. I suggest that patients suffering from terminal illnesses, including end-stage dementia, should not be managed aggressively, but should receive symptomatic treatment only, and if possible, remain in the community for end-of-life care.
References
- 1.Adrogue HJ, Madias NE. Hypernatraemia. N Engl J Med 2000;342:1493–9. 10.1056/NEJM200005183422006 [DOI] [PubMed] [Google Scholar]
- 2.Snyder NA, Feigal DW, Arieff AI. Hypernatraemia in elderly patients. A heterogeneous, morbid, and iatrogenic entity. Ann Intern Med 1987;107:309. 10.7326/0003-4819-107-2-309 [DOI] [PubMed] [Google Scholar]
- 3.Schlanger LE, Bailey JL, Sands JM. Electrolytes in the aging. Adv Chronic Kidney Dis 2010;17:308–19. 10.1053/j.ackd.2010.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Phillips PA, Bretherton M, Johnston CI, Gray L. Reduced osmotic thirst in healthy elderly man. Am J Physiol 1991;261:R166. [DOI] [PubMed] [Google Scholar]
- 5.Faull CM, Holmes C, Baylis PH. Water balance in elderly people: is there a deficiency of vasopressin? Age Ageing 1993;22:114–20. 10.1093/ageing/22.2.114 [DOI] [PubMed] [Google Scholar]
- 6.National Patient Safety Agency Risk of harm from CPM syndrome following rapid correction of sodium, 2012. www.nrls.npsa.nhs.uk/resources/?entryid45=132971 [Accessed 3 February 2014]. [Google Scholar]
- 7.Wolters Kluwer Health , 2014. www.uptodate.com/contents/treatment-of-hypernatraemia [Accessed 3 February 2014]. [Google Scholar]
- 8.Borra SI, Beredo R, Kleinfeld M. Hypernatremia in the aging: causes, manifestations, and outcome. J Natl Med Assoc 1995;87:220–4. [PMC free article] [PubMed] [Google Scholar]
- 9.Onem Y, Terekeci H, Kucukardali Y, et al. Albumin, hemoglobin, body mass index, cognitive and functional performance in elderly persons living in nursing homes. Arch Gerontol Geriatr 2010;50:56–9. 10.1016/j.archger.2009.01.010 [DOI] [PubMed] [Google Scholar]
- 10.Turgutalp K, Özhan O, Gök Oğuz E, et al. Community-acquired hypernatremia in elderly and very elderly patients admitted to the hospital: clinical characteristics and outcomes. Med Sci Monit 2012;18:CR729–34. 10.12659/MSM.883600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alshayeb HM, Showkat A, Babar F, et al. Severe hypernatremia correction rate and mortality in hospitalized patients. Am J Med Sci 2011;341:356–60. 10.1097/MAJ.0b013e31820a3a90 [DOI] [PubMed] [Google Scholar]
- 12.Molaschi M, Ponzetto M, Massaia M, et al. Hypernatremic dehydration in the elderly on admission to hospital. J Nutr Health Aging 1997;1:156–60. [PubMed] [Google Scholar]
- 13.Teno JM, Gozalo P, Mitchell SL, et al. Survival after multiple hospitalizations for infections and dehydration in nursing home residents with advanced cognitive impairment. JAMA 2013;310:319–20. 10.1001/jama.2013.8392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chassagne P, Druesne L, Capet C, et al. Clinical presentation of hypernatremia in elderly patients: a case control study. J Am Geriatr Soc 2006;54:1225–30. 10.1111/j.1532-5415.2006.00807.x [DOI] [PubMed] [Google Scholar]