Glucocorticoids are widely used in many medical specialties for their anti-inflammatory and immunosuppressive qualities. The majority of glucocorticoid use occurs in the outpatient setting. Long-term glucocorticoid use is associated with several side effects, including the development of hyperglycaemia. Observational data for many, if not most, medical and surgical conditions requiring hospitalisation suggest that the additional presence of hyperglycaemia or diabetes is associated with poorer outcomes.1,2 Despite this association there are no data on the prevalence of glucocorticoid use in hospitalised inpatients.
We conducted a single centre prevalence study carried out over two consecutive days in January 2014, assessing every adult bed (n = 940) in our institution, excluding the accident and emergency department, coronary care, and intensive care units. Our aim was to look at the number of patients on glucocorticoids and to see how many had their glucose levels measured.
We found that 120 patients (12.8%) were being treated with glucocorticoids; 99 of these (82.5%) were on prednisolone. The mean daily dose (MDD) for prednisolone was 25.0 mg ± 12.5 (range 0.5–60). Sixteen patients (13.3%) were receiving dexamethasone with a MDD of 9.2 mg ± 6.5 (range 0.5–20). The remaining four patients (3.3%) were being treated with hydrocortisone either intravenously or orally, with a MDD of 107.5 mg ± 106.9 (range 20–200). Sixty-four (53.3%) of patients who were being treated with glucocorticoids had been receiving their treatment for longer than 10 days at the time the data was collected.
Table 2.
Baseline characteristics and steroid use of patient cohort (n = 120).
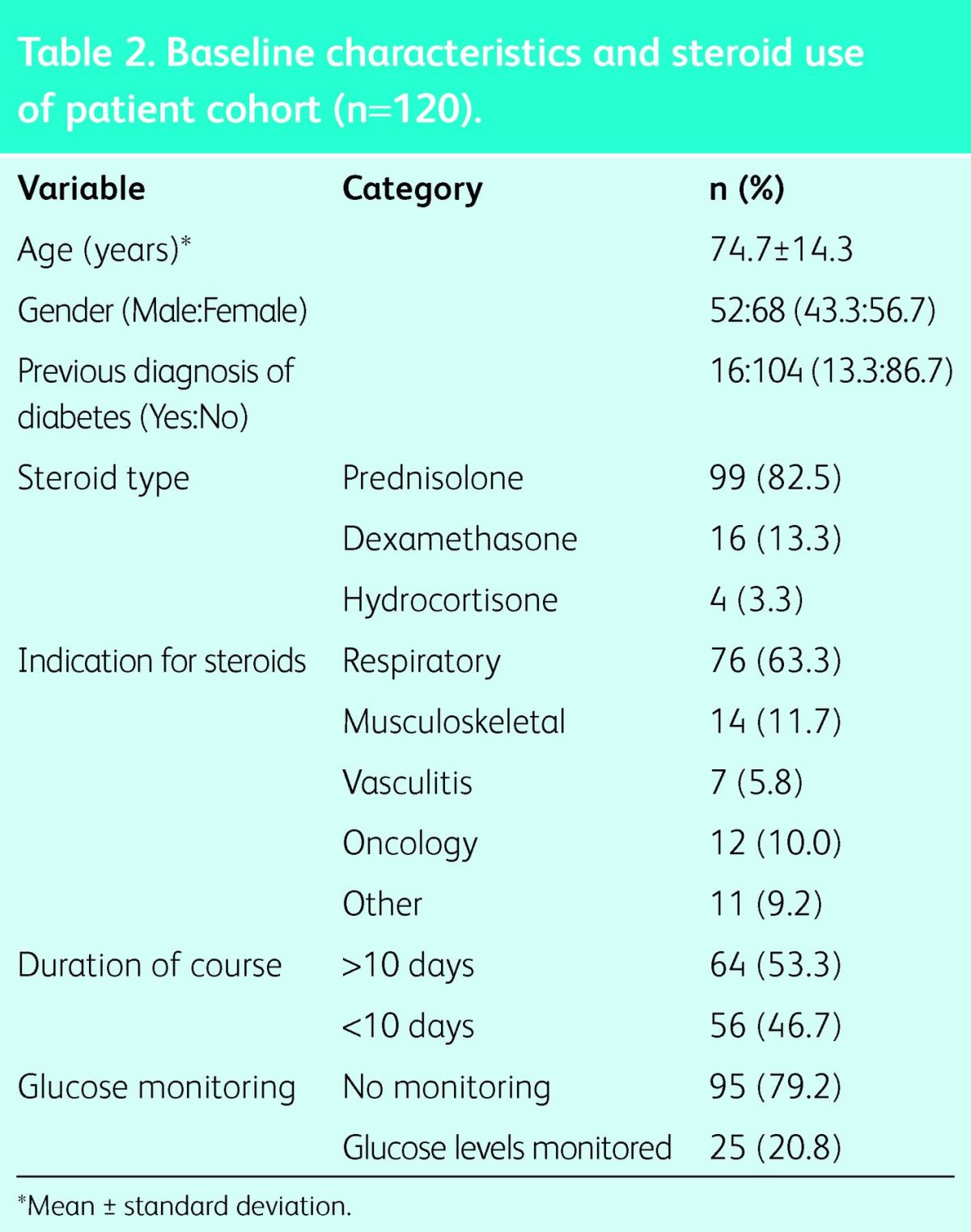
Of the 120 patients receiving glucocorticoids, only 25 (20.8%) had their blood glucose levels measured during their time as inpatients. Of these, 13 had pre-existing diabetes. There were three patients who had diabetes and were receiving glucocorticoids but had no regular blood glucose measurements. Compared to those without diabetes, patients with pre-existing diabetes were more likely to have their glucose levels measured (p < 0.001). Of the patients without diabetes, only 12 patients (11.5%) were having their blood sugars measured while on glucocorticoids.
This study has highlighted the need for continued improvement to the care of hospitalised inpatients. Despite the knowledge that glucocorticoids cause hyperglycaemia and that high levels of glucose are associated with harm, very few patients in this study were having their glucose levels measured.
We suggest that all hospitalised patients being treated with glucocorticoid doses greater than an equivalent of 7.5 mg of prednisolone must have their blood glucose levels measured regularly. Initially this should be postprandially once or twice per day, and if the glucose level is found to be >12 mmol/l during any 24-hour period then testing should be before meals and before bedtime. If glucose levels remain >12 mmol/l then treatment (initially with sulfonylureas) should be started. A new guideline produced by the Joint British Diabetes Societies Inpatient Care group addresses glucocorticoid associated hyperglycaemia and is freely available at www.diabetologists-abcd.org.uk/JBDS/JBDS.htm.
References
- 1.Baker EH, Janaway CH, Philips BJ, et al. Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax 2006;61:284–9. 10.1136/thx.2005.051029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwon S, Thompson R, Dellinger P, et al. Importance of perioperative glycemic control in general surgery: A report from the surgical care and outcomes assessment program. Ann Surg 2013;257:8–14. 10.1097/SLA.0b013e31827b6bbc [DOI] [PMC free article] [PubMed] [Google Scholar]


