Abstract
Regular supraventricular tachycardia (SVT) is frequently encountered in clinical practice. Guidelines are available from the National Service Framework (NSF) for the treatment of patients attending emergency departments (ED) with SVT. These recommend a thyroid-function test (TFT) and arrhythmia electrocardiography (ECG), and referral to a heart-rhythm specialist on discharge. Hospital admission is rarely required. In our multicentre study, we examined the implementation of these guidelines among patients attending the ED with SVT. Only 34% of patients had specialist referrals, with an average wait of 50.3 days (the majority of delays resulted from referral requests from general practitioners). A history of previous SVT, the mode of tachycardia termination, patient age and/or comorbidities were similar for the 27 (23.5%) patients who were admitted overnight. Of these, 15 (13%) of the total 115 patients who attended ED with regular SVT were referred for Holter monitoring despite having ECGs demonstrating arrhythmia. Low referral rates, unnecessary investigations and admissions indicate a need for improvement for better patient care and to minimise healthcare costs. We have formulated a standard operating procedure, which will be available via the College of Emergency Medicine website.
Key Words: regular SVT, emergency department admission, National Service Framework
Introduction
Regular narrow QRS complex supraventricular tachycardia (SVT) is a benign fast heart rhythm that is frequently encountered in clinical practice.1–4 It predominantly includes two forms of tachycardia (atrioventricular (AV) nodal re-entry and AV re-entry) and occurs in 35 out of 100,000 person years, with a prevalence of 2.29 per 1,000 people.5 It is sometimes possible for patients to terminate the tachycardia themselves by simple manoeuvres that change the properties of the AV node. Patients who know their diagnosis and have had a clear explanation of the problem do not always need to attend hospital. Nevertheless, attendance at hospital emergency departments (ED) is often required for treatment.
For those patients admitted to the ED, the National Service Framework (NSF) guidelines for treatment of regular SVT state that, after successful termination of the arrhythmia:6
patients should be given a copy of their electrocardiogram (ECG) recorded during the arrhythmia
they should have a thyroid function test (TFT)
they do not need to be admitted to hospital overnight
they should be referred to a heart rhythm specialist.
Given the range of medical problems that ED and medical on-call teams are expected to deal with, it is an understandable challenge for them to use all of the available guidelines that pertain to these conditions. To our knowledge, there are no studies that have evaluated the implementation of the guidelines for SVT management in practice. In the present multicentre study, we performed a retrospective notes-based audit of patients admitted to four tertiary-centre EDs with an ECG-confirmed diagnosis of SVT over a 12-month period. We investigated whether NSF guidelines were being followed.
Methods
Study design
The present study was a retrospective audit. The ED notes for all patients with a recorded admission diagnosis of regular SVT were examined over a 12-month period across four tertiary centres (St Bartholomew's Hospital, St Mary's Hospital, Charing Cross Hospital and Hammersmith hospital). Ethical approval was not required, as advised by the local ethics committee.
Patients
All patients admitted to the ED with an ECG-confirmed diagnosis of regular SVT were included in the study. Patients were excluded if the diagnosis was atrial fibrillation or sinus tachycardia, and also when no arrhythmia ECG was recorded.
Data collection
Patients were identified from the hospital ED databases. The ED notes of the identified patients were examined to confirm an ECG diagnosis of regular SVT.
Hospital notes and admission records were reviewed to determine whether the patient: had had previous admissions with tachycardia; had been given a copy of their ECG; had been admitted overnight; had had TFT; and had been referred to a heart rhythm specialist. We also determined how long it took for referral to occur.
Statistics
Data were analysed using SPSS version 16 and are summarised as means with standard deviations for continuous data, and percentages for dichotomous data.
Results
A total of 115 patients attended the ED with a confirmed diagnosis of regular SVT. Of these, 35 (30%) were men with a mean age of 49.8 years. A past history of SVT was noted in 34% of the patients, of whom 13% were taking anti-arrhythmic medication.
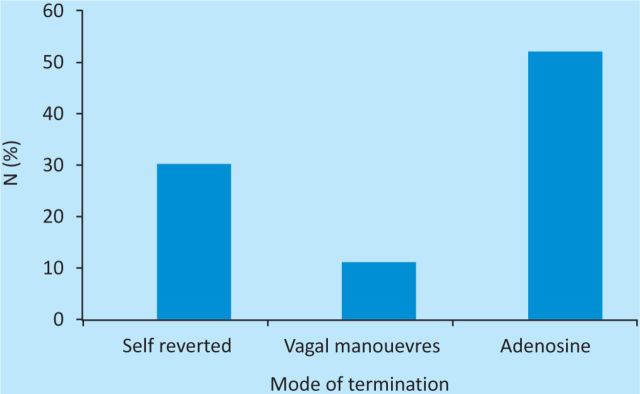
Most of the patients received appropriate clinical treatment. The SVT spontaneously reverted to sinus rhythm in 39 (34%) patients, whereas 13 (11%) converted with vagal manoeuvres and 63 (55%) needed adenosine to terminate the arrhythmia (Fig 1).
Fig 1.
Arrhythmia termination.
There were a few (four) patients in whom vagal manoeuvres were not tried before the administration of adenosine. In two cases, adenosine was not given as per recommended guidelines (same dose of 6 mg repeated) for arrhythmia termination. Only 9 (7%) patients were given a copy of their arrhythmia ECG on discharge, but 65% of patients had a TFT. In total, 15 patients were referred for Holter monitoring despite having a diagnostic 12-lead ECG demonstrating regular SVT. The referral rates and admission times are summarised in Table 1.
Table 1.
Summary of hospital admissions and referral times.

In total, 27 patients were admitted to a medical unit, spending a mean of 2.3 nights in hospital. Five of these patients required admission because of exacerbation of underlying comorbidities (chronic obstructive pulmonary disease and myelodysplasia). However, in the remaining 81% of admissions, the reason for overnight admission was not clear and it was not related to having a history of previous SVT, the mode of tachycardia termination, patient age or comorbidities.
Only 39 (34%) patients were referred to the heart rhythm service. The remainder were either given no further follow up (n=44) or were asked to get their general practitioners (GPs) to refer them (n=32), of whom nine were referred to a heart rhythm clinic. The average waiting time for the referred patients was 50.3 days, with the majority of delays occurring when the GP was requested to refer the patient to specialist care.
Patients with a previous history of SVT had significantly higher electrophysiology (EP) referral rates compared with those with no previously documented arrhythmia (Fig 2; p=0.01).
Fig 2.
Referral rates in patients with a past history of SVT. SVT = supraventricular tachycardia.
We also found that patients admitted to ED with an on-site heart rhythm service had a significantly higher specialist referral rate (48.9% vs 23.5%, p=0.005; Fig 3).
Fig 3.
Effect of on-site heart rhythm service on referral rates.
Discussion
This study shows that patients admitted to ED with regular SVT are often appropriately sent home the same day, but often without a copy of their diagnostic ECG. A significant number are admitted to hospital and undergo inappropriate investigations, adding to healthcare costs. Referral for definitive investigation and treatment is delayed when the patient's GP is asked to make a referral for specialist care.
Obtaining copies of the diagnostic ECG is challenging, especially when patients are not directly referred by the ED. Thus, the patient is frequently seen in the specialist clinic without the required diagnostic information, mandating a request to the ED for the ECG and a second clinic appointment. Giving the patient their ECG often solves this problem because they might remember to bring a copy with them; therefore, this has become one of the recommendations of the NSF (chapter 8).
It was difficult to establish the reason for admission and, in some cases, it would seem inevitable that this was appropriate, for example if a concomitant medical condition was identified but not recorded in the notes. Although the majority (65%) of patients had a TFT done as per NSF guidelines, the large number of 24-h tapes requested for diagnostic purposes alone represents an unnecessary expenditure of £1,500 in addition to costs of hospital admission.
NSF recommends catheter ablation as the treatment of choice for recurrent SVT.6 The low rate of direct referral (34%) could be explained by primary care trust policies, which in recent years have tried to discourage interhospital referral of patients. Of those not referred, most had no further follow up (n=44). The remaining patients were asked to get their GPs to refer them (n=32), of whom nine were referred to a heart rhythm clinic. This resulted in patients attending the ED on multiple occasions (eight patients attended the ED on more than one occasion) before definitive treatment was offered. We also found that referral rates were unsurprisingly better in patients who had a past history of SVT. There are no data to guide us as to whether it is appropriate for patients to have catheter ablation after a single admission to the ED with SVT, but referral is still appropriate to enable the patient to receive an explanation of the condition and the treatment options available.
Although a potential limitation of our study is that we rely on accurate clinical documentation, it indicates that there is a clear need for improvement in the implementation of NSF guidelines for patients attending the ED with regular SVT. This would improve the quality of patient care and minimise healthcare costs. To facilitate this, we have formulated a standard operating procedure, which is available via the College of Emergency Medicine website.7
References
- 1.Josephson M, Buxton A, Marchlinski F. The tachyarrhythmias. In: Isselbacher K, Braunwald E, Wilson JD, et al. (eds), Harrison's Principles of Internal Medicine, 13th edn. New York: McGraw-Hill, 1994: 1024–9. [Google Scholar]
- 2.Zipes D. Specific arrhythmias: diagnosis and treatment. In: Braunwald E. (ed), Heart Disease: A Textbook of Cardiovascular Medicine, 4th edn. Philadelphia: Saunders, 1992: 688–93. [Google Scholar]
- 3.Akhtar M, Jazayeri M, Sra J, et al. Atrioventricular node reentry: clinical, electrophysiological and therapeutic considerations. Circulation 1993; 88: 282–95. [DOI] [PubMed] [Google Scholar]
- 4.Manfreda J, Cuddy TE, Tate RB, et al. Regular narrow QRS complex tachycardias in the Manitoba Follow-up Study (1948–88). Can J Cardiol 1992; 8: 195–9. [PubMed] [Google Scholar]
- 5.Orejarena LA, Vidaillet H, Jr, DeStefano F, et al. Paroxysmal supraventricular tachycardia in the general population. J Am Coll Cardiol 1998; 31: 150–7. 10.1016/S0735-1097(97)00422-1 [DOI] [PubMed] [Google Scholar]
- 6.The National Archives. Coronary heart disease, 2010. www.dh.gov.uk/en/Policyandguidance/Healthandsocialcaretopics/Coronaryheartdisease/DH_4117048 [Accessed 29 January 2013].
- 7.The College of Emergency Medicine, 2013. www.collemergencymed.ac.uk [Accessed 29 January 2013].