Abstract
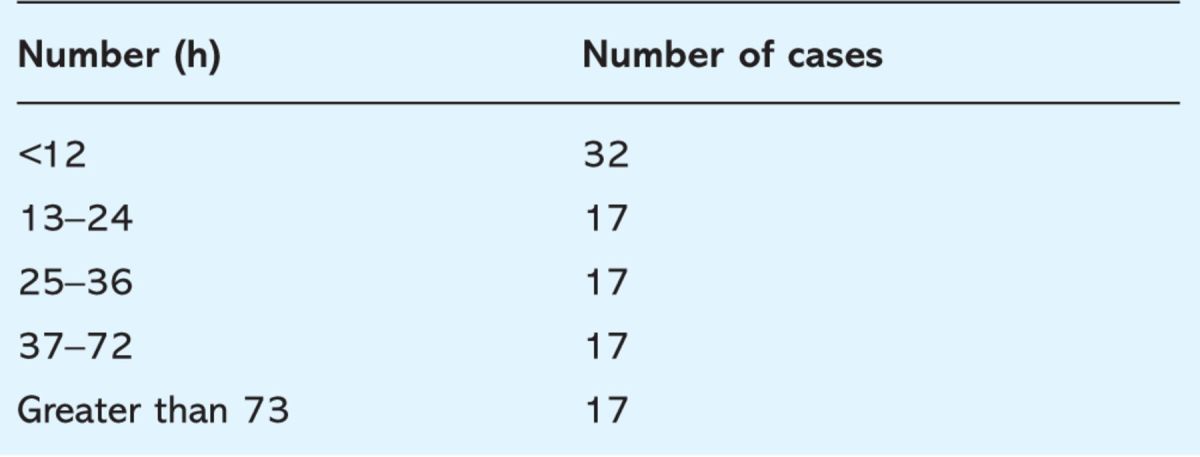
Studies have shown that end-of-life care within the UK hospital setting is variable, and care pathways are now being advocated in the UK. This report presents results from an audit revealing that it is possible to anticipate a large proportion of deaths within an acute setting, but this is generally achieved very close to the end of life. Forty-nine per cent of patients were recognised as dying 24 hours or less before death, 17% between 24 and 36 hours before death, 21% between 36 and 72 hours before death, and 13% greater than 72 hours before death. It discusses the challenges around making the ‘diagnosis of dying’ and highlights that if clinicians do not feel confident in performing such a diagnosis, then patients cannot benefit from end-of-life care pathways. Instead of asking healthcare professionals to make accurate prognoses or diagnose dying, an environment needs to be created where teams feel comfortable in actively managing patients (appropriately) alongside considering their symptom control and planning for possible end-of-life care.
Key Words: care of the dying, diagnosis of dying, end-of-life care pathways, prognostication
Background
Studies have highlighted the variability in the care received by patients at the end of life within the healthcare setting, and although there are government initiatives to enable patients to die in the place of their choice, more than 50% of the UK population dies in hospital.1,2 The Liverpool Care Pathway for the Care of the Dying (LCP) has been developed to try to foster the hospice approach in caring for the dying in other settings and is being rolled out nationally as a template for end-of-life care. However, patients can only benefit from such pathways if clinicians are able to recognise those patients that are dying and feel confident to ‘diagnose’ it.
An audit of end-of-life care was performed in an acute hospital trust that has approximately 1,500 deaths a year. End-of-life care pathways for the dying have not yet been implemented in the trust. This retrospective case-note baseline audit included almost all specialties and aimed to establish:
whether deaths that occurred could have been anticipated
whether a diagnosis of dying, and the timing of this decision in relation to death, had been documented in the notes
the level of documentation of the care received by patients, using guidelines set out in the LCP.
The results of the first and second parts of the audit are presented in this paper as there is a paucity of literature about the anticipation, documentation and timing of the diagnosis of dying in relation to death.
Methods
The notes of patients that had died between 1 January and 31 March 2007 were reviewed. While it was recognised that it is not possible to anticipate every death, the aim was to identify 100 deaths that could have been anticipated according to the information recorded in the notes. Obviously, sudden deaths do occur and some patients should receive full active medical management until death.
Notes were selected randomly by the audit department and screened by two senior members of the team to determine whether the death could have been anticipated within four hours of death. This judgement was made by looking at the documentation by the medical team caring for the patient or by the audit team using the LCP criteria suggested to help diagnose dying (two of the following criteria – bed bound, semi-comatose, unable to take tablets, unable to take fluids). To ensure validity, a senior palliative medicine consultant reviewed one in every four decisions about the diagnosis of dying. Medical and nursing notes and drug and observation charts were reviewed against the guidelines set out by the LCP.
Results
There were 435 deaths during the audit period. Of those, 154 sets of notes were screened to identify 100 deaths that could have been anticipated. Of the 54 deaths that were judged to be unlikely, 36 patients had an acute deterioration or cardiac arrest, six were appropriately actively managed until death and in 12 sets of notes the documentation was too poor to determine if the death could have been anticipated or not.
Of the deaths that were judged could have been anticipated, there was documentation to suggest that the patient was dying in 93/100 medical notes; using terms such as ‘for best supportive care’, ‘TLC’ (tender loving care) or ‘comfort care only’. In 7/100 patients, the fact the patient was dying was not recognised or documented by the medical team. Of the 100 deaths, 70% occurred on medical wards, 24% on surgical wards and 6% on the intensive care unit. Table 1 shows the patient demographics for those deaths that could have been anticipated. Table 2 shows the timings from admission to death and Table 3 shows the timings from anticipation of death by the medical team to death.
Table 1.
Basic demographics.
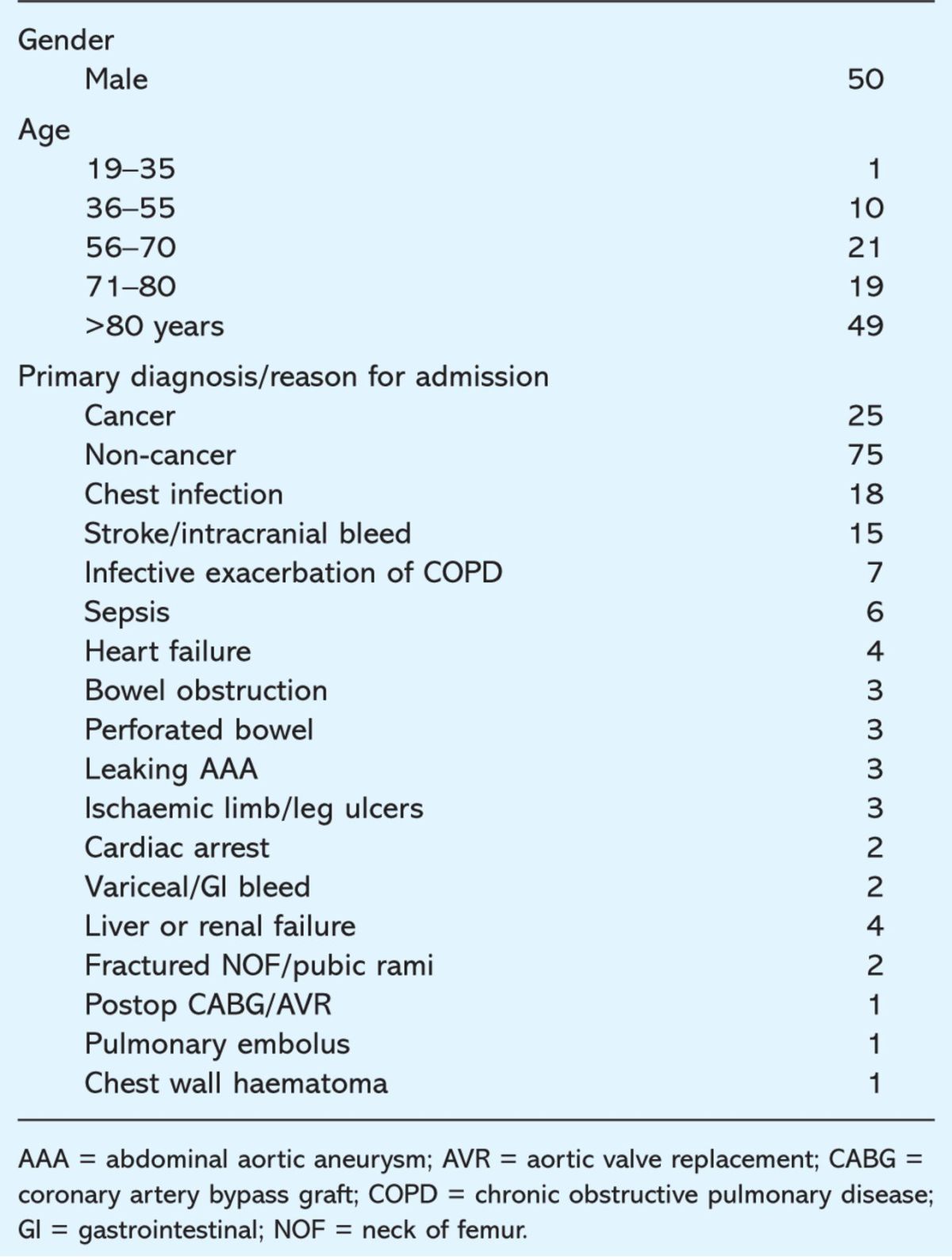
Table 2.
Timing from admission to death. Range 4 hours to 108 days.
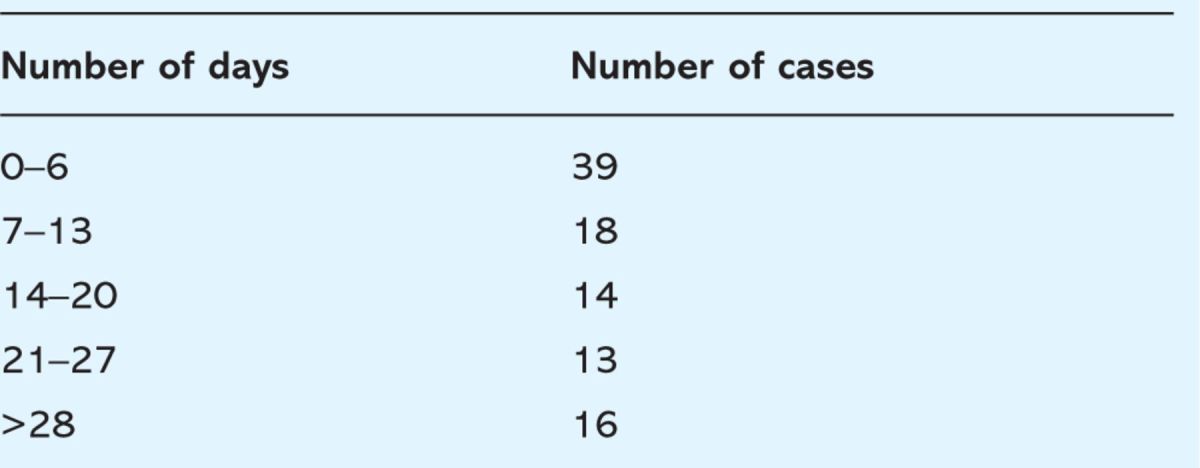
Table 3.
Timing of anticipation of dying to death. Range 4 to 404 hours (16.5 days).
Discussion
The findings
This audit has revealed that in the acute hospital setting, two thirds of all deaths can be anticipated at least four hours before the death occurs (100/154). However, the length of time from recognition of dying to death is short; 87% of patients are recognised as dying less than 72 hours before death.
Limitations
This was a retrospective audit as it was known that the patients had died and so an attempt to make fair decisions in determining whether the death could have been anticipated or not was made. Some would argue that the minimum four-hour period between the diagnosis of dying and death for inclusion in this audit was too short. This window was chosen because in four hours measures can be undertaken to change patient care meaningfully, and it also coincides with the timing of nursing observations. This audit did not look at patients who were thought to be dying, but subsequently improved, as the methods did not allow data capture about these patients. A prospective study of deaths in an acute trust that will include these patients is, however, currently being performed.
Links with existing knowledge – timing of diagnosis of dying in relation to death
Reports have shown that half of all deaths in the UK can be anticipated.3 In one study, recognising that elderly care patients were close to death occurred most frequently between 24 and 48 hours prior to death.4 A case-note audit on the implementation of the LCP showed the average length of time on a care of the dying pathway was 33 hours.5 Of deaths, 75% were highly or moderately expected by the nursing staff on general hospital wards in Italy when asked the question, ‘Had somebody told you yesterday that the patient would have died within a day how far would you have agreed?’6 The findings in this paper are consistent with these studies; clinicians do make the diagnosis of dying, but this occurs very close to death.
Links with existing knowledge – the challenges of diagnosing dying
Studies have highlighted that healthcare professionals have difficulty in making accurate prognostic predictions in patients with malignant and non-malignant disease, and that it can be difficult to diagnose dying.7–11 Doctors' estimates of prognosis in terminally ill patients with cancer are usually overoptimistic.7 Why is it so difficult and can we do better? Diagnosing dying is a complex process including patient, healthcare professional and institutional factors. Patients with chronic non-cancer diseases, for example, can come close to death on several occasions before they die, making it difficult for healthcare professionals to determine which will be their last episode.9 In addition, patients and their families have very individual and changing needs with regard to knowing and accepting a prognosis,12 yet up to one fifth of patients with a non-cancer diagnosis in the last year of their life are reported to suspect that they are dying.13 Qualitative interviews with terminally ill cancer patients show that people who are dying want to understand what is happening to them and can cope with this information.14 Focus groups of patients with advanced chronic illness, their families and healthcare professionals reveal they all agree that preparation for death is important for patients as many wanted to make funeral plans and know the timing of death.10
Links with existing knowledge – the role of healthcare professionals
Most healthcare professionals have little formal training in diagnosing dying and although most patients die within the hospital setting, looking after dying patients remains a small proportion of an individual clinician's workload.8 Healthcare professionals can be reluctant to diagnose dying if there is any hope of cure and death is often deemed as a failure.16 Qualitative interviews have revealed that some specialist clinicians, despite being sensitive and caring, express reluctance to face the palliative care needs of their patients and find it difficult to discuss prognostication and end-of-life issues with patients.8,17
Studies suggest that the culture of large hospitals remains that the focus of care is cure; life prolongation and continuation of invasive procedures, investigations and treatments are often continued at the expense of comfort for the patient.1,15 The acceptance of dying and the transition to end-of-life care can be difficult.1 There is an abundance of literature to suggest that the palliative care approach should be fully integrated into the hospital setting.17,18 Although advances have been made over the past few decades, the ability to judge prognosis has not changed during this time8; research tools are emerging to predict short-term survival and these have been investigated in the acute hospital setting but further work is needed before these can be used routinely in clinical practice.19,20
Implications for practice
It is clear that healthcare professionals do not find it easy to diagnose dying and this is perhaps reflected in the recent national end-of-life care audit results; in institutions where the LCP had been rolled out, only 15% of patients who had died were placed on the pathway.21 Instead of asking healthcare professionals to make accurate prognoses or diagnose dying, an environment needs to be created where teams feel comfortable in actively medically managing patients (appropriately) alongside considering their symptom control and planning for possible end-of-life care. Posing the question, ‘Would you be surprised if this patient died on this admission?’ to teams caring for patients is the first step, however, this would require considerable time and skills to be introduced properly.
Summary
It is possible to anticipate a large proportion of deaths within the acute hospital setting, however, this is generally achieved very close to death. End-of-life care pathways for the dying are being advocated by the Department of Health, but if clinicians do not feel confident in ‘diagnosing dying’, then patients cannot benefit from such pathways. The first step is to assist clinicians in identifying those patients who might die during their current hospital admission, thereby enabling active treatment, where appropriate, alongside symptom relief and advance care planning for the future.
Reference
- 1. SUPPORT Principle Investigators. A controlled trial to improve care for seriously ill hospitalised patients: the study to understand prognoses and preferences for outcomes and risks of treatment. JAMA 1995; 274:1591–8. 10.1001/jama.1995.03530200027032 [DOI] [PubMed] [Google Scholar]
- 2. Edmonds P, Rogers A. ‘If only someone had told me’; A review of the care of patients dying in hospital. Clin Med 2003; 3:149–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Council for Hospice and Specialist Palliative Care Services. A statement of definitions. Occasional paper Number 8. London: National Council for Hospice and Specialist Palliative Care Services, 1995. [Google Scholar]
- 4. Twomey F, McDowell D, Corcoran G. End of life care for older patients dying in an acute general hospital – can we do better? Age Ageing 2007: 12;462–4. [DOI] [PubMed] [Google Scholar]
- 5. Mirando S, Davies P, Lipp A. Introducing an integrated care pathway for the last days of life. Palliat Med 2005; 19:33–9. 10.1191/0269216305pm960oa [DOI] [PubMed] [Google Scholar]
- 6. Toscani F, Di Giulio P, Brunelli C, Miccinesi G, Laquintanaa D. How people die in hospital general wards: a descriptive study. J Pain Symptom Manage 2005; 30:33–40. 10.1016/j.jpainsymman.2005.01.013 [DOI] [PubMed] [Google Scholar]
- 7. Christakis N, Lamont E. Extent and determinants of error in doctors' prognoses in terminally ill patients: a prospective cohort study. BMJ 2000; 320:469–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Christakis N, Iwashyna T. Attitude and self-reported practice regarding prognostication in national sample of internists. Arch Intern Med 1998; 158:2389–95. 10.1001/archinte.158.21.2389 [DOI] [PubMed] [Google Scholar]
- 9. Coventry P, Grande G, Richards D, Todd C. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing 2005; 34:218–27. 10.1093/ageing/afi054 [DOI] [PubMed] [Google Scholar]
- 10. Steinhauser K, Christakis N, Clipp E. et al Preparing for the end of life; preference of patients, families, physicians and other care providers. J Pain Symptom Manage 2001; 22:727–37. [DOI] [PubMed] [Google Scholar]
- 11. Higgs R. The diagnosis of dying. J R Coll Physicians Lond 2000; 33:110–2. [PMC free article] [PubMed] [Google Scholar]
- 12. Higginson I, Priest P, McCarthy M. Are bereaved family members a valid proxy for a patient's assessment of dying? Soc Sci Med 1994; 38:553–7. [DOI] [PubMed] [Google Scholar]
- 13. Hinton J. How reliable are relatives' reports of terminal illness? Patients and relatives accounts compared. Soc Sci Med 1996; 43:1229–36. [DOI] [PubMed] [Google Scholar]
- 14. Barnett M. Does it hurt to know the worst? Psychological morbidity, information preferences and understanding of prognosis in patients with advanced cancer. Psychooncology 2006; 15:44–55 10.1002/pon.921 [DOI] [PubMed] [Google Scholar]
- 15. Ellershaw J, Ward C. Care of the dying patient: the last hours or days of life. BMJ 2003; 326:30–4. 10.1136/bmj.326.7379.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Miller F, Fins J. A proposal to restructure hospital care for dying patients. N Engl J Med 1996; 334:1740–2 10.1056/NEJM199606273342612 [DOI] [PubMed] [Google Scholar]
- 17. Fitzsimons D, Mullan D, Wilson J. et al The challenge of patients' unmet palliative care needs in the final stages of chronic disease. Palliat Med 2007; 21:313–22. [DOI] [PubMed] [Google Scholar]
- 18. Lynn J. Learning to care for people with chronic illness facing the end of life. JAMA 2000; 284:2508–11. 10.1001/jama.284.19.2508 [DOI] [PubMed] [Google Scholar]
- 19. Pirvano M, Maltoni M, Nanni O. et al A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. J Pain Symptom Manage 1999; 17:231–9. [DOI] [PubMed] [Google Scholar]
- 20. Olajide O, Hanson L, Usher B. et al Validation of the palliative performance scale in the acute tertiary care hospital setting. J Palliat Med 2007; 10:111–7. 10.1089/jpm.2006.0125 [DOI] [PubMed] [Google Scholar]
- 21. The Marie Curie Palliative Care Institute Liverpool. National care of the dying audit-hospitals. Generic report 2006/2007. London: RCP, 2007. www.rcplondon.ac.uk/college/ceeu/NCDAH/NCDAH-Generic-Report.pdf (accessed 20 December 2007). [Google Scholar]


