The ability to support patients with chronic respiratory failure (CRF) in the home has been one of the major advances of respiratory medicine. The delivery of ventilatory support has progressed from negative pressure devices, introduced as a consequence of the poliomyelitis epidemics in the 1940s and 1950s, through ventilation via tracheostomy to non-invasive ventilation (NIV) via face or nasal masks. NIV has expanded from its initial role within the intensive care unit to the respiratory ward and subsequently to the home setting. The provision for home mechanical ventilation (HMV) in the UK has expanded but the clinical benefit to differing diagnostic groups is far from clear. Clinical practice is based on a combination of physiological studies, randomised controlled trials (RCT) and clinical experience.
Obstructive lung disease
The evidence for using NIV for the management of acute hypercapnic respiratory failure (AHRF) in patients with chronic obstructive pulmonary disease (COPD) is established in both the critical care and ward setting,1,2 but the evidence for HMV is controversial. There is evidence that long-term oxygen therapy (LTOT) improves survival in patients with severe COPD,3,4 but fails to improve nocturnal hypoventilation and is required for more than 15 hours a day. In addition, sleep disordered breathing, prevalent in COPD patients,5 contributes to morbidity so a rationale to use nocturnal NIV to manage CRF is appropriate. Three physiological mechanisms of action for NIV have been proposed:
improved hypercapnic ventilatory response (HCVR)
enhanced pulmonary mechanics
increased respiratory muscle strength (RMS).
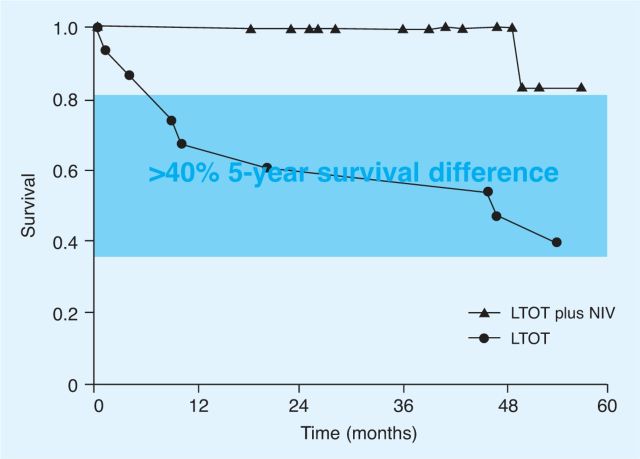
These mechanisms were investigated by Nickol et al6 in COPD patients using HMV for three months. The study confirmed the improvement in arterial blood gas parameters shown previously and investigated these mechanisms in detail. HCVR is a simple test measuring changes in ventilation in response to breathing carbon dioxide (CO2): the relationship between changes in ventilation and CO2 reflects central chemoreceptor sensitivity. There was an increased HCVR at five days but no further increase at three months, highlighting the importance of ensuring an adequate initial set up of HMV in these patients (Fig 1). Hyperinflation was reduced over the course of the intervention, indicating enhanced pulmonary mechanics. RMS was unchanged.
Fig. 1.
Effect of non-invasive ventilation (NIV) on arterial blood gases and hypercapnia ventilatory response (HCVR) in chronic obstructive pulmonary disease (COPD). Mean (SEM) PaCO2, PaO2 and HCVR at days 0 (D0) and 5 (D5) and three months (3M) are shown.
There was a significant fall in PaCO2 (p=0.001) and rise in PaO2 (p=0.004). There was a significant increase in HCVR from baseline to D5 (p=0.009).6 SEM = standard error of mean; PaCO2 = arterial carbon dioxide tension; PaO2 = arterial oxygen tension.
Despite a paucity of RCT evidence in support, these and other physiological data have directed clinicians to use HMV for COPD patients with CRF, in particular those with frequent admissions with AHRF. An early double-blind RCT conducted using negative pressure ventilation showed no differences in any of the clinical and physiological outcome variables measured.7 However, as with a number of the subsequent studies using positive pressure ventilation, there was a high rate of non-compliance; thus this study can be criticised for only demonstrating that domiciliary negative pressure ventilation has limited feasibility in the home setting. There has been improved tolerance with positive pressure NIV but all the RCTs to date are limited by poor study design.
The most common critique of the current evidence is that the trials used suboptimal inspiratory pressures and therefore failed to ventilate patients effectively.8 Other trials had poor ventilator compliance or did not select patients with CRF (which seems counterintuitive). Clini et al 9 assessed performance of NIV against LTOT in a multicentre RCT in hypercapnic patients. A small improvement in gas exchange and health-related quality of life (HRQL) was demonstrated, but without hospitalisation or mortality benefit. The NIV settings were titrated to comfort with inspiratory pressures that would be considered low in comparison with today's clinical practice. Furthermore, the patients selected would now be classified as severe ‘end-stage’ disease. Positive outcomes were shown in a randomised crossover trial with hypercapnic COPD patients treated for three months with LTOT alone or plus HMV.10 The latter group showed improved gas exchange, sleep quality and exercise capacity.10 Further RCTs are required focusing on optimisation of ventilator settings and patient compliance to clarify the role of HMV in COPD patients with CRF.
Restrictive lung disease
The demographics of HMV users with restrictive lung disease are changing. The original indication was related to the sequelae of poliomyelitis epidemics as well as post-tuberculosis chest wall disease. These diseases are decreasing but, although other neuromuscular disorders (eg motor neuron disease and Duchenne muscular dystrophy) are increasingly treated with HMV, there has been a significant rise in obesity hypoventilation syndrome (OHS).11
Neuromuscular disease
Early studies showed that the cause of death in most patients with progressive neuromuscular disease was respiratory failure,12 identifying HMV as a potential useful treatment in patients such as those with Duchenne muscular dystrophy and motor neuron disease. The physiological data investigating the modes of action showed improved gas exchange and Epworth Sleepiness Score at three months.13 As with COPD, the mechanism of action was associated with improvements in HCVR, with limited changes in pulmonary mechanics and RMS.13 In addition, a dose-response effect of NIV on arterial CO2 (PaCO2) was demonstrated, supporting a true treatment effect.13
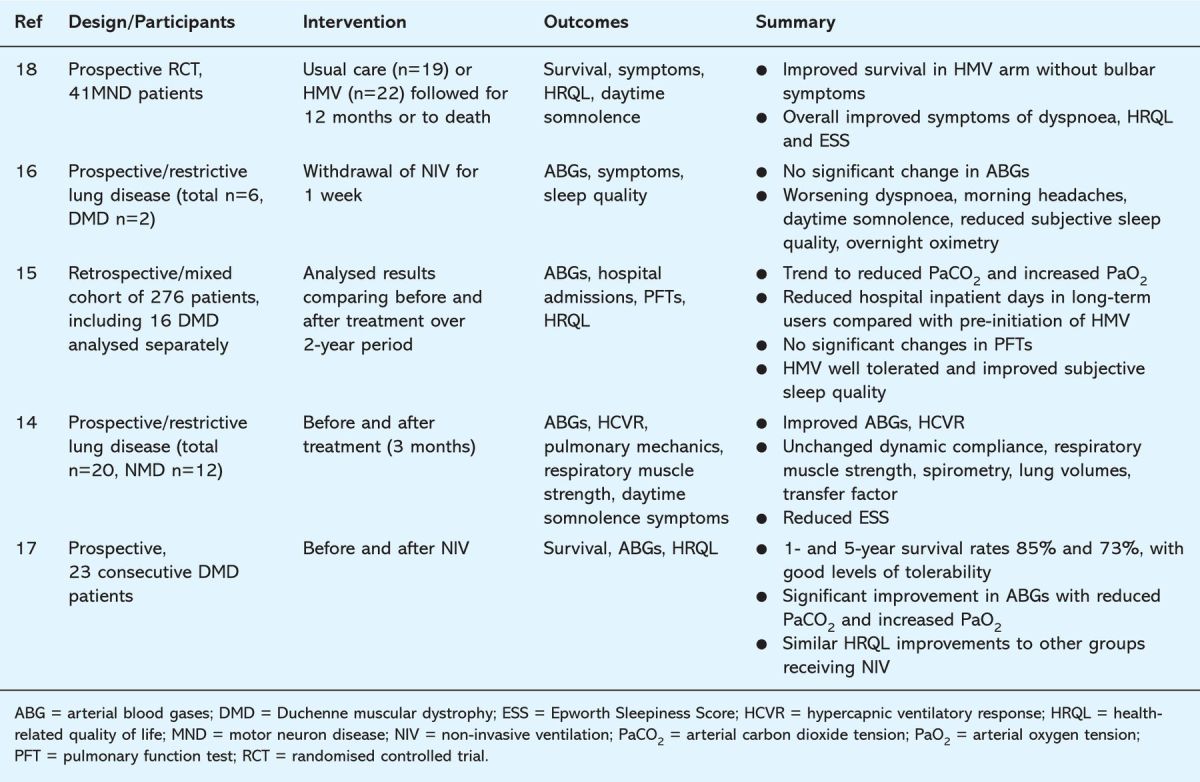
Initial data from observational trials showed HMV was associated with improved HRQL, fewer inpatient hospital days and improved survival (Table 1).14–16 However, these results should be interpreted with caution as no control or sham groups were used, the comparisons being made with historical data or with patients who failed to tolerate NIV.
Table 1.
Summary of outcome data for trials involving home mechanical ventilation (HMV) in patients with neuromuscular disease (NMD)
Key Points.
Home mechanical ventilation (HMV) can effectively be used to manage chronic respiratory failure in both restrictive and obstructive lung disease
The patient demographics have changed over time with chronic obstructive pulmonary disease (COPD) and obesity-related respiratory failure (ORRF) accounting for the majority of patients currently initiated
Well designed randomised controlled trials are required to demonstrate clinical effectiveness of HMV for COPD and ORRF
To investigate the effect of HMV on survival and HRQL, Bourke et al17 performed an RCT of patients with motor neuron disease randomised to receive NIV or standard care. Criteria for initiation of HMV were symptomatic hypercapnia or orthopnoea with a maximum inspiratory pressure below 60% predicted. The patients were followed up for 12 months or until death. HMV improved HRQL and survival in all patients; in particular, the subgroup with better bulbar function had a median survival benefit of 205 days with maintained HRQL. HMV also improved HRQL in those with poor bulbar function but without any survival benefit.
These data have been used to support the provision of HMV in neuromuscular disease but the optimum timing for initiation of ventilation has not yet been established. Most trials used symptomatic daytime hypercapnia or evidence of profound respiratory muscle weakness as markers for initiation. One multicentre RCT18 showed that early intervention in Duchenne muscular dystrophy prior to the development of CRF showed no benefit in delaying progression to ventilatory failure, and alarmingly demonstrated higher mortality in the HMV arm.
A more structured approach was adopted in a study of neuromuscular disease and chest wall disease patients with daytime normocapnia but nocturnal hypoventilation, randomising them to either early or delayed treatment.19 Within 24 months, 90% of patients required initiation of HMV, 70% within the first 12 months. The earlier initiation of HMV to reduce risk of acute decompensation needs to be balanced against its inconvenience.
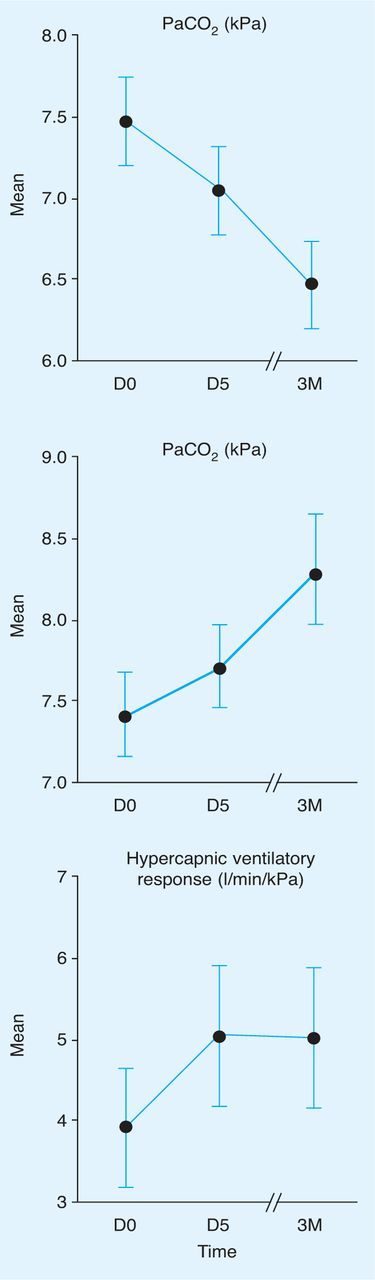
Chest wall disease
Many of the studies of patients with neuromuscular disease include patients with chest wall disease. Data from small retrospective studies or uncontrolled trials show improvement in gas exchange.20 Again, like other groups, these patients have an improvement in HCVR.13,20 Survival data from observational cohorts show a survival advantage with HMV over standard care with oxygen (Fig 2).13,21
Fig. 2.
Survival curves of kyphoscoliotic patients treated with long-term oxygen therapy (LTOT) or LTOT plus non-invasive ventilation (NIV).
Obesity hypoventilation syndrome
The obesity epidemic has driven obesity-related respiratory problems. Obstructive sleep apnoea has a standard diagnostic and treatment algorithm but OHS, despite its high mortality, is underdiagnosed with limited understanding of the pathophysiology of CRF.22 The diagnosis of OHS is an overlap of obesity (body mass index (BMI) ≥30 kg/m2), daytime hypercapnia (PaCO2 >6 kPa) and sleep-disordered breathing. The population prevalence is unknown but it is more common with increasing BMI, occurring in approximately 25% of patients with a BMI over 40.23
Nowbar et al22 showed that survival rates are poor without NIV (as with other areas of HMV), but there are no RCTs of treatment with NIV compared with sham or standard care. The only prospective RCT compared NIV with continuous positive airways pressure (CPAP) in a highly selected subset of OHS patients without severe nocturnal hypoventilation. Not unsurprisingly, this study showed no advantage of NIV over CPAP.24 A number of studies have demonstrated improvement in physiological parameters, including gas exchange, sleep quality, daytime vigilance and HRQL.24 Again, NIV improves the HCVR.25
Conclusions
Current practice is to start HMV for stable hypercapnic COPD patients who have recurrent admissions with AHRF requiring NIV and for symptomatic neuromuscular, chest wall deformity and OHS patients. Future trials need to have an emphasis on COPD and OHS patients, for whom physiological improvements have not been substantiated, by well designed RCTs demonstrating clinical effectiveness in terms of improving HRQL, exercise capacity and survival.
Reference
- 1. Plant PK, Owen JL, Elliott MW. Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet 2000; 355:193–15. 10.1016/S0140-6736(00)02323-0 [DOI] [PubMed] [Google Scholar]
- 2. Brochard L, Mancebo J, Wysocki M. et al Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995; 333:817–22. 10.1056/NEJM199509283331301 [DOI] [PubMed] [Google Scholar]
- 3. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Party. Lancet 1981;i:681–6. [PubMed] [Google Scholar]
- 4. Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med 1980; 93:391–8. [DOI] [PubMed] [Google Scholar]
- 5. Arand DL, McGinty DJ, Littner MR. Respiratory patterns associated with haemoglobin desaturation during sleep in chronic obstructive pulmonary disease. Chest 1981; 80:183–90. 10.1378/chest.80.2.183 [DOI] [PubMed] [Google Scholar]
- 6. Nickol AH, Hart N, Hopkinson NS. et al Mechanisms of improvement of respiratory failure in patients with COPD treated with NIV. Int J Chron Obstruct Pulmon Dis 2008; 3:453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shapiro SH, Ernst P, Gray-Donald K. et al Effect of negative pressure ventilation in severe chronic obstructive pulmonary disease. Lancet 1992; 340:1425–9. [DOI] [PubMed] [Google Scholar]
- 8. Casanova C, Celli BR, Tost L. et al Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest 2000; 118:1582–90. 10.1378/chest.118.6.1582 [DOI] [PubMed] [Google Scholar]
- 9. Clini E, Sturani C, Rossi A. et al The Italian multicentre study on noninvasive ventilation in chronic obstructive pulmonary disease patients. Eur Respir J 2002; 20:529–38. 10.1183/09031936.02.02162001 [DOI] [PubMed] [Google Scholar]
- 10. Meecham Jones DJ, Paul EA, Jones PW, Wedzicha JA. Nasal pressure support ventilation plus oxygen compared with oxygen therapy alone in hypercapnic COPD. Am J Respir Crit Care Med 1995; 152:538–44. [DOI] [PubMed] [Google Scholar]
- 11. Janssens JP, Derivaz S, Breitenstein E. et al Changing patterns in long-term noninvasive ventilation: a 7-year prospective study in the Geneva Lake area. Chest 2003; 123:67–79. 10.1378/chest.123.1.67 [DOI] [PubMed] [Google Scholar]
- 12. Rideau Y, Gatin G, Bach J, Gines G. Prolongation of life in Duchenne's muscular dystrophy. Acta Neurol (Napoli) 1983; 5:118–24. [PubMed] [Google Scholar]
- 13. Nickol AH, Hart N, Hopkinson NS. et al Mechanisms of improvement of respiratory failure in patients with restrictive thoracic disease treated with non-invasive ventilation. Thorax 2005; 60:754–60. 10.1136/thx.2004.039388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Leger P, Bedicam JM, Cornette A. et al Nasal intermittent positive pressure ventilation. Long-term follow-up in patients with severe chronic respiratory insufficiency. Chest 1994; 105:100–5. 10.1378/chest.105.1.100 [DOI] [PubMed] [Google Scholar]
- 15. Hill NS, Eveloff SE, Carlisle CC, Goff SG. Efficacy of nocturnal nasal ventilation in patients with restrictive thoracic disease. Am Rev Respir Dis 1992;145(2 Pt 1)365–71. [DOI] [PubMed] [Google Scholar]
- 16. Simonds AK, Muntoni F, Heather S, Fielding S. Impact of nasal ventilation on survival in Duchenne muscular dystrophy. Thorax 1998; 53:949–52. 10.1136/thx.53.11.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bourke SC, Tomlinson M, Williams TL. et al Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 2006; 5:140–7. 10.1016/S1474-4422(05)70326-4 [DOI] [PubMed] [Google Scholar]
- 18. Raphaël JC, Chevret S, Chastang C, Bouvet F. Randomised trial of preventive nasal ventilation in Duchenne muscular dystrophy. French Multicentre Cooperative Group on Home Mechanical Ventilation Assistance in Duchenne de Boulogne Muscular Dystrophy. Lancet 1994; 343:1600–4. [DOI] [PubMed] [Google Scholar]
- 19. Ward S, Chatwin M, Heather S, Simonds AK. Randomised controlled trial of non-invasive ventilation (NIV) for nocturnal hypoventilation in neuromuscular and chest wall disease patients with daytime normocapnia. Thorax 2005; 60:1019–24. 10.1136/thx.2004.037424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Buyse B, Meersseman W, Demedts M. Treatment of chronic respiratory failure in kyphoscoliosis: oxygen or ventilation? Eur Respir J 2003; 22:525–8. 10.1183/09031936.03.00076103 [DOI] [PubMed] [Google Scholar]
- 21. Jäger L, Franklin KA, Midgren B, Löfdahl K, Ström J. Increased survival with mechanical ventilation in posttuberculosis patients with the combination of respiratory failure and chest wall deformity. Chest 2008; 133:156–60. [DOI] [PubMed] [Google Scholar]
- 22. Nowbar S, Burkart KM, Gonzales R. et al Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. Am J Med 2004; 116:1–7. 10.1016/j.amjmed.2003.08.022 [DOI] [PubMed] [Google Scholar]
- 23. Mokhlesi B, Kryger MH, Grunstein RR. Assessment and management of patients with obesity hypoventilation syndrome. Proc Am Thorac Soc 2008; 5:218–25. 10.1513/pats.200708-122MG [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Piper AJ, Wang D, Yee BJ, Barnes DJ, Grunstein RR. Randomised trial of CPAP v bilevel support in the treatment of obesity hypoventilation syndrome without severe nocturnal desaturation. Thorax 2008; 63:395–401. [DOI] [PubMed] [Google Scholar]
- 25. Redolfi S, Corda L, La Piana G. et al Long-term non-invasive ventilation increases chemosensitivity and leptin in obesity-hypoventilation syndrome. Respir Med 2007; 101:1191–5. 10.1016/j.rmed.2006.11.005 [DOI] [PubMed] [Google Scholar]