Abstract
Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction characterised by rapidly developing life-threatening airway, breathing and/or circulation problems usually associated with skin and mucosal changes. Updated guidance on the recognition, acute management and follow up of adults with anaphylaxis has recently been published. This is a concise version of the full guidelines published by the Resuscitation Council (UK) in 2008. The use of an airway, breathing, circulation, disability and exposure approach to recognise and treat anaphylaxis is emphasised.
Key Words: anaphylaxis
Introduction and aims
Anaphylaxis is a severe, life-threatening hypersensitivity reaction which is estimated to affect approximately 1 in 1,333 of the English population at some point in their lives. The incidence of anaphylaxis is increasing and there has been a dramatic growth in the rate of related hospital admissions in the last two decades. Although the overall prognosis of anaphylaxis is good (case-fatality ratio of less than 1%), the risk of death is increased in those with pre-existing asthma. There are approximately 20 deaths due to anaphylaxis reported each year in the UK.
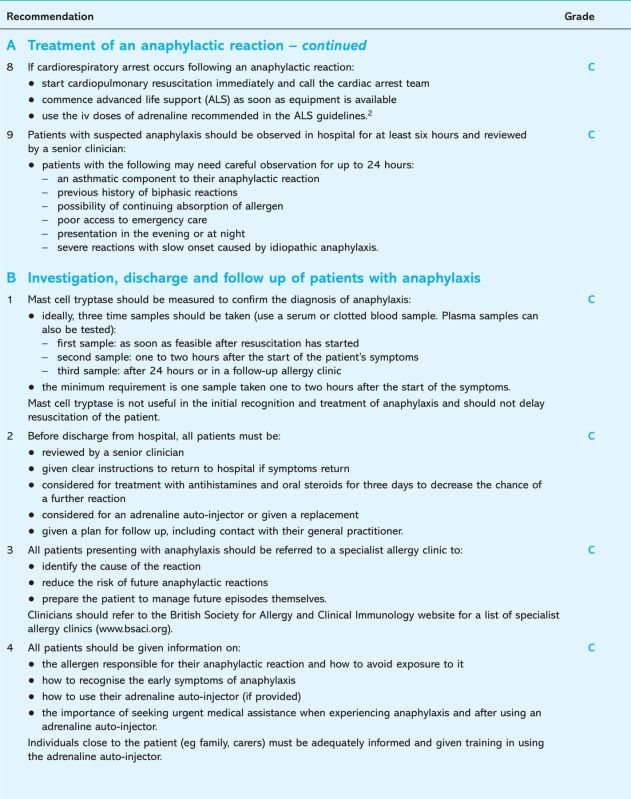
Anaphylaxis can occur following exposure to a very broad range of triggers (Table 1). It has a range of possible presentations and the lack of any consistent clinical manifestations continues to cause diagnostic difficulty. Full guidance for the emergency treatment of anaphylactic reactions has recently been published.1 Information in this concise guidance has been extracted from the full guideline. Please refer to the full guidance for details of methodology.
Table 1.
Allergens known to trigger fatal anaphylactic reactions. For further details, please see the full guidance document.1
The aim of this guidance is to provide updated recommendations in the following areas:
the recognition and correct diagnosis of anaphylaxis
the acute management and effective treatment of an anaphylactic reaction in adults
the appropriate investigation and follow up of patients with suspected anaphylaxis.
Pathophysiological consequences of anaphylaxis
Anaphylaxis can be caused by allergic and non-allergic mechanisms. Allergic anaphylaxis is caused by an immediate (type I) hypersensitivity reaction following exposure to an allergen to which the patient has become sensitised. The allergen stimulates IgE-mediated degranulation of mast cells, releasing large quantities of histamine into the circulation which causes intense smooth muscle contraction, increased vascular permeability and vasodilation. The clinical presentation is the same regardless of whether the reaction has an allergic or non-allergic mechanism.
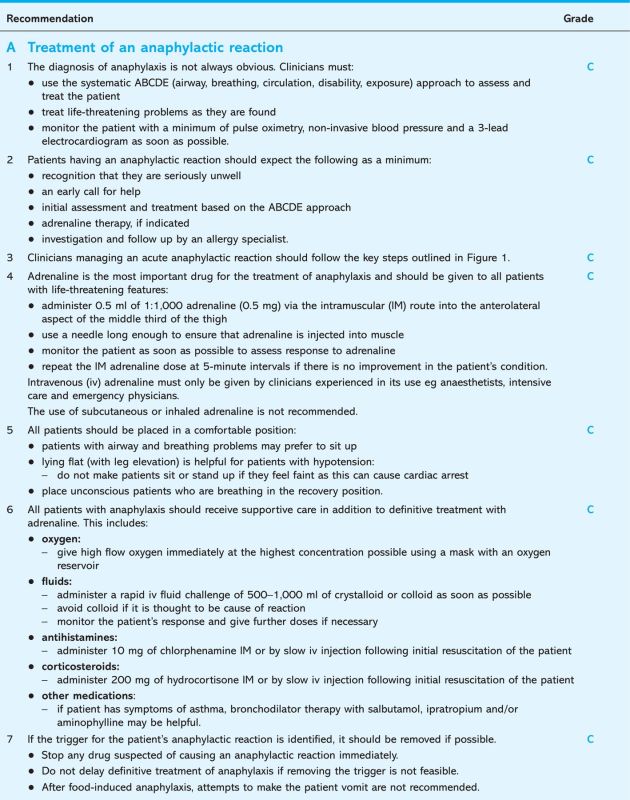
Adrenaline is the most important drug for the treatment of an anaphylactic reaction. Failure to inject adrenaline promptly increases the risk of death. Adverse effects of adrenaline are extremely rare when the correct doses are injected intramuscularly. Intravenous adrenaline has a much greater risk of causing harmful side effects and hence should only be used by those experienced in the use and titration of vasopressors in their normal clinical practice.
Recognition of an anaphylactic reaction
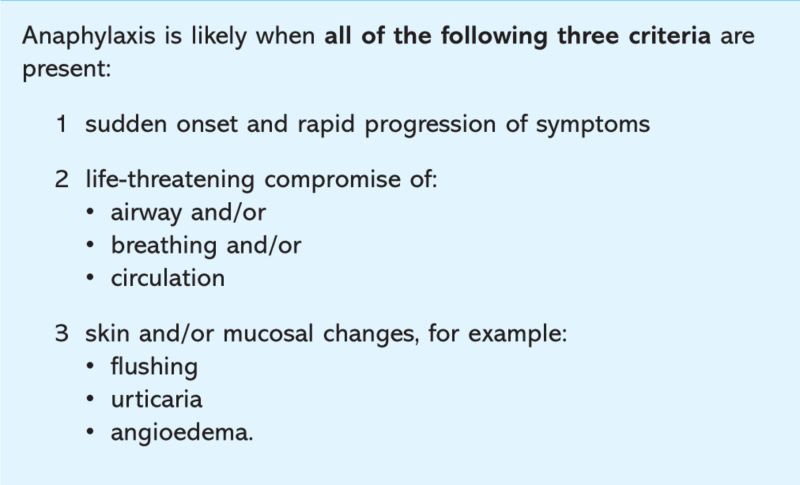
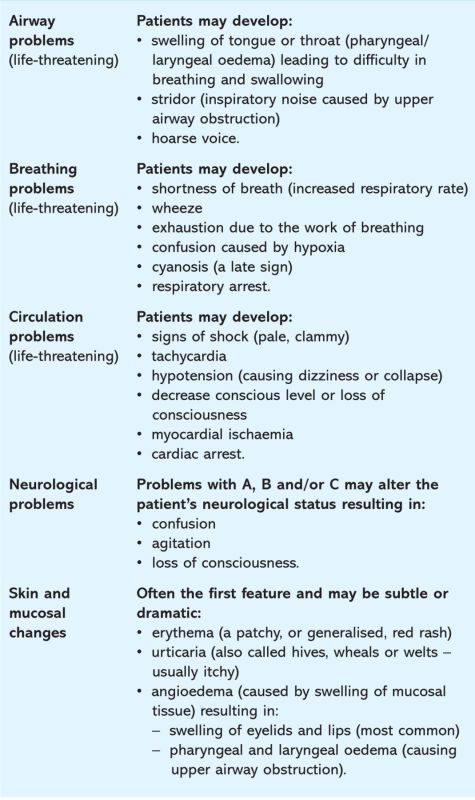
There is a range of signs and symptoms, none of which are entirely specific for anaphylactic reaction, however, certain combinations of signs make the diagnosis more likely (Box 1). Most anaphylactic reactions develop suddenly and evolve rapidly following exposure to a trigger (allergen). There is a rapid progression of symptoms resulting in life-threatening compromise of airway, breathing and/or circulation (Box 2).
Box 1. Recognition of an anaphylactic reaction.
Box 2. Symptoms and signs of anaphylaxis.
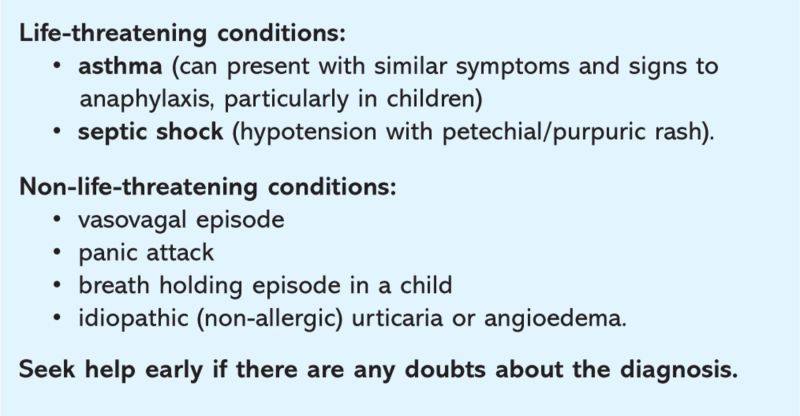
Some patients have less severe systemic allergic reactions that are characterised by skin or mucosal changes alone (eg generalised urticaria or angioedema). These reactions are not described as anaphylaxis because life-threatening features are not present. Most patients who have skin changes caused by allergy do not go on to develop an anaphylactic reaction. The differential diagnosis of anaphylaxis is summarised in Box 3.
Box 3. Differential diagnosis of anaphylaxis.
Implications for implementation
The implications for implementation of these guidelines are primarily those of staff education and awareness. All clinical staff within the hospital setting should be able to call for help and initiate treatment in a patient experiencing an anaphylactic reaction.
Resuscitation equipment and drugs to help with the rapid resuscitation of a patient with anaphylaxis must be immediately available in all clinical settings. No new drugs for the treatment of anaphylaxis are needed. Intramuscular injection of adrenaline is the initial treatment of choice.
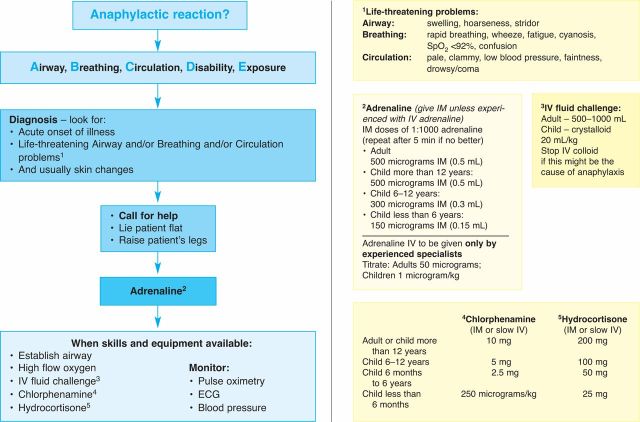
Summary of the guidelines.
Fig. 1.
The anaphylaxis algorithm. Reproduced and modified with permission from the Resuscitation Council (UK). ECG = electrocardiogram; IM = intramuscular; iv = intravenously.
Membership of the Guideline Development Group
Jasmeet Soar, Co-chair Working Group and Vice Chair, Resuscitation Council (UK); Richard Pumphrey, Co-chair Working Group, Royal College of Pathologists; Andrew Cant, Royal College of Paediatrics and Child Health; Sue Clarke, Anaphylaxis Campaign; Allison Corbett, British National Formulary; Peter Dawson, Royal College of Radiologists; Pamela Ewan, British Society for Allergy and Clinical Immunology; Bernard Foëx, College of Emergency Medicine; David Gabbott, Executive Committee Member Resuscitation Council (UK); Matt Griffiths, Royal College of Nursing; Judith Hall, Royal College of Anaesthetists; Nigel Harper, Association of Anaesthetists of Great Britain and Ireland; Fiona Jewkes, Royal College of General Practioners, Joint Royal College Ambulance Liason Committee; Ian Maconochie, Executive Committee Member, Resuscitation Council (UK); Sarah Mitchell, Director, Resuscitation Council UK; Shuaib Nasser, British Society of Allergy and Clinical Immunology; Jerry Nolan, Chair, Resuscitation Council (UK); George Rylance, Royal College of Paediatrics and Child Health; Aziz Sheikh, Resuscitation Countil UK; David Joseph Unsworth, Royal College of Pathologists; David Warrell, Royal College of Physicians.
Reference
- 1. Soar J, Pumphrey R, Cant A. et al Emergency treatment of anaphylactic reactions – guidelines for healthcare providers. Resuscitation 2008; 77:157–69. [DOI] [PubMed] [Google Scholar]
- 2. Resuscitation Council (UK). Adult advanced life support. London: Resuscitation Council (UK), 2005. www.resus.org.uk/pages/als.pdf. [Google Scholar]
Other useful sources of information
- Resuscitation Council (UK): www.resus.org.uk
- British Society for Allergy and Clinical Immunology: www.bsaci.org