ABSTRACT
Rehabilitation following acquired brain injury improves health outcomes, reduces disability, and improves quality of life. We assessed the cost effectiveness of inpatient rehabilitation after brain injury in individuals with brain injury admitted to the Irish national tertiary specialist rehabilitation centre in 2011. Patients’ score on the Disability Rating Scale (DRS) was recorded on admission and at discharge after intensive inpatient rehabilitation. Cost savings attributed to the rehabilitation programme were calculated as the difference between direct care costs on admission and discharge. Direct costs of care were calculated as the weekly cost of the care-assistant hours required to care for patients on the basis of their level of disability or daily nursing-home bed cost when this was required. Of 63 patients, complete DRS information for admission and discharge was available for 41. DRS scores, and therefore average levels of functioning, differed significantly at admission (2.3, between mildly and moderately dependent) and discharge (1.1, independent in special environments, p<0.01). Average weekly care costs fell from €629 to €242, with costs recouped within 30 months. Thus, substantial savings result from inpatient rehabilitation, and these savings could have been greater had we considered also the economic benefit of enabling patients to return to employment.
KEYWORDS: Rehabilitation, cost-effectiveness, brain injury
Introduction
According to the Irish National Audit of Stroke Care and data from the Hospital In-Patient Enquiry scheme,1 in excess of 20,000 people in Ireland suffer some form of acquired brain injury (ABI) every year. ABI is the third most common cause of death and disability internationally and consequentially results in a substantial burden of disability for patients, families, health professionals and wider society. There is now clear evidence that rehabilitation interventions after acquired brain injury improve health outcomes, decrease costs by shortening hospital stays, reduce disability, and improve quality of life.2–8 Research on the health economics of rehabilitation indicates that specialist rehabilitation interventions, including those delivered through a multidisciplinary team led by a consultant in rehabilitation medicine, help to reduce the costs of disability and the need for health and social services.9–11
The Irish National Rehabilitation Hospital (NRH) provides a comprehensive range of specialist rehabilitation services to patients from throughout Ireland who, as a result of an accident, illness or injury, have acquired a physical or cognitive disability and who need specialist medical rehabilitation. The interdisciplinary team within the Brain Injury Programme provides specialist rehabilitation treatment and care designed to assist people with ABI to: adjust to their injury, achieve the safest possible level of functional independence and participate socially and in the community. The brain injury team – which consists of a consultant in rehabilitation medicine, non-consultant hospital doctors, nurses trained in rehabilitation, physiotherapists, occupational therapists, speech and language therapists, psychologists, clinical nutritionists, pharmacists and medical social workers – works with patients and their families and carers to achieve the best possible outcome from the rehabilitation programme, an inpatient programme tailored to meet each patient's individual needs.
The entire team formally discusses patients weekly. For each patient, at least one goal-setting conference, in which they are included, occurs towards the start of the admission – around 2 weeks after admission, when the interdisciplinary team have undertaken their initial assessments. These goals are reviewed weekly and there is at least one follow-up formal meeting between the team, patient and the patient's family. There is a discharge conference for each patient within a week of discharge. The team also liaise with community interdisciplinary teams to plan towards discharge. It is important to note that patients are already medically stable before admission. Adult patients with potential for improvement are admitted irrespective of age. However, those over 65 years with stroke are rehabilitated in other nationwide post-stroke rehabilitation programmes for older people.
Other groups have demonstrated the cost-effectiveness of rehabilitation after brain injury in different settings. Oddy and Ramos report cost benefits of up to £1.13 million on average per individual participating in neurobehavioural rehabilitation within a year of sustaining a brain injury.12 Andelic and colleagues have shown continuous rehabilitation to be less costly and more effective than a broken chain of rehabilitation.13 Van Heugten and coworkers demonstrated favourable societal cost benefits of a residential community reintegration programme.14 However, the cost-effectiveness of rehabilitation has not been explored before in an Irish context.
We aimed to examine the reduction in direct care costs after acquired brain injury that can be achieved through specialist rehabilitation at the tertiary specialist rehabilitation centre by assessing the changes in functional ability of patients with brain injury after a period of inpatient rehabilitation and the financial savings in terms of cost of care accrued as a result of these improvements in functionality.
Methods
The study included all patients discharged between 1 January 2011 and 31 December 2011 from the NRH Brain Injury Programme under one of the NRH rehabilitation consultants (AC). Patients who were not admitted for the purposes of rehabilitation were excluded. Patient demographics, including sex, age, diagnosis, time from onset of brain injury to admission, length of stay and discharge location, were recorded. Two functional measures are routinely used on all patients admitted for the Brain Injury Programme: the modified Barthel Index, which is calculated by the nursing staff, and the Disability Rating Scale (DRS), which is completed by the full interdisciplinary team. Both are recorded at the goal-setting conference and re-administered at the discharge conference.
Similar to previous analyses,9,15 we calculated the savings in cost of care by calculating the average difference between care costs on admission and on discharge. In these previous analyses estimated care costs were based on the Northwick Park Dependency Scale, but this is not used at our centre. Instead we used the level of functioning of the DRS, although we acknowledge that the Northwick Park Dependency Scale would have been preferable since it incorporates algorithms designed to calculate costs on the basis of clinical and care input, and hence the estimations of cost might be more accurate with this approach.
The estimated costs of care associated with each level of functioning are shown in Table 1. The cost of each hour of care was taken as the cost of care provided by the Irish Wheelchair Association and the cost of residential care was taken as the average cost provided through the Nursing Home Support Scheme (€1,200) plus the top-up amount (€400). Under the scheme, the cost of nursing home care is paid jointly by the patient and the government, with the patient's contribution determined by an assessment of their finances. Under this scheme, the government have negotiated a fixed weekly rate of €1,200. For those who are more dependent an additional €400 is paid.
Table 1.
Estimated costs of care based on DRS level of functioning.
| DRS level | Dependency | Care provided | Weekly cost, € |
|---|---|---|---|
| 0.0 | Independent | None | 0 |
| 0.5 | Between independent and independent in special environment | – | 58.75 |
| 1.0 | Independent in special environment | 1 hour daily, 5 days a week | 117.5 |
| 1.5 | Between independent in special environment and mildly dependent | – | 221.5 |
| 2.0 | Mildly dependent | One person for 3 hours daily, 5 days a week | 325.5 |
| 2.5 | Between mildly dependent and moderately dependent | – | 528.75 |
| 3.0 | Moderately dependent | Two people for 3 hours daily, 5 days a week | 705 |
| 3.5 | Between moderately dependent and markedly dependent | – | 1,152.5 |
| 4.0 | Markedly dependent | Residential care | 1,600 |
| 4.5 | Between markedly dependent and totally dependent | – | 1,600 |
| 5.0 | Totally dependent | Residential care | 1,600 |
The weekly cost of inpatient rehabilitation in the Brain Injury Programme at the National Rehabilitation Hospital is €4,900. ‘Between’ scores weekly costs represent an average of the integer scores on each side. DRS = disability rating scale.
Results
Seventy-two patients matched the criteria for inclusion in the study. Ten patients were excluded: five who were admitted for assessment of consciousness level and five admitted for disability management. Of the remaining 62 patients, data for DRS at admission and discharge were available for 41 (66.1%) – this is the group included in the study. Table 2 shows the demographics and diagnoses of individuals and time to admission. Patients are referred once they are stabilised and discharged from an intensive-care unit.
Table 2.
Diagnostic and demographic information in individuals with and without DRS available on admission and discharge.
| Parameter | Full data (n = 41) | Missing data (n = 21) | p value |
|---|---|---|---|
| Sex | 0.11 | ||
| Women | 16 (39%) | 4 (19%) | |
| Men | 25 (61%) | 17 (81%) | |
| Age (years), mean (SD, range) | 43.5 (12.7, 18–64) | 48.2 (11.7, 27–66) | 0.16 |
| Days from referral to admission, mean (SD, range) | 50.9 (35.1, 2–159) | 35.7 (39.3, 1–138) | 0.13 |
| Diagnosis | 0.29 | ||
| Aneurysm or arteriovenous malformations | 5 (12%) | 1 (5%) | – |
| Brain tumour | 1 (2%) | 2 (10%) | – |
| Encephalitis or meningitis | 2 (5%) | – | – |
| Haemorrhagic stroke | 2 (5%) | 3 (14%) | – |
| Ischaemic stroke | 23 (56%) | 9 (42%) | – |
| Other non-traumatic brain injury | 2 (5%) | 2 (10%) | – |
| Other stroke | 2 (5%) | 1 (5%) | – |
| Traumatic brain injury | 4 (10%) | 2 (10%) | – |
| Discharge destination | 0.5 | ||
| Home | 32 (79%) | 18 (86%) | – |
| Residential | 7 (17%) | 2 (10%) | – |
| Acute hospital | 1 (2%) | 1 (5%) | – |
| District hospital | 1 (2%) | – | – |
Data are n (%), unless otherwise specified. Because of rounding, some percentages do not total 100%. DRS = Disability Rating Scale; SD = standard deviation.
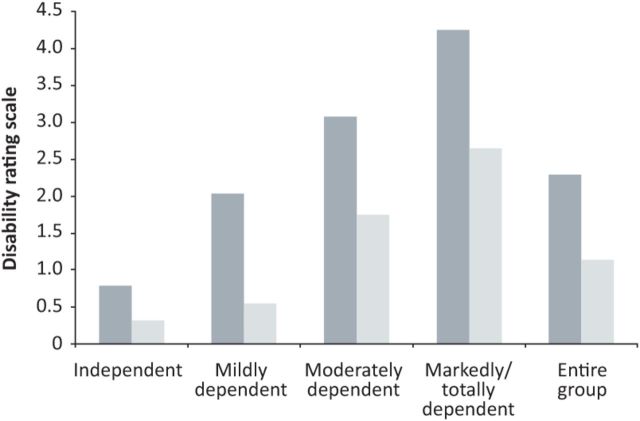
Fig 1 shows the proportion in each level of functioning (based on domain G of DRS) at admission and discharge, by category of dependency at admission. After an average length of stay of 79.9 days, the average level of function, based on DRS domain G, improved from 2.3 on admission to 1.1 on discharge. Table 3 details the mean admission and discharge function scales (modified Barthel Index and DRS domain G) in the overall group and the four categories of dependency on admission, and the average length of stay.
Fig 1.
Percentage of patients at each level of functioning (based on average DRS domain G) at admission (dark grey) and discharge (light grey). DRS = disability rating scale.
Table 3.
DRS (domain G) and modified Barthel Index scores on admission and discharge in each dependency subgroup.
| Dependency subgroup | DRS (domain G) | Modified Barthel Index | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Admission | Discharge | Change | p value | Admission | Discharge | Change | p value | |
| Independent | 14 | 0.8 (0–1.5) | 0.3 (0–1) | 0.5 | 0.003 | 89 (79–100) | 98 (88–100) | 8 | 0.0017 |
| Mildly dependent | 11 | 2.0 (2–2.5) | 0.5 (0–1) | 1.5 | 0.003 | 83 (64–96) | 90 (78–100) | 7 | 0.0032 |
| Moderately dependent | 6 | 3.1 (3–3.5) | 1.8 (0–3.5) | 1.3 | 0.051 | 66 (17–96) | 80 (38–100) | 14 | 0.0277 |
| Markedly or totally dependent | 10 | 4.3 (4–5) | 2.7 (2–4) | 1.6 | 0.046 | 35.4 (2–90) | 58.1 (9–93) | 23 | 0.0059 |
| Overall | 41 | 2.3 (0–5) | 1.1 (0–4) | 1.2 | <0.0001 | 71.2 (2–100) | 83.3 (9–100) | 12.1 | <0.0001 |
Data are mean (range). P values for difference are based on Wilcoxon’s signed-rank test. DRS = disability rating scale.
The average care costs on admission of the group were €629.1 weekly, which fell to €242.2 weekly at discharge. At a daily inpatient cost of €700, the average cost of inpatient rehabilitation was €48,949 per person. The average length of time for the cost of inpatient stay to be covered by the savings in terms of reduced care costs was 30 months. These figures for each subgroup are detailed in Table 4.
Table 4.
Costs for continuing care and inpatient rehabilitation by dependency subgroup.
| n | Weekly admission care costs, € | Weekly discharge care costs, € | Weekly mean saving, € | Mean length of stay, days | Total mean inpatient cost, € | Weeks to cover cost of inpatient rehabilitation | |
|---|---|---|---|---|---|---|---|
| Independent | 14 | 96 (0–221) | 38 (0–118) | 58 (0–222) | 59 (31–88) | 41,500 | 716 |
| Mildly dependent | 11 | 343 (325–528) | 59 (0–118) | 284 (208–411) | 65 (41–79) | 45,500 | 160 |
| Moderately Dependent | 6 | 780 (705–1,153) | 418 (0–1,153) | 362 (0–705) | 65 (37–79) | 45,383 | 125 |
| Markedly or totally dependent | 10 | 1,600 (1,600–1,600) | 625 (325–1,600) | 975 (0–1,275) | 93 (65–185) | 65,310 | 67 |
| Overall | 41 | 629 (0–1,600) | 242 (0–1,600) | 387 (0–1,275) | 70 (31–185) | 48,949 | 127 |
Data are mean (range).
Discussion
This analysis of the cost effectiveness of inpatient rehabilitation in patients with brain injury has demonstrated that, although the cost of inpatient rehabilitation in this group is expensive initially, in the medium term these costs are covered by the savings in care costs. In the group as a whole, the costs were recovered within 30 months. On average, after the first 30 months, inpatient rehabilitation is associated with a cost saving of almost €20,000 per patient annually.
As shown in Table 4, inpatient rehabilitation was most cost effective in the group who were markedly dependent on admission. In this group, costs were covered in only 67 weeks (15.6 months); thereafter, calculated savings of over €50,000 per patient accrued annually. These results are similar to the findings in a previous study by Turner-Stokes and colleagues.16,17 In that analysis, in the high-dependency group, the weekly cost of care fell by an average of £639, and the cost of inpatient rehabilitation was covered by these cost savings in 16.3 months. Rehabilitation in the group who were deemed either independent or independent in a special environment on admission was less cost effective than that in the more dependent group.
However, in our population, those in the independent groups tended to be younger patients in whom there was potential for savings to continue for at least 20–25 years. These individuals were admitted specifically for the purpose of working on more subtle cognitive and behavioural difficulties with the aim of returning to employment. Such patients might have been excluded from previous studies. For example, in the analysis by Turner-Stokes and colleagues, their lowest dependency group were equivalent to our mildly dependent group (mean Barthel index of 16.1 vs mean modified Barthel Index of 84, respectively). When the lowest-dependency group is excluded from our analysis, the average length of time to cover the costs of inpatient rehabilitation falls to 22.7 months. However, specialist rehabilitation is still valuable and cost effective in this group.
Ceiling and floor effects of dependency scales can result in underestimation of cost-effectiveness of rehabilitation. For example, in our analysis, patients who were markedly dependent or totally dependent might have had significant reductions in dependency, but because of floor effects these improvements might not translate into changes in the DRS but could result in substantial improvements in quality of life for patients and their families and carers. Likewise, substantial improvements in individuals with brain injury who are independent on admission might be missed as a result of ceiling effects on functional scores, despite substantial benefits in terms of cognition and behaviour. The financial implications of enabling these individuals to return to employment, through a patient-centred rehabilitation programme, could also be underestimated, further augmenting the ceiling effect.
Cost-effectiveness of rehabilitation could be improved further if bed day costs were reduced. However, it should be remembered that, in practice, many of the patients included in this analysis were transferred from acute hospitals in which the bed day costs were approximately 150% higher. The savings accrued as a result of vacating an acute hospital have not been taken into account in this analysis. Another approach would be to limit the duration of inpatient rehabilitation and combine with intensive outpatient rehabilitation. An important strength of this analysis is the inclusion of patients undergoing routine clinical care. As there were no research or experimental aspects to the rehabilitation programme, these results are likely to be representative of the current routine inpatient programme at the NRH.
There are also some limitations. The interdisciplinary team assessing the level of dependency on discharge were not blinded to the level on admission. The team could have been biased towards good results, as they also provide the therapy. As mentioned previously, the use of Northwick Park Dependency Scale rather than the DRS might have produced more accurate estimations of cost. In this report, we have detailed the changes in dependency and consequent care costs after a period of inpatient rehabilitation. However, we do not have information about the changes that would have occurred without rehabilitation and so cannot definitively ascribe these positive changes to the rehabilitation process. A randomised controlled trial of rehabilitation versus no rehabilitation would provide more information but would generate an ethical dilemma, in that it would necessitate denying treatment, which is considered standard and has sufficient evidence to support its use, to a group of individuals. We have looked only at financial savings here. An analysis of gains in quality of life would clearly provide a more accurate reflection of the value of inpatient rehabilitation.
Individuals and society gain much more from rehabilitation than the financial savings from reducing the cost of care. The rehabilitation process focuses on increasing participation in the community and increasing functional abilities. This is reflected in the last domain of the DRS, employability. In our study, 66% of individuals who were classed not employable on admission were considered employable by the time of discharge with 41% of these in selected competitive jobs.
This is the first analysis of the cost effectiveness of inpatient rehabilitation in an Irish setting. We have shown that, on average, the cost of inpatient rehabilitation is covered by the savings resulting from reductions in dependency within 30 months. Inpatient rehabilitation seems to be most cost effective in individuals with brain injury who are markedly dependent on admission, with only 15.6 months required to cover the inpatient cost in this group. After this time, calculated savings of over €50,000 per patient annually can be expected.
References
- 1.Irish Heart Foundation Irish national audit of stroke care. Dublin: Irish Heart Foundation, 2007. [Google Scholar]
- 2.Langhorne P, Williams BO, Gilchrist W, Howie K. Do stroke units save lives? Lancet 1993;342:395–8. [DOI] [PubMed] [Google Scholar]
- 3.Barnes M, Radermacher H. Community rehabilitation in neurology: a summary of the evidence of the efficacy of community rehabilitation. Cambridge: Cambridge University Press, 2003. [Google Scholar]
- 4.Edwards SG, Thompson AJ, Losseff N, Playford ED. Shortening inpatient stay for stroke. Lancet 2002;359:2205. [DOI] [PubMed] [Google Scholar]
- 5.Turner-Stokes L. Evidence for the effectiveness of rehabilitation following acquired brain injury: a synthesis of two systematic approaches. J Rehab Medicine 2008;40:691–701. [DOI] [PubMed] [Google Scholar]
- 6.Slade A, Tennant A, Chamberlain MA. A randomised controlled trial to determine the effect of intensity of therapy upon length of stay in a neurological rehabilitation setting. J Rehab Med 2002;34:260–6. [DOI] [PubMed] [Google Scholar]
- 7.Kwakkel G, Wagenaar RC, Twisk JW, Lankhorst GJ, Koetsier JC. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet 1999;354:191–6. [DOI] [PubMed] [Google Scholar]
- 8.Ronning OM, Guldvog B. Outcome of subacute stroke rehabilitation: a randomized controlled trial. Stroke 1998;29:779–84. [DOI] [PubMed] [Google Scholar]
- 9.Turner-Stokes L, Paul S, Williams H. Efficiency of specialist rehabilitation in reducing dependency and costs of continuing care for adults with complex acquired brain injuries. J Neurol Neurosurg Psychiatry 2006;77:634–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner-Stokes L. Cost-efficiency of longer-stay rehabilitation programmes: can they provide value for money? Brain Injury 2007;21:1015–21. [DOI] [PubMed] [Google Scholar]
- 11.Worthington AD, Matthews S, Melia Y, Oddy M. Cost-benefits associated with social outcome from neurobehavioural rehabilitation. Brain Injury 2006;20:947–57. [DOI] [PubMed] [Google Scholar]
- 12.Oddy M, da Silva Ramos S. The clinical and cost-benefits of investing in neurobehavioural rehabilitation: a multi-centre study. Brain Injury 2013;27:1500–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andelic N, Ye J, Tornas S, et al. Cost-effectiveness analysis of an early-initiated, continuous chain of rehabilitation after severe traumatic brain injury. J Neurotrauma 2014;31:1313–20. [DOI] [PubMed] [Google Scholar]
- 14.Van Heugten CM, Geurtsen GJ, Derksen RE, et al. Intervention and societal costs of residential community reintegration for patients with acquired brain injury: a cost-analysis of the Brain Integration Programme. J Rehab Med 2011;43:647–52. [DOI] [PubMed] [Google Scholar]
- 15.O’Connor RJ, Beden R, Pilling A, Chamberlain MA. What reductions in dependency costs result from treatment in an inpatient neurological rehabilitation unit for people with stroke? Clin Med 2011;11:40–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turner-Stokes L. The evidence for the cost-effectiveness of rehabilitation following acquired brain injury. Clin Med 2004;4:10–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fleminger S. Can severely disabled patients benefit from in-patient neurorehabilitation for acquired brain injury? J Neurol Neurosurg Psychiatry 2006;77:570. [DOI] [PMC free article] [PubMed] [Google Scholar]