ABSTRACT
Standard medical education dictates that the vast majority of cases of an alanine aminotransferase (ALT) level >1,000 IU/l will be due to acute ischaemia, acute drug-induced liver injury (DILI) (usually paracetamol) or acute viral hepatitis. There are very few references in the literature to other potential causes of an ALT >1,000 IU/l nor to the prognosis ascribed to each aetiology. In this study, we have confirmed that the main causes of a dramatic ALT rise are ischaemic liver injury, DILI and viral hepatitis. Common bile duct stones and hepatitis E are two causes for which there needs to be a high index of suspicion as the necessary tests may not be in the clinician's first-line investigation panel. Failing to find a cause and determining that the cause was ischaemic both have poor prognostic implications.
KEYWORDS : Alanine aminotransferase, transaminases, acute hepatitis, aetiology, prognosis
Introduction
Alanine aminotransferase (ALT) is an enzyme involved in the alanine cycle and is primarily found in muscle and the liver.1 In clinical practice, ALT is measured as one of the liver function tests (LFTs) to screen for hepatocellular injury.2 The differential diagnosis for elevated serum aminotransferases is broad and includes metabolic liver disease, alcohol-related liver disease, ischaemic hepatopathy, hepatotoxicity from drugs or toxins, autoimmune, hepatocellular and biliary injury, chronic viral hepatitis and malignant infiltration. Typically, ALT levels in these conditions can be two-to-five times the upper limit of normal, which is around 40 IU/l in most hospitals. Occasionally ALT levels can rise to levels of >1,000 IU/l. This will usually lead to an urgent referral to hospital or within hospital to the gastroenterology or hepatology teams. Standard medical education dictates that the vast majority of these cases will be due to acute ischaemia or congestion, acute drug-induced liver injury (DILI) (usually paracetamol) or acute viral hepatitis.3–5 The requirement for admission to hospital and the prognostic and treatment implication for these three groups of conditions are very different and as such, it is important to determine the cause of the dramatic ALT elevation early.
Our aim was to review all the cases with an ALT level >1,000 IU/l in our city centre university hospital in order to determine cause and prognosis and improve urgent care pathways.
Materials and methods
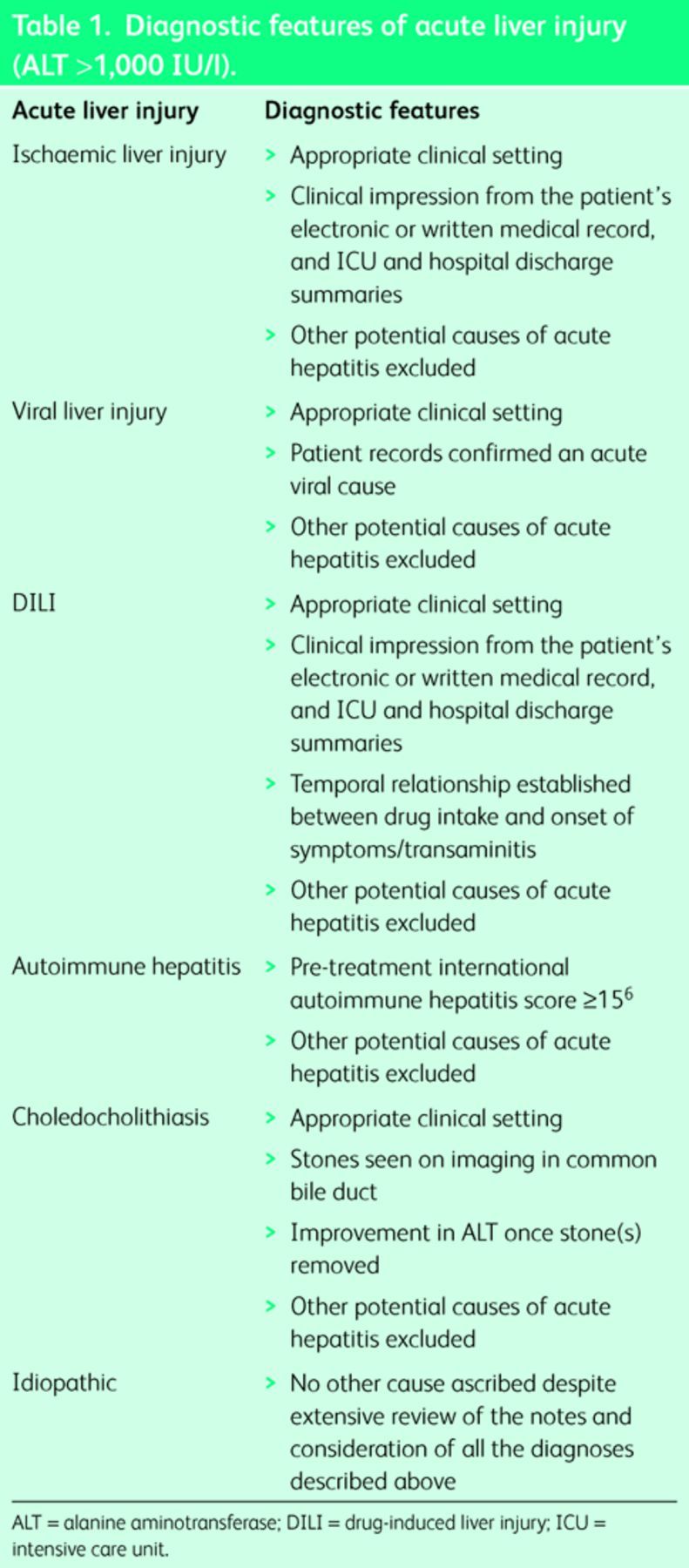
This single-centre, retrospective, observational study was conducted in a tertiary referral university hospital over a two-year period. A retrospective chart review was performed on every patient who had presented to the hospital over this time period with an ALT >1,000 IU/l. This included reviewing, where applicable, the primary care referral letters for that episode, the written and electronic patient charts, patient medication records, intensive care unit (ICU) discharge summaries, hospital discharge summaries and death notifications. Where possible, aetiology was ascribed and prognosis (survival to hospital discharge) was recorded. In all cases, the aetiology ascribed in the patient notes was correlated with diagnostic criteria that had been established prior to the review (Table 1). All data were anonymised and recorded in a secure dedicated electronic database. Statistical data analysis was carried out using SPSS version 20. The study protocol was approved by the Research Ethics Committee of the Mater Misericordiae University Hospital (MMUH 1/378/1545 TMR).
Table 1. .
Diagnostic features of acute liver injury (ALT >1,000 IU/l).
Results
In total, 182 patients (56% (n = 102) male and 44% (n = 80) female) with an ALT >1,000 IU/l were identified.
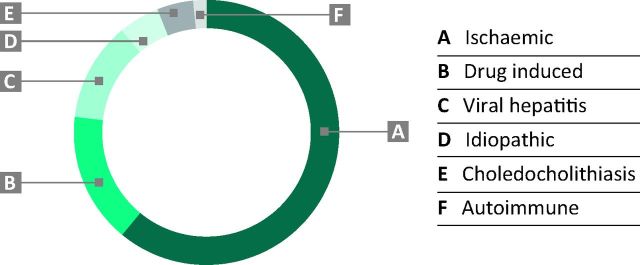
The aetiology of the raised ALT is shown in Fig 1. As expected, ischaemic liver injury (61%, n = 111), DILI (15.9%, n = 29) and acute viral hepatitis (12.1%, n = 22) were the most common causes accounting for nearly 90% of all cases. Interestingly, the next most common causes were idiopathic (5.0%, n = 9) and acute choledocholithiasis (4.4%, n = 8). Autoimmune hepatitis (1.6%, n = 3) made up the remaining cases.
Fig 1.
Aetiology of liver injury in patients with an ALT >1,000 IU/l (%) (n = 182). ALT = alanine aminotransferase.
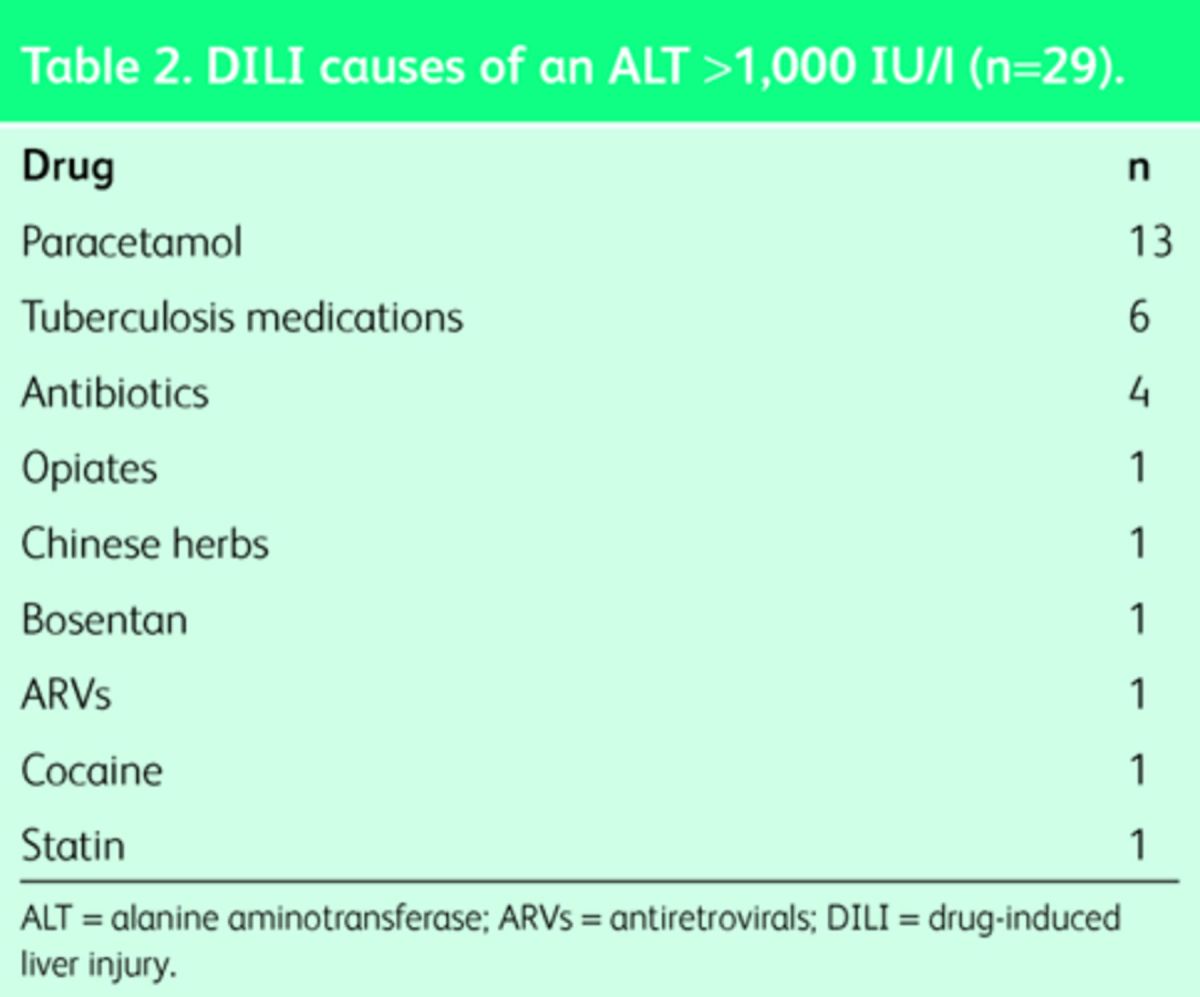
Paracetamol toxicity accounted for almost half (13/29) of the DILI cases. The other common causes were anti-tuberculosis medications (6/29) and other antibiotics (4/29). Other drugs were also implicated in smaller numbers (Table 2).
Table 2. .
DILI causes of an ALT >1,000 IU/l (n = 29).
In order of frequency, the viral hepatitides causing ALT >1,000 IU/l were hepatitis B (7/22), hepatitis C (5/22), hepatitis E (4/22) and hepatitis A (3/22). Cytomegalovirus, Epstein–Barr virus and varicella zoster each accounted for one case.
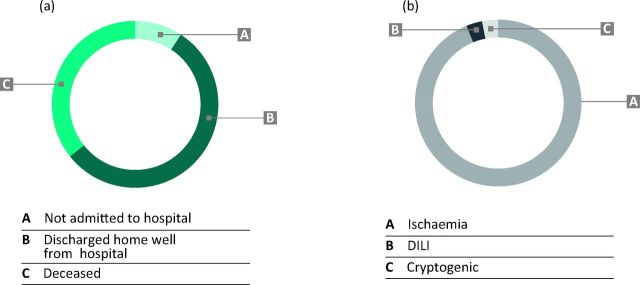
9.3% (n = 17) of patients had their acute hepatitis managed as outpatients, 54.9% (n = 100) were admitted to the hospital and discharged home well and 35.7% (n = 65) died during their admission (Fig 2A). Survival was highly dependent on the aetiology of the raised ALT. Ischaemic liver injury was the cause of the ALT >1,000 IU/l in the vast majority of patients who died during the admission (93.8%, n = 61) (Fig 2B). Overall mortality was 55% (61/111) in the ischaemic group, 6.9% (2/29) in DILI and 0% if the aetiology was viral hepatitis, stone disease or autoimmune hepatitis. 22.2% (2/9) of those patients in whom a cause could not be identified died.
Fig 2.
(A) Outcome of patients who presented with an ALT >1,000 IU/l (%) (n = 182). (B) Aetiology of ALT >1,000 IU/l in the deceased cohort (%) (n = 65; 35.7% of total cohort). ALT = alanine aminotransferase; DILI = drug-induced liver injury.
Conclusions
We reviewed the investigations and outcomes of 182 cases where the ALT measurement was >1,000 IU/l. The results were generated by the biochemistry department attached to a tertiary referral university hospital and could come from the hospital in-patients or patients attending local general practitioners. The vast majority of these patients were admitted to hospital but some were managed in the community by primary care or in the hepatology out-patient department. There were some findings that reinforced standard teaching around ‘acute hepatitis’ and some that were surprising.
To the best of the authors knowledge, no similar case series has been published, however, a review of the literature reveals that ischaemia, drugs and toxins can cause elevations in ALT of greater than 40 times the upper limit of normal (ULN) while viral aetiology generally causes elevations of 10 to 40 times the ULN, ie any of these aetiologies can cause an ALT of >1,000 IU/l.7,8 Prognosis largely depends on aetiology and as such it is important to make the correct diagnosis from the outset. There are no specific blood tests for ischaemic or DILI and so detailed history taking and a thorough physical examination are essential in order to make the correct diagnosis. A number of laboratory tests and patterns may also be useful. In viral hepatitis, transaminases rarely increase to greater than 40 times ULN unlike that seen in ischaemic or DILI. Lactate dehydrogenase (LDH) activity often is higher than that of AST at presentation in ischaemic or drug-induced hepatic injury,8,9 as compared with viral hepatitis when the LDH level is generally normal or only slightly above the ULN.10 Choledocholithiasis is a recognised but rare cause of severe transaminitis.11 Agahi et al described three cases of choledocholithiasis causing an ALT >1,000 IU/l, all of these cases had repeated investigation for liver disease before eventual identification of common bile duct stones with magnetic resonance cholangiopancreatogram.12 Presentation of fulminant AIH has been described with transaminases of >1,000 IU/l, but it is rare.13 A recent single-centre review of all cases of AIH over a ten-year period identified 32 cases of acute severe AIH (defined as an international normalised ratio >1.5 without evidence of fibrosis). Although exact numbers were not given, the average AST was 619 IU/l (116–2,690 IU/l) indicating that very few patients had an AST of >1,000 IU/l.14
The proportion of patients that had ischaemic injury, DILI or viral hepatitis was exactly as we would have expected at around 90%. We were surprised to find choledocholithiasis as the next most common cause of an ALT >1,000 IU/l (8/182 cases). This is significantly higher than the incidence rates seen in the literature and may confound admitting teams who would expect biliary colic due to bile duct obstruction to present with obstructive LFTs.
The second important clinically relevant finding from this study was that hepatitis E was more frequently detected than hepatitis A. This was in spite of hepatitis A serology being in the first-line viral screen and the need for hepatitis E serology to be requested separately if the first-line screen is negative. Hepatitis E is one of the most common causes of acute hepatitis worldwide, with the majority of cases occurring in Asia. In recent years, however, an increasing number of acute and chronic hepatitis E virus infections have been reported in industrialised countries.15 This has both clinical and treatment implications. In the first instance, a positive viral serology test allows the clinician to stop searching for other causes and may avoid liver biopsy. In addition, hepatitis E infection can become chronic in immunocompromised patients and lead to hepatic fibrosis and cirrhosis. Treatment strategies are currently being evaluated and attempts are being made to develop effective hepatitis E virus vaccines.16 Physicians need to be aware of hepatitis E as a cause of both acute and chronic hepatitis in immunocompromised patients and this is particularly important if there may be a risk of pregnant women being exposed to infection given the high maternal mortality associated with the syndrome.
Nine patients had no cause identified for their acute transaminases. Four of these patients were not admitted to our institution nor were they referred to hepatology outpatient clinics. It was established that these patients were still alive but it was not possible to retrospectively establish the cause of the liver injury. They may have been referred to another local hospital or managed in the community. Despite extensively reviewing the clinical notes for the remaining five patients, it was not possible to confidently attribute a cause for the liver injury. There were no recorded hypotensive episodes, viral serology was negative and no incriminating drugs were recorded in the medical history. It is important to highlight that none of the patients were checked for hepatitis E. A retrospective effort to establish the hepatitis E virus status of these patients was not successful because samples were no longer available (stored for six months).
Finally, the clinical courses are very different for each of the aetiologies of liver injury. This has implications for follow-up. The prognosis in acute viral hepatitis, even with ALT >1,000 IU/l is extremely good and these patients can almost always be managed closely in the community. DILI has a well-defined mortality which will be drug-dependent and, certainly in the case of paracetamol, very predictable. Patients in whom the ALT rises to >1,000 IU/l due to ischaemic liver injury have a very poor prognosis. Often this is evident at the time, with the liver being simply another organ insulted in multi-organ failure. Sometimes, however, the ALT rise may be one of the earlier signs that augurs poorly for patient prognosis.
Limitations of this study are similar to those seen in other retrospective studies. This study depended on the availability, accuracy and comprehensiveness of the medical records. In the majority of cases it was possible to confidently attribute an aetiology to each patient; however there were a small number of cases where an educated assumption needed to be made. It was not possible to retrospectively apply diagnostic criteria such as the CIOMS/RUCAM scale for DILI,17 to check LDH, or to complete the viral or autoimmune screens in those who had some missing results. There were nine cases where it was not possible to define an aetiology. The high mortality seen in the idiopathic group could possibly be explained by the fact that some of this group were in fact unrecognised ischaemic or drug-induced injuries.
In summary we have defined the main causes of a dramatic ALT rise and associated a prognosis with each aetiological group. Common bile duct gallstones and hepatitis E are two causes for which there needs to be a high index of suspicion, as the necessary tests may not be in the first-line investigation panel of the clinician. Failing to find a cause and determining that the cause was ischaemic both have poor prognostic implications.
References
- 1. .Zimmerman HJ, West M. Serum enzyme levels in the diagnosis of hepatic disease. Am J Gastroenterol 1963;40:387–404. [PubMed] [Google Scholar]
- 2. .Ellis G, Goldberg DM, Spooner RJ, Ward AM. Serum enzyme tests in diseases of the liver and biliary tree. Am J Clin Pathol 1978;70:248–58. [DOI] [PubMed] [Google Scholar]
- 3. .Xu HM1, Chen Y, Xu J, Zhou Q. Drug-induced liver injury in hospitalized patients with notably elevated alanine aminotransferase. World J Gastroenterol 2012;18:5972–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. .Hickman PE, Potter JM. Mortality associated with ischaemic hepatitis. Aust N Z J Med 1990;20:32–4. [DOI] [PubMed] [Google Scholar]
- 5. .Lee WM, Seremba E. Etiologies of acute liver failure. Curr Opin Crit Care 2008;14:198–201. [DOI] [PubMed] [Google Scholar]
- 6. .Manns MP, Czaja AJ, Gorham et al. Diagnosis and management of acute hepatitis. Hepatology 2010;51:2193–213. [DOI] [PubMed] [Google Scholar]
- 7. .Dufour DR1, Lott JA, Nolte FS, et al. Diagnosis and monitoring of hepatic injury. II. Recommendations for use of laboratory tests in screening, diagnosis, and monitoring. Clin Chem 2000;46:2050–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. .Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005;172:367–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. .Fry SW, Seeff LB. Hepatotoxicity of analgesics and anti-inflammatory agents. Gastroenterol Clin North Am 1995;24:875–905. [PubMed] [Google Scholar]
- 10. .Rozen P, Korn RJ, Zimmerman HJ. Computer analysis of liver function tests and their interrelationships in 347 cases of viral hepatitis. Isr J Med Sci 1970;6:67–79. [PubMed] [Google Scholar]
- 11. .Nathwani RA, Kumar SR, Reynolds TB, Kaplowitz N. Marked elevation in serum transaminases: an atypical presentation of choledocholithiasis. Am J Gastroenterol 2005;100:295–8. [DOI] [PubMed] [Google Scholar]
- 12. .Agahi A, McNair A. Choledocholithiasis presenting with very high transaminase level. BMJ Case Rep 2012;pii:bcr2012007268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. .Kessler WR, Cummings OW, Eckert G, et al. Fulminant hepatic failure as the initial presentation of acute autoimmune hepatitis. Clin Gastroenterol Hepatol 2004;2:625–31. [DOI] [PubMed] [Google Scholar]
- 14. .Yeoman AD, Westbrook RH, Zen Y, et al. Prognosis of acute severe autoimmune hepatitis (AS-AIH): the role of corticosteroids in modifying outcome. J Hepatol 2014;61:876–82. [DOI] [PubMed] [Google Scholar]
- 15. .Riveiro-Barciela M, Rodríguez-Frías F, Buti M. Hepatitis E virus: new faces of an old infection. Ann Hepatol 2013;12:861–70. [PubMed] [Google Scholar]
- 16. .Haffar S, Bazerbachi F, Lake JR. Making the case for the development of a vaccination against hepatitis E virus. Liver Int 2015;35:311–6. [DOI] [PubMed] [Google Scholar]
- 17. .Tajiri K, Shimizu Y.Practical guidelines for diagnosis and early management of drug-induced liver injury. World J Gastroenterol 2008;14:6774–85. [DOI] [PMC free article] [PubMed] [Google Scholar]