OVERVIEW
Please submit letters for the editor's consideration within three weeks of receipt of Clinical Medicine. Letters should ideally be limited to 350 words, and sent by email to: clinicalmedicine@rcplondon.ac.uk
Editor – You have previously highlighted the potential benefits of the deployment of physician associates (PAs) to emergency departments in the UK (Clin Med 2014;3:219–20). Tamara Ritsema subsequently elaborated on the scope of practice of PAs working in UK emergency departments from a national perspective. (Clin Med 2014;6:691–4). To expand on this further, I offer a brief case study of PAs working in a UK emergency department.
In July 2011, a district general hospital in the West Midlands recruited three UK-trained PAs to join a US-trained PA already working in emergency medicine. The Trust has two acute hospital sites, each with an emergency department and two PAs were placed in each of these. On one site the PAs were part of the junior doctor rota, taking gaps that would have been filled by locum doctors, while at the second site they had a separate rota. Each had a designated consultant acting as an educational supervisor and on a day-to-day basis worked under the supervision of the consultant and registrars in the department.
All four PAs could work across the departments, seeing undifferentiated patients presenting to ‘minors’, ‘majors’, ‘paediatrics’ and ‘resuscitation’, taking patient histories, undertaking physical examination, ordering and interpreting diagnostic tests and procedures, formulating a diagnosis and initiating management, or referring to speciality as required. They employed a range of diagnostic and therapeutic procedures, some of which PAs have from graduation (for example suturing, venepuncture and cannulation), to more complex procedures (such as digital ring blocks and chest drain insertion).
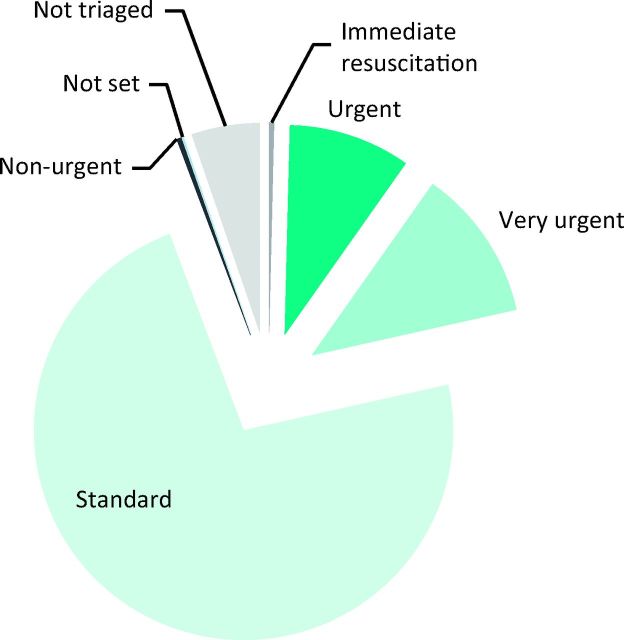
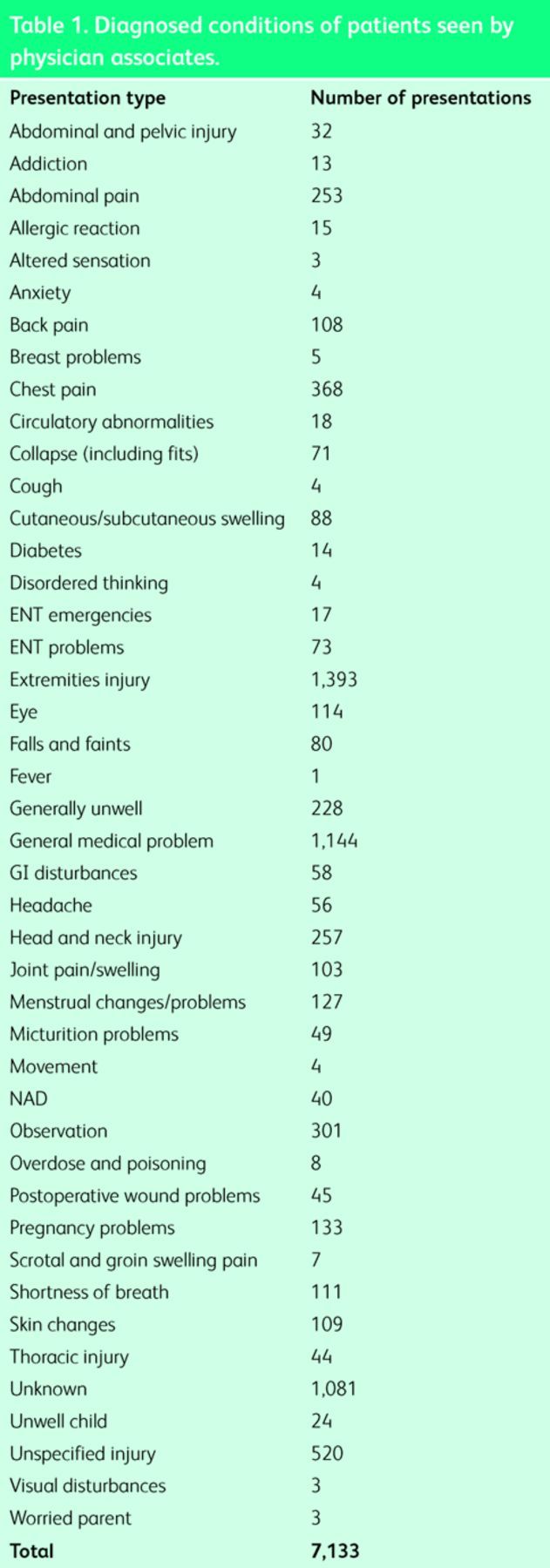
During the 12-month period between September 2011 and August 2012, the four PAs saw a total of 7,133 patients.1 The triage categories of these patients varied from five (least urgent) to one (most urgent) (Fig 1), and this is reflected by the types of presenting complaints that these patients booked in with, which are specified by the Department of Health as those which a PA should be able to assess from graduation.2 These included chest pain, shortness of breath, collapse and a variety of minor illness and injury. A more precise breakdown of the specific conditions seen is presented in Table 1.
Fig 1.
Triage categories of patients seen by physician associates.
Table 1. .
Diagnosed conditions of patients seen by physician associates.
This case study demonstrates that PAs working in emergency departments are utilising the generalist nature of their training by seeing a wide, undifferentiated caseload of patients that present with a variety of medical and surgical conditions. This is making a dynamic and valuable contribution to service provision at a time when it is becoming increasingly difficult to recruit staff to emergency medicine.
References
- 1. .Plant M.Database review of physician associate activity in A&E. Birmingham: Information Services, Sandwell and West Birmingham Hospitals NHS Trust, 2012(unpublished). [Google Scholar]
- 2. .Department of Health The competence and curriculum framework for physician assistants. London: DH, 2006. Available online at www.dh.gov.uk/en/Publicationsandstatistics/Publications/Publications PolicyAndGuidance/DH_4139317 [Accessed 11 March 2015]. [Google Scholar]