As Bob Dylan has said ‘The times they are a-changin’. Only a decade ago stroke patients in the UK would routinely wait two to three days for their emergency computed tomography (CT) scan following admission. Some thought that this delay was even advantageous as it allowed infarct changes to become well established. For ischaemic strokes, acute treatment was limited to aspirin.
Moving forward 10 years, with the introduction of routine intravenous thrombolysis and the advent of interventional neuroradiology, Greater London has undergone a dramatic transformation of acute stroke services. Currently, eight hyper acute stroke units (HASUs) are being established across the capital, providing 116 monitored beds (Fig 1). The aim of this is to offer equitable, around-the-clock access to stroke specialists, investigations, imaging and, if indicated, thrombolysis. Thrombolysis, if given early enough, has been shown to significantly reduce stroke morbidity, with a number needed to treat of 3.1.1 This has the potential to make serious inroads into a condition that afflicts 110,000 people yearly in the UK. If established infarct changes are seen on a CT brain, stroke physicians now would feel an opportunity had been missed.
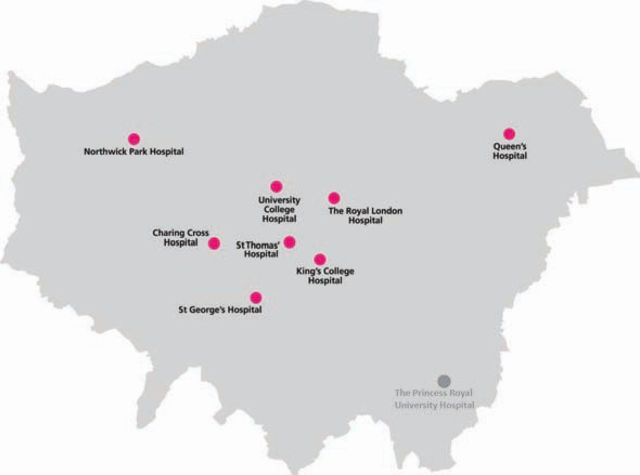
Fig 1.
The location of hyper acute stoke units (HASUs) in Greater London. The unit at Princess Royal University Hospital is scheduled to open in April 2011. In the interim, St Thomas' Hospital is providing a transitional service.
This paper describes experiences in the North Central London sector, which spans inner city areas to the northern green belt, with University College Hospital (UCLH) as the serving HASU. Transforming stroke services has been taxing at times and some of the key challenges faced and lessons learnt are discussed below.
Decommissioning
The 2004 Sentinel stroke audit showed that the overall standard of stroke services in London was lower than in other parts of the country.2 Quality of care markers, such as proportion of stroke patients treated in a stroke unit, physiotherapy assessment within 72 hours and CT brain scan within 24 hours of stroke, were not being met by many London units. In 2006, by these measures, services had worsened.
In order to address this issue, several models of care were considered and a transparent public consultation was undertaken. A ‘hub and spoke’ model was decided upon, which envisaged fewer acute centres to concentrate expertise and resources, thereby driving quality upwards.
This has resulted in some services being decommissioned, which has understandably been controversial and has resulted in challenges from the public, MPs, and healthcare professionals. In response, Healthcare for London (HfL) has been required to demonstrate the robustness of the ‘hub and spoke’ model. Already there are early indications that this model is effective in improving access to thrombolysis.3
Loss of expertise
With the transformation of services there has been concern over the risk of losing valuable experience and expertise from decommissioned acute units.
In the North Central London sector a joint approach to leading the HASU has been developed. Although the HASU is based at UCLH, half of the stroke consultants are from hospitals in the rest of the sector. This collaborative approach is in no small part due to the close links between local stroke units forged through the cardiac and stroke network and working together within one of the recently created academic health science centres, UCL Partners. By joint working, better links and cooperation between units have been forged, while the issue of an acute shortage in stroke specialists has also been addressed.
Changing mindset
For a long time stroke has been perceived as a rehabilitation specialty rather than an acute medical specialty in part due to the lack of acute stroke treatments available. Stroke thrombolysis is a time-critical service and for it to be successful, acute stroke needs to be recognised and reprioritised as a medical emergency by the public and healthcare professionals alike.4
The USA has recognised the importance of classifying strokes as emergencies. The phrase ‘brain attack’ is synonymous with strokes and, along with ‘time is brain’, is used to convey a sense of urgency on a par with acute coronary syndromes.
In 2009, the Department of Health rolled out the ‘Act FAST’ campaign, aimed at increasing awareness among the public. This has had a significant impact on the public psyche, on several occasions patients have rapidly accessed healthcare due to recognition of their early stroke symptoms matching the descriptions from the TV campaign.
Iterative improvements
During the early stages of our HASU development it was thought that expedient thrombolysis was being delayed due to the lack of a dedicated CT scanner in accident and emergency (A&E). However, when carefully audited, delays were distributed throughout the care pathway. Many small changes to the thrombolysis pathway have been iteratively implemented, rather than making one significant change. Implemented changes include ‘next available slot’ CT scanning, 24-hours hot CT scan reporting, pre-hospital activation of emergency stroke team, priority lift passes, thrombolysis training, regular quality and audit meetings. Currently over 70% of the patients at UCLH are thrombolysed with a door-to-needle time of less than one hour, which contrasts with only 10% prior to the establishment of the HASU. Other centres report similar improvements due to an ‘aggregation of marginal gains’.5
Pathway changes
For the pre-hospital pathway, London Ambulance Service has assigned strokes a ‘Category A’ priority, with a response time of under eight minutes. Suspected stroke patients are FAST assessed by paramedics to determine whether or not patients enter acute stroke pathways at their nearest HASU bypassing local A&Es.
The HASU is intended to provide the first two to three days of care for stroke patients, the rest being provided by local stroke units. Patient's progress has been actively managed through the stroke pathway by the team closely working with other units. For example, ensuring key investigations are timely obtained, improving communication to receiving units of expected transfer dates, active discharge planning and proactive bed management policies. The Stroke Network has been instrumental in facilitating some of these processes, allowing a forum for discussion, sharing of ideas, education and for collaboration.
Early results
This new model of acute stroke care was phased in across London in February 2010. From July 2010 onwards HASUs directly received all suspected stroke patients. Preliminary results have shown an increase in thrombolysis rates from 3.5% between February and July 2009 to 12% over the same period in 2010. From February 2010 to June 2010 the 30-day mortality figure for UCLH HASU patients was 6% compared to a UK average of 22%. Approximately 35% of patients are discharged directly home. Patients requiring additional in-hospital care are transferred to their local stroke unit within 72 hours. Throughout London the combined HASU and stroke unit length of stay for patients has fallen to a mean of 19.4 days compared to a UK average of 24 days.
Conclusion
London has undergone the largest transformation of metropolitan acute stroke services worldwide. Although preliminary results are highly encouraging, improved long-term outcomes, for example in mortality, disability and return to normal life roles, need to be demonstrated. Additionally, in the current economic climate the cost effectiveness of this new model needs to be evident. Although the challenges and constraints will vary region to region, many of the lessons learnt in setting up HASU services can be of benefit to other units nationally and internationally. The next step is ensuring acute stroke patients wherever they are in the UK have around-the-clock access to hyper acute stroke services and that the current momentum is carried forward into the development of comprehensive services supporting stroke survivors following rehabilitation.
References
- 1.Saver JL. Number needed to treat estimates Incorporating effects over the entire range of clinical outcomes: novel derivation method and application to thrombolytic therapy for acute stroke. Arch Neurol 2004;61:1066–70 10.1001/archneur.61.7.1066. [DOI] [PubMed] [Google Scholar]
- 2.Irwin P, Hoffman A, Lowe D, Pearson M, Rudd A. Improving clinical practice in stroke through audit: results of three rounds of National Stroke Audit. J Eval Clin Pract 2005;11:306–14 10.1111/j.1365-2753.2005.00529.x. [DOI] [PubMed] [Google Scholar]
- 3.Moynihan B, Davis D, Pereira A, Cloud G, Markus HS. Delivering regional thrombolysis via a hub-and-spoke model. J R Soc Med 2010;103:363–9 10.1258/jrsm.2010.090434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emergency and comprehensive care for stroke needed Lancet 2009 10.1016/S0140-6736(09)60833-3;373:1496. [DOI] [PubMed] [Google Scholar]
- 5.O'Brien A, Guyler P. Aggregation of marginal gains in the care of acute stroke. Br J Hosp Med 2009;70:154–7. [DOI] [PubMed] [Google Scholar]