Abstract
Neurological conditions comprise a significant proportion of patient admissions to hospital but, in the majority of cases, are admitted under the care of non-neurological physicians. As a consequence, neurological ward consultations are commonly requested by the admitting medical teams to review diagnoses and management plans. The outcomes of neurological ward consultations were examined and the time required for the referral process recorded by performing a detailed prospective three-month audit of inpatient referrals to the neurology service. The consultations of 120 patients were recorded, categorised and analysed. These consultations were beneficial in the vast majority of cases, with a clear impact on patient diagnoses or management plans. The consultation process was time consuming, however, both in respect of the initial review, but also with follow-up visits. This audit highlights the importance of neurological input in the diagnosis and management of hospital inpatients. The time taken for this process should be resourced appropriately.
Key Words: inpatient consultation, job planning referral, workload
Introduction
Approximately 10% of patients seen in accident and emergency (A&E) departments and 10–20% of patients subsequently admitted to hospital have a primary neurological problem.1–3 The Association of British Neurologists (ABN) proposes that ‘a 24-hour neurological service should be available to all patients admitted with acute neurological illness and that all those who do not require immediate intervention should be seen within 24 hours’. The implementation of this proposal, with 24-hour on-site neurology, would require a significant expansion in the number of UK consultants from the current level of 620 to 1,403.4,5
Current government priorities are largely directed at reducing outpatient waiting times and it is likely that, for the foreseeable future, the majority of inpatients with acute neurological problems will remain under the care of physicians who are not neurologists. Neurological ward consultations – in which inpatients are reviewed to contribute to the diagnostic or management process – are commonplace, but the costs and benefits of the process have been subjected to only limited analyses. The process is likely to be time consuming for neurologists, detracting from other clinical duties, and the overall benefit of the consultation process is unclear. A prospective audit was therefore performed on inpatient neurological consultations to evaluate the characteristics of the consultations, the time taken for the process and the resultant outcomes.
Methods
The audit was performed at City Hospital, Birmingham, an 800-bedded teaching hospital, providing care for a population of over 250,000 people. The A&E department deals with 70,000 patients, with the hospital caring for 28,000 inpatients per year. Four consultant neurologists and two specialist registrars assist in the management of patients from a wide range of medical, surgical and allied specialties. At the time of the audit, neurological referrals were usually made by the admitting team, rather than directly from A&E. In addition, the hospital operated an independently functioning stroke unit, taking referrals with suspected strokes directly from the A&E department, for a typical inpatient stay of seven to 10 days. At the time of the audit (2005), the unit did not make distinctions based on patient demographics (young stroke, for example) and a thrombolysis service was not in operation.
An audit of inpatient referrals to the neurology service was performed over a three-month period (September through to November to avoid potentially atypical seasonal clusters of activity), with prospectively collected data for all ward referrals seen by one of four consultant neurologists. The accompanying data were either recorded by the relevant consultant or by the accompanying specialist registrar (MD). Basic patient demographics were collected, along with the initial working diagnosis from the referring team and the final diagnosis following the consultation and relevant investigations. Diagnostic categories were allocated according to the survey of Steiger et al.6 The time taken for the consult was recorded, approximating to the interval from the time at which notes were found on the ward, to the time for the notes to be returned to the ward, rounded up to the nearest five minutes. A significant proportion of patients required more than one visit, and this was recorded as above. At the end of the consultation process, all patient records were examined retrospectively to determine and verify the number of recorded neurological follow-up visits.
The outcome was also recorded and coded into previously established categories.7,6 In these, the neurologist:
makes a novel neurological diagnosis where no previous diagnosis existed
changes an incorrect diagnosis made by the referring physician
suggests an additional differential diagnosis or diagnoses and/or additional test to narrow down the differential diagnosis
suggests a treatment plan for the neurological condition.
Finally, if the consultation had no impact on patient management, the outcome was recorded as ‘no definite contribution’.
Results
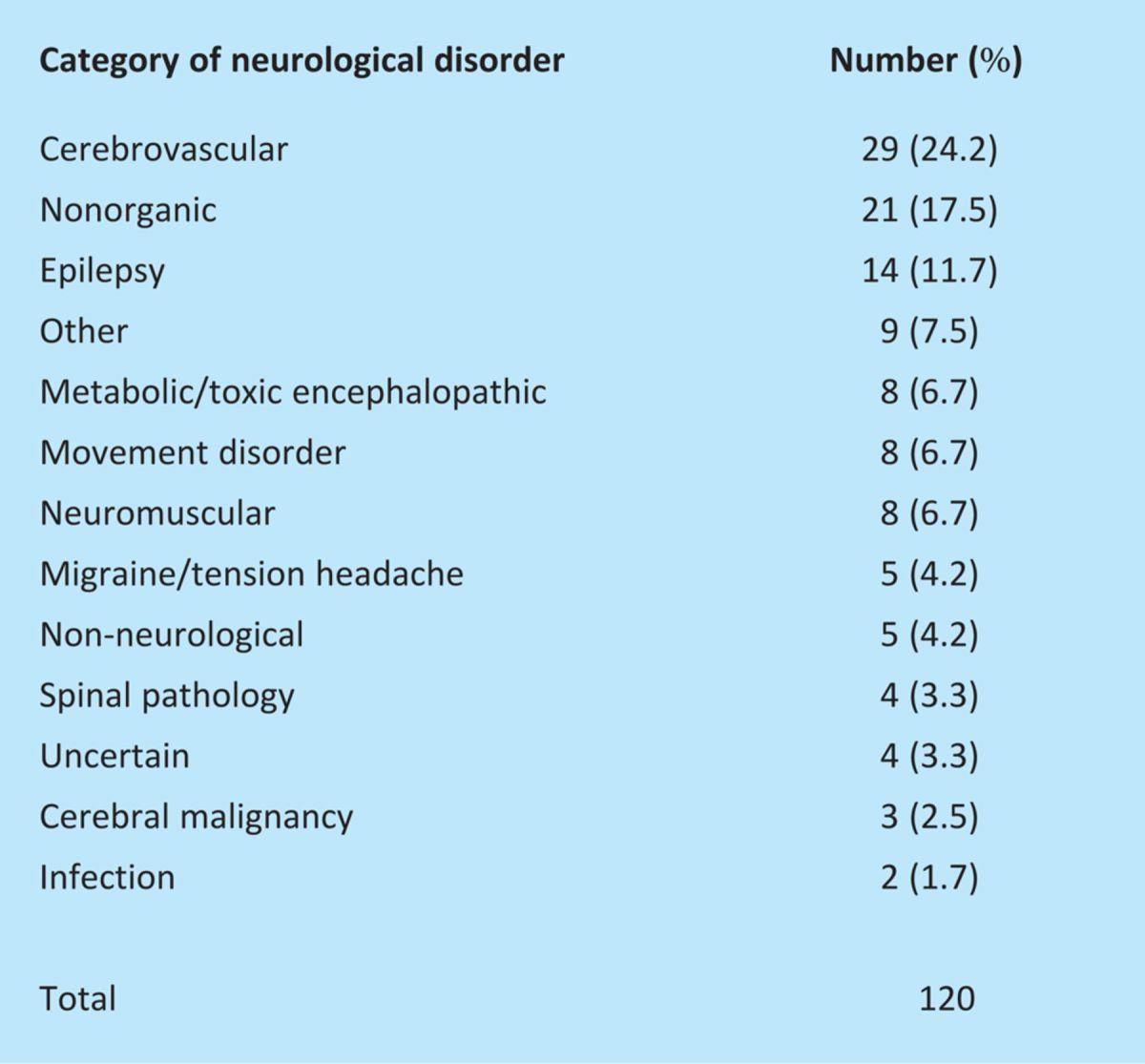
Seventy seven of the 120 patients were female (64%), with a mean age of 51.1 years (range 17 to 97). The diagnostic categories and relative numbers of patients are detailed in Table 1. Nine patients (7.5%) were allocated to the ‘other’ category, with diagnoses including multiple sclerosis (MS) relapses (4 patients), idiopathic intracranial hypertension (2), a diabetic sixth nerve palsy (1) and neurosarcoidosis (1). Cerebrovascular disease was the most common diagnostic category, accounting for 29% of cases seen. Nonorganic diagnoses were common (comprising 17.5% of cases), presenting either with functional hemipareses, parapareses or nonepileptic seizures. Non-neurological diagnoses included cases of anxiety or systemic infection. Of 120 patients, few had pre-existing established neurological diagnoses – epilepsy (7), MS (4), Parkinson's disease (3) and dystonia (1).
Table 1.
Number of patients according to the type of neurological disorder diagnosed.
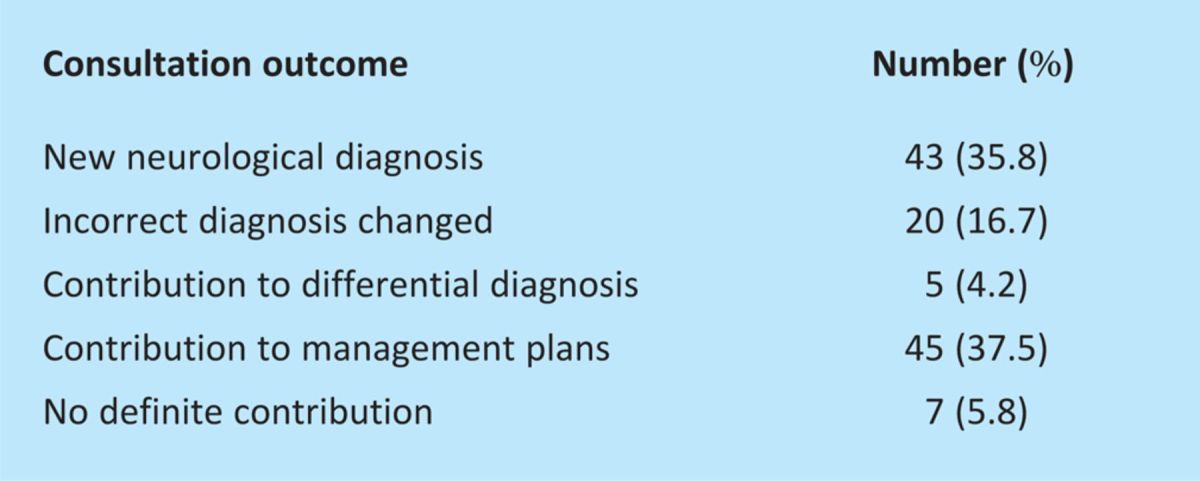
The contribution of the neurological consultation to the diagnostic and management process was determined (Table 2). New neurological diagnoses were made – where no diagnosis existed before – in 35.8% of patients and in 16.7% of cases an incorrect diagnosis was corrected. Contribution to the differential diagnosis and management plans were made in 4.2% and 37.5% of cases respectively.
Table 2.
Overall contribution of the neurological consultation.
The consultation time was collected prospectively for 104 (87%) initial visits, with a mean consultation time of 20.6 min (range 5 to 120 min). Consultation time was collected for 25 follow-up visits, with a mean time of 12.8 min per visit (range 10 to 25 min). Retrospective analysis of patient notes provided an indication of the total number of follow-up visits (216), giving a mean follow-up of 1.8 visits. An estimated total time for individual referral was therefore 20.6 + 12.8 × (1.8) = 43.6 minutes. Overall, neurologists reviewed patients promptly – for the patients surveyed and available data, 84 patients were seen within 24 hours, usually the same day (typically within four hours). Three were seen within 48 hours and two within 96 hours.
Discussion
A small number of prospective studies have examined the spectrum of neurological admissions to UK hospitals, with the earliest surveys finding that around 20% of adult medical admissions are primarily related to a neurological complaint. Most were admitted from primary care physicians or through the hospital A&E department. Only 8% of patients seen were subsequently transferred to a regional neurosciences centre,2 in part to gain access to neuroimaging facilities. In this survey of 180 cases, cerebrovascular disease and epilepsy formed the most important diagnostic categories, comprising 26% and 14% of cases respectively. Subsequent studies have broadly confirmed these findings.6,8 The patient characteristics seen in this survey are reasonably typical, with a broad range of ages, and a mean or median age around 50.2,6,8
As observed in previous studies, cerebrovascular disease continues to be the most common diagnostic category, despite the introduction of a dedicated stroke unit in the hospital. It was interesting that the nonorganic category formed a considerable group (17.5%) in this study, which was significantly higher than the 5.3% (9/169) seen in the 1996 survey conducted by Steiger et al.6 This was a similarly sized study and may reflect different population characteristics (based in North London rather than central Birmingham) or may be a consequence of a changing referral pattern which has evolved over the years between the studies. This latter possibility could be a consequence of changes in medical training, with the newer generation of consultants having trained through the Calman pathway and potentially having a more limited neurological exposure and/or confidence. Alternatively, it could reflect a more defensive medical attitude, with referrals driven with medicolegal concerns in mind. Finally, it could reflect a more inclusive attitude towards neurological colleagues, particularly as consultant numbers and inpatient ‘visibility’ have increased significantly over the past decade.
This study confirms that ward consultations continue to be clearly beneficial – to both patients and the referring team. The earliest study on this topic, based in the Royal Free Hospital in London in a 1995 survey of 169 patients, found that neurological consultations led to novel diagnoses in 15% and changed existing diagnoses in 18% of patients. A number of studies have found similar benefits in both neurological and non-neurological (medical and surgical) contexts, with specialists providing more comprehensive evaluations, leading to significant increases in diagnostic accuracy and consequently better patient management.9,10,11 Early specialised neurological input also leads to shorter inpatient times, with a study finding a reduction in the median length of stay from six to three days following the introduction of a liaison neurology service.12
Neurological ward consultations are therefore clearly beneficial, but the cost of the activity is unclear. Although some components of the workload of a neurologist can be monitored easily, such as measuring the number of outpatients (new and follow-up) and inpatients seen, workload by inpatient referral is typically ‘invisible’.11 This survey suggests that the total time per patient is around 45 minutes, roughly corresponding to the time taken for two new outpatient slots. It is likely to be an underestimate, of course, as this does not include the time taken finding the patient, retrieving investigation results and discussing issues with relevant colleagues.
Consultant job plans typically allocate one or two sessions per week to these activities, but it is not clear how this is decided upon. It should probably be a correlate of the number of inpatients with neurological disorders factored to the number of consultant neurologists for that hospital. There are reasonable studies detailing the patients admitted with acute neurological conditions and, for the foreseeable future, these patients will be cared for by non-neurologists and this activity will continue to be important, beneficial and is likely to be extremely cost effective.
These factors may change over time, however, with increased access to neurological advice potentially changing the pattern of referrals. This is clearly demonstrated in a recent publication detailing the use of a web-based inpatient neurological referral system. This approach increased the quality of referrals, but led to a significant (60%) increase in their number.13 Alterations to medical training, with more limited general medical and neurological exposure, are almost certain to increase the need for specialised neurological input. Data from this survey suggest that the presence of a specialised stroke unit in a hospital does not lead to a significant change in the pattern of referrals seen.
In conclusion, this study finds that inpatient neurological consultations lead to significantly improved patient diagnostic and management plans. The process is, however, time consuming and should be resourced appropriately.
References
- 1.Hampton JR, Gray A. The future of general medicine: lessons from an admissions ward. J R Coll Physicians Lond 1998;32:39–43 [PMC free article] [PubMed] [Google Scholar]
- 2.Morrow JI, Patterson VH. The neurological practice of a district general hospital. J Neurol Neurosurg Psychiatry 1987;50:1397–401 10.1136/jnnp.50.11.1397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Playford ED, Crawford P, Monro PS. A survey of neurological disability at a district general hospital. Br J Clin Pract 1994;48:304–6 [PubMed] [Google Scholar]
- 4.Carroll C, Zajicek J. Provision of 24 hour acute neurology care by neurologists: manpower requirements in the UK. J Neurol Neurosurg Psychiatry 2004;75:406–9 10.1136/jnnp.2003.018010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butcher J. UK neurology: the Blair years. Lancet Neurol 2007;6:670–1 10.1016/S1474-4422(07)70183-7 [DOI] [PubMed] [Google Scholar]
- 6.Steiger MJ, Enevoldson TP, Hammans SR, Ginsberg L. Influence of obtaining a neurological opinion on the diagnosis and management of hospital inpatients. J Neurol Neurosurg Psychiatry 1996;61:653–4 10.1136/jnnp.61.6.653-a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hillen ME, Sage JI. Proving the worth of neurologists. Neurology 1996;46:276–7 10.1212/WNL.46.1.276 [DOI] [PubMed] [Google Scholar]
- 8.Weatherall MW. Acute neurology in a twenty-first century district general hospital. J R Coll Physicians Edin 2006;36:196–200 [Google Scholar]
- 9.Bala C, Poon AC, Joblin P, McCluskey PJ. Ophthalmologists in teaching hospitals: do we make a difference to patient outcome?. Clin Experiment Ophthalmol 2001;29:59–63 10.1046/j.1442-9071.2001.d01-4.x [DOI] [PubMed] [Google Scholar]
- 10.Braiteh F, El Osta B, Palmer JL, Reddy SK, Bruera E. Characteristics, findings, and outcomes of palliative care inpatient consultations at a comprehensive cancer center. J Palliat Med 2007;10:948–55 10.1089/jpm.2006.0257 [DOI] [PubMed] [Google Scholar]
- 11.Koh CE, Walker SR. Vascular surgery consults: a significant workload. ANZ J Surg 2007;77:352–4 10.1111/j.1445-2197.2007.04058.x [DOI] [PubMed] [Google Scholar]
- 12.Forbes R, Craig J, Callender M, Patterson V. Liaison neurology for acute medical admissions. Clin Med 2004;4:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ali E, Chaila E, Hutchinson M, Tubridy N. The ‘hidden work’ of a hospital neurologist: 1000 consults later. Eur J Neurol 2010;17:e28–32 10.1111/j.1468-1331.2009.02901.x. [DOI] [PubMed] [Google Scholar]


