Introduction
Hajj is one of the five pillars of Islam and is obligatory for all adult Muslims who can afford the journey and are in good health. Hajj is the Arabic word for pilgrimage; it commemorates the patriarch Abraham's readiness to sacrifice his son Ishmael in Biblical times. Over two million pilgrims gather from different nationalities to perform pilgrimage in Saudi Arabia, and more than 20,000 Britons do the Hajj each year,1 most from south Asian origin with a high prevalence of diabetes. Most healthcare professionals in the west are unaware of what the Hajj entails or its associated health risks and typically find it difficult to offer an informed opinion. This article deals with the effects of this event on diabetes and its management and explains the Hajj journey and the possible associated health hazards.
The rites of Hajj
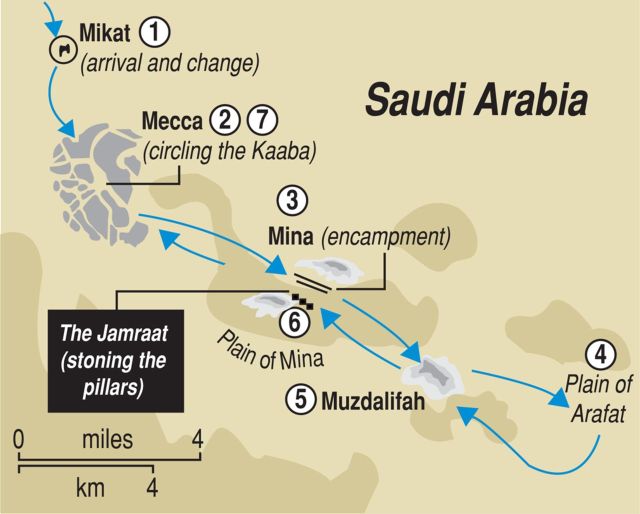
Hajj involves travel to the holy sites in Saudi Arabia (in and around Mecca and Medina) during a specified short period of time (Fig 1). It lasts for five days and, as the Islamic calendar is lunar, the precise dates on the Gregorian calendar will vary each year. Hajj is the most complex of the Islamic rituals and involves, among other things, walking long distances and camping in desert tents.2 Central in these activities is the pilgrim's presence on the desert plain of Arafat, from noon until sundown. There, dressed in the simplest possible clothing, pilgrims will spend much of the day standing in humility and prayer. Because of the large numbers of people, performing even the simplest rites can take an extraordinary length of time.
Fig 1.
Hajj journey.
Health hazards during Hajj
The Hajj duties can be demanding in terms of physical activities and mental effort. People performing it may be preoccupied by the religious rituals and self-management may be neglected. This may be further complicated by the language barrier making it difficult to access medical services when necessary. Furthermore a significant proportion of those performing Hajj are elderly and may suffer from chronic medical conditions, which may be aggravated during Hajj.3
Recorded temperatures during Hajj range between 37°C and 45°C.4 Overcrowding and the hot climate subject the pilgrims to environmental and health hazards. Specific risks during Hajj include intercurrent illness including upper respiratory tract infections and diarrhoea, heat stroke, dehydration and electrolyte imbalance, lack of adequate supply of medication and limited access to specialist medical care facilities.5 During Hajj, the person's life routine changes as they travel through places where the geography, weather, diet and habits are different, therefore medical condition, such as diabetes, which depend on a stable routine would predictably be significantly affected. Increasingly, diabetes has been reported as a leading cause of morbidity and mortality during Hajj.6 In a recent study, 31.9% of a total of 689 patients admitted as an emergency had diabetes.3
Diabetes-related clinical problems during Hajj
Hyperglycaemic emergencies
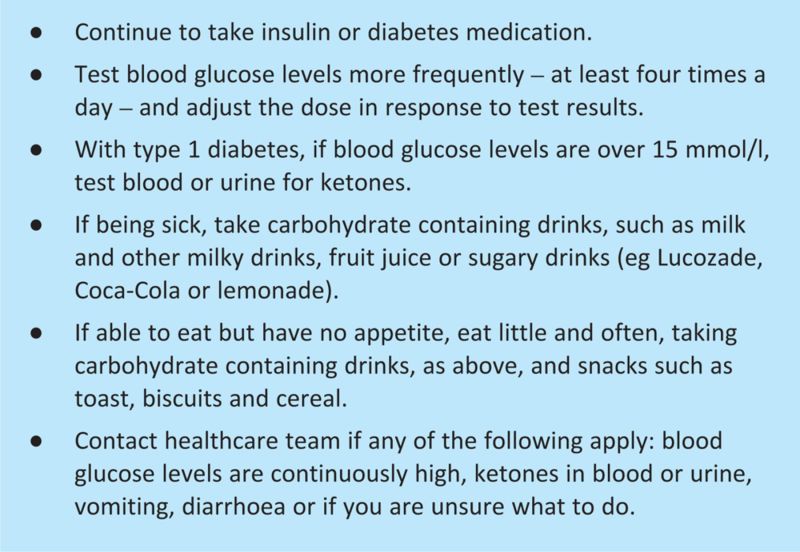
Intercurrent illnesses and lack of adequate insulin/medications predictably precipitate hyperglycaemic complications such as diabetic ketoacidosis or hyperglycaemic hyperosmolar state. Respiratory infections are known precipitating factors for hyperglycaemic crisis, people with diabetes should be annually vaccinated against influenza and it should be a priority in those attending Hajj. This has been asserted in the official Saudi health check directives for 2007. In a prospective study of all diabetic ketoacidosis admitted to a single hospital, 18 episodes were examined; all but one was during Hajj. Poor concordance with treatment was the precipitating factor in 94%, mortality rate was 5.6%.7 If any illness occurs, diabetes control will need careful monitoring and sick day rules should be applied (Box 1). Patients should continue to take their insulin regularly and should seek medical advice urgently if any symptoms or signs of diabetic ketoacidosis arise. People with type 2 diabetes who are on tablets may need insulin temporarily during acute illnesses.
Box 1. Sick day rules.
Hypoglycaemia during Hajj
Hypoglycaemic episodes are common during Hajj as a result of increased physical activities.8 Insulin doses which may be optimal during sedentary life prove excessive during Hajj due to the loss of normal routine of balanced diet to match a strenuous exercise. Similarly preference for performing prayers in the holy shrines may delay meal times contributing to hypoglycaemia. It may be necessary to advise the well-controlled diabetic patient to reduce the dose of oral hypoglycaemic agent or insulin as they are likely to be exercising the equivalent of two hours or more every day.9 Insistence on regular meals and taking mid-morning snacks is also important. People on twice daily mixture insulin may need to consider changing to basal bolus regime to allow flexibility. Excessive heat during the summer months may enhance insulin absorption and produce hypoglycaemia, although it may conversely interfere with insulin storage and cause hyperglycaemia. If sickness or diarrhoea develops, patients can substitute solid foods with carbohydrate containing fluids, they should never stop insulin even if they can not tolerate solid food. Blood glucose levels should be monitored frequently and insulin doses adjusted as appropriate. If sickness and or diarrhoea persist, medical advice should be sought. If using an insulin pump, basal rate may need to be reduced to allow for the effect of excess exercise.
Foot problems
Diabetic foot was one of the most common causes for admission to a surgical ward over two consecutive years' study.10 Cracking of the skin is common and it can cause deep fissures resulting in pain and discomfort with the possibility of a developing infection. A good moisturizer applied two or three times a day starting as soon as possible after arrival in Arabia will help the skin retain moisture.11 Most pilgrims travel on foot. In one study, movement between holy places amounting to 5–15 km was made on foot in 40% of those studied, by bus or car in 31%, or a combination of both in 29%12 so good quality footwear is essential. Foot burns can be sustained during summer due to high ground temperature that can reach 50–60°C. Patients with diabetic neuropathy or peripheral vascular disease are at particularly increased risk often compounded by the problems of poor healing and the increased risk of infection. Twelve cases of foot burn sustained from standing or walking barefoot on the street were reported. All injuries occurred during the summer months. Eight out of the 10 adults had diabetes with significant peripheral neuropathy.13 Care needs to be taken to avoid walking barefoot at all times because of the serious risk of burns to the foot.
Minor injuries are relatively common, particularly to the toes: these typically result from inadvertently being stamped on while circling the Ka'bah barefoot.14 Skin infections (bacterial and fungal) are more common in patients with poorly controlled diabetes.15
Renal and cardiovascular disease
Renal failure and heatstroke during the summer are the main reasons for hospital admissions.16 During the summer months, the temperature can go above 50°C, patients with diabetic nephropathy must make every effort to avoid dehydration and carry water bottles with them at all times. They should drink two or more litres of water daily depending on the weather. In cases of diarrhoea or vomiting they should seek medical help to ensure that dehydration is corrected promptly thus avoiding any deterioration of renal function. They should not self-prescribe as some medication might affect renal function adversely. If a patient is taking a diuretic regularly, the dose may need to be reduced to avoid dehydration.
Many diabetic patients will have asymptomatic coronary artery disease, hence a pre-travel electrocardiogram is advisable with clear instruction to present to a health facility as soon as possible if chest pain, shortness of breath, or palpitations arise. Reduction in cardiovascular mortality has been reported by formal assessment and management before Hajj.17 The diabetic hypertensive patient must try to control their blood pressure before travel and an attempt should be made to take into account the control during exercise. They should also be advised to either self-monitor or go to the country health mission and check their blood pressure regularly.
The ‘travel Hajj consultation’
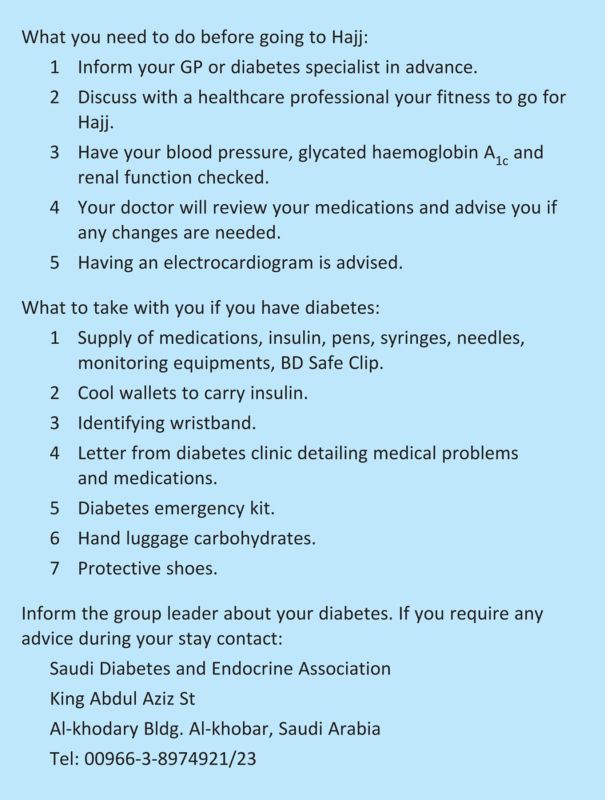
People with diabetes who are going for Hajj should have enough time to discuss it with a healthcare professional and to consider a management plan for their diabetes (Box 2). Several diabetes units in the UK are now holding pre-Hajj education seminars.18 A religious dispensation exists for those in poor health and many will make use of this allowance after consultation with their doctor.19
Box 2. Diabetes Hajj checklist.
Travellers should take sufficient supplies of their usual drugs and also carry a written record, giving the generic names in case further supplies are needed. Adequate supply of needles, pens and monitoring instruments is essential. Travellers should be strongly encouraged to wear identifying wristbands and to take protective shoes.
Due to the recent increase in airport security it is important that patients have a letter from their diabetes clinic confirming the diagnosis of diabetes in order for them to be allowed to carry needles and syringes in their hand luggage. Furthermore, a letter documenting medical problems and drugs will allow rapid assessment should an illness occur. Pharmacies in Arabia do not require prescriptions for certain medications making them easily accessible to the millions of people that travel there, without the need to see a doctor.11
Those who intend to perform Hajj during summer are likely to suffer problems unless they are warned and educated. Reduction in mortality has been reported by formal assessment and management before Hajj.17
Storing insulin and the diabetes emergency kit
Insulin should not be put in the luggage hold of the aircraft as it may freeze and should instead be handed to the aircrew to keep refrigerated. Once in Saudi Arabia, insulin should be refrigerated but not in the freezer compartment. While moving around in hot places insulin could be stored in special cool wallets and kept away from direct sunlight. Extra care should be taken as some blood glucose tests strips may over heat in very hot weather.
People who are treated with insulin or sulphonylurea should carry a diabetes emergency kit at all times; the kit should contain Glucogel with instruction to rub on the patient's gums if they are found unconscious. It must also contain glucagon for ready use in insulin-treated patients.
Summary
Keeping well during Hajj is a challenge for people with diabetes. However, with proactive planning and education, it may prove to be an excellent opportunity for reviewing management and enhancing diabetes education to reduce diabetes-related short- and long-term problems. People with diabetes should have enough time to consider a management plan. It is important that healthcare professionals are well informed regarding the effects of Hajj on diabetes and are able to offer advice, guidance and change of medications as required during pre-Hajj counselling to enable patients to stay healthy.
References
- 1. Muslim Council of Britain, www.mcb.org.uk.
- 2.Sarwar G. Islam: beliefs and teachings. London: George Allen and Unwin, 1985:242. [Google Scholar]
- 3.Khan NA, Ishag AM, Ahmad MS. Patterns of medical diseases and determinants of prognosis of hospitalisation during 2005 Muslim pilgrimage Hajj in a tertiary care hospital. Saudi Med J 2006;27:1373–80. [PubMed] [Google Scholar]
- 4.Minesh SA, Al-Khenaizan S, Memish ZA. Dermatologic changes of pilgrimage. Clin Dermatol 2008;26:52–61 10.1016/j.clindermatol.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Madina TA, Ghabrah TM, Al-Hedaithy MA. Causes of hospitalisation of pilgrims in the Hajj season of the Islamic year 1423(2003). Ann Saudi Med 2006;26:346–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Turki A. general guidelines for people with diabetes intending to perform Haj. IDF Bulletin 1998;43:25–70. [Google Scholar]
- 7.Yusuf M, Chaudhry S. Diabetic ketoacidosis in pilgrims visiting Madina Al-Munawarah, Saudi Arabia. Intern Diabetes Digest 1998;8:14–16. [Google Scholar]
- 8.Khan SA, Bhat AR, Khan LA. Hypoglycaemia in diabetes during Hajj. Saudi Med J 2002;23:1548. [PubMed] [Google Scholar]
- 9.Beshyah SA, Sherif IH. Care for people with diabetes during the Moslem Pilgrimage (Hajj). An overview. LJM 2008;3:39–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Salamah SM. General Surgical problems encountered in the Hajj pilgrims. Saudi Med J 2005;26:290–2. [PubMed] [Google Scholar]
- 11.Hajj health guidelines. www.salaam.co.uk/hajj/HEALTH_GUIDELINES.pdf.
- 12.Baomer AA, el Bushra HE. Profile of diabetic Omani pilgrims to Mecca. East Afr Med J 1998;75:211–4. [PubMed] [Google Scholar]
- 13.Al-Qattan MM. The ‘Friday Mass’ burns of the feet in Saudi Arabia. Burns 2000;26:102–5 10.1016/S0305-4179(99)00097-2. [DOI] [PubMed] [Google Scholar]
- 14.Gatrad AR, Sheikh A. Hajj journey of a lifetime. Student BMJ, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samdani AJ. Spectrum of skin disorders presenting to king abdul Aziz Hospital during Hajj season 2000. J Ayub Med Coll Abbottabad 2004;16:10–3. [PubMed] [Google Scholar]
- 16.Madani Tj, Ghabrah TM, Al-Hedaithy MA, et al. Causes of hospitalisations of pilgrims in the Hajj season of the Islamic year 1423(2003). Ann Saudi 2007;27:101–5 10.4103/0256-4947.51528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Afshin-Nia F, Dehkordi HM, Fazel M, Ghanei M. How to reduce cardiovascular mortality and morbidity among Haj pilgrims: a multiphasia screening, intervention and assessment. Ann Saudi Med 1999;19:55–7. [DOI] [PubMed] [Google Scholar]
- 18.Figueira E. Diabetes and the pilgrimage of Haj: piloting of an education programme for muslim patients with diabetes. Diabetes Today 2003;6:41–2. [Google Scholar]
- 19.Sabiq AS. Figh us-sunnah: Hajj and Umrah. Indianapolis: American Trust Publications, 1992:5. [Google Scholar]