Abstract
Although telephone consulting is increasingly used by clinicians seeking to balance rising caseloads, heightened patient expectation and the desire to ensure continued improvements in the quality, convenience and accessibility of the care they provide, its use to provide care to renal transplant recipients has not previously been described. Climate change is a major global public health threat. However, the provision of healthcare itself has a significant environmental impact. A transformation to lower carbon clinical care must be achieved without detriment to the quality of the patient care. This article reports the use of telephone consultation clinics to provide follow-up to renal transplant recipients over a three-year period. The benefits of this service to patients, providers and the environment are outlined, the existing literature regarding the provision of virtual care to patients with kidney disease is reviewed, and the possibilities of more widespread adoption are discussed
Key Words: climate change, renal transplant, telephone clinic
Introduction
Telephone consulting offers clinicians a means by which to meet the challenge of improving quality and accessibility despite rising caseloads and heightened patient expectation.1 It is now utilised to triage patients, manage acute and chronic conditions, enhance compliance and communicate results. When used appropriately, telephone consulting offers the patient and clinician multiple benefits, including enhanced access to healthcare, heightened continuity of care, reduced travelling and considerable time savings.
Climate change has been described as ‘the biggest global health threat of the 21st century’.2 However, the provision of healthcare itself has a significant environmental impact; the carbon footprint of NHS England is 21.2 MtCO2 eq per year.3 Telephone consulting offers the further benefit of reducing the 18% of emissions attributable to patient and staff travel. 3
UK guidelines do not offer a follow-up timetable for stable renal transplant recipients, although most services offer three- to six-monthly appointments. This is in keeping with the guidance of the American Society of Transplantation, which notes that there are virtually no scientific data on which to base decisions regarding the optimal frequency (or type) of follow-up of these patients.4 This article reports the use of telephone consulting to provide three-monthly follow-up to renal transplant recipients in a single UK renal unit over a three-year period.
Case study
The University Hospital of Coventry and Warwickshire (UHCW) renal service began to offer telephone consultations to provide routine follow-up to renal transplant recipients in 2006. The service now provides approximately 350 appointments per year, facilitating follow-up to 123 of the 360 patients in whom transplantation was undertaken more than one year previously.
The service is offered to patients at their physician's discretion. Most patients are well known to the department and all must have demonstrated stable graft function. Patients receive quarterly clinic appointments, of which one remains a face-to-face consultation. Consultations commence with the patient ringing through to the clinician at a time detailed in their appointment letter, which also requests that they provide their weight and blood pressure readings. As with face-to-face consultations, blood tests are undertaken beforehand; patients may attend their family practice, the city centre phlebotomy service or their local hospitals. Fifteen minutes are allocated per consultation. Clinic letters are copied to the patient, along with any necessary prescriptions, a blood test form and their next appointment details. The annual face-to-face consultation allows for physical examination (including urinalysis).
The authors believe that this is the only service of its nature in the UK. Informal feedback from patients suggests high levels of satisfaction. To date, only two patients have opted to return to face-to-face follow-up. There have been no reported patient safety issues.
Discussion
Telephone consulting has mainly been used to manage the demand for care, predominantly out-of-hours and within the emergency department and primary care settings (where more than half of out-of-hours calls can be handled by telephone advice alone).5,6 Telephone consulting in other services is less well researched. No reports of telephone-based care for renal transplant recipients were found, although telemedicine for dialysis patients has been described.77–9 Videoconferencing can facilitate routine consultations between nephrologists and dialysing patients.7 Telemedicine offers haemodialysis and peritoneal dialysis patients improved access, reduced costs and travel savings.10
The few studies assessing patients' and clinicians' perceptions of telephone clinics are limited to primary care. In one study, both groups considered telephone consultations to be convenient, and to be best suited to the management of chronic conditions.11 In another study, patients with chronic diseases managed by telephone care changed their perceptions such that, at the end of the two-year study, they believed that telephone consultations could be used to manage their conditions.12
The benefits of telephone consulting
High quality healthcare should be safe, timely, effective, efficient, equitable, patient-centred and sustainable. While the model of care reported here delivers in each of these domains, it offers particular improvements in efficiency, sustainability and patient-centred care.
Patient-centred, convenient care
Many patients who have undergone a transplant have previously attended the hospital (for example, for dialysis) with a very high frequency for many years. It is the experience of the authors that these patients perceive a positive health gain from telephone consultations. While this may simply reflect the improved convenience, the authors consider this health gain to be predominantly attributable to heightened patient empowerment resulting from the telephone clinic model. Patient empowerment is a key component to the successful management of chronic disease. More research to determine the nature of this under-recognised benefit of telephone consulting is required. RenalPatientView,13 an existing patient empowerment tool, would compliment the use of telephone consultations.
It is estimated that 25% of patients would have taken time off work to attend face-to-face appointments but participated in telephone consultations without doing so. In contrast, the proposal of evening or weekend clinics has been poorly received by patients.
This study showed that patients prefer to ring the clinic than be rung, as this negates the need to advise where they will be in advance. The financial cost of their call is usually more than offset by savings in fuel costs and parking. Furthermore, offers to consult by email have been declined, perhaps indicating the value patient's place upon direct communication.
Safe care
Clinicians familiar with face-to-face consultations may question the safety of telephone consultations, an area in which robust evidence is lacking. While a review of telephone-related malpractice suits determined that patient safety is compromised mainly when consultations include diagnostic or triaging components,14 there is evidence that their use in the provision of routine follow-up is safe.12 A systematic review of the literature found no increase in adverse effects or use of other services.15
The care of patients receiving immunosuppression should encompass vigilance for skin lesions, and patients followed by telephone consultation should receive regular education around this. In the UHCW service, those patients reporting lesions and who do not already have open access to the dermatology service are advised to seek an urgent dermatology referral through their general practitioner under the ‘two-week wait’ system.
One randomised controlled trial, involving 497 patients with chronic diseases being managed in primary care, is of particular note.12 Follow-up in a traditional clinic was compared against follow-up in which the recommended interval for face-to-face time was doubled and three intervening telephone consultations were arranged. Telephone-care reduced utilisation of medical services without adversely affecting patient-reported health. Telephone-care patients had fewer scheduled and unscheduled clinic visits than usual-care patients, and fewer and shorter hospital admissions. The estimated expenditure of their care was 28% less in the telephone-care group. When new or worsening problems were uncovered during a telephone consultation, the patient was seen at the clinic or admitted to hospital in a timely fashion. The patients' diagnoses and demographics, and the degree of continuity of care, were similar across the two groups. This study therefore suggests that the increased communication afforded by more frequent contact may be the determinant of the underlying health benefits of telephone care.
Sustainable care
The provision of healthcare is associated with greenhouse gas emissions and contributes to climate change,3 which in turn represents a major threat to global health.2 Patient travel contributes to the carbon footprint of a renal service,16 but the potential reductions attributable to telephone consulting have not previously been studied. The reduction in greenhouse gas emissions associated with the UHCW telephone clinic model was therefore examined.
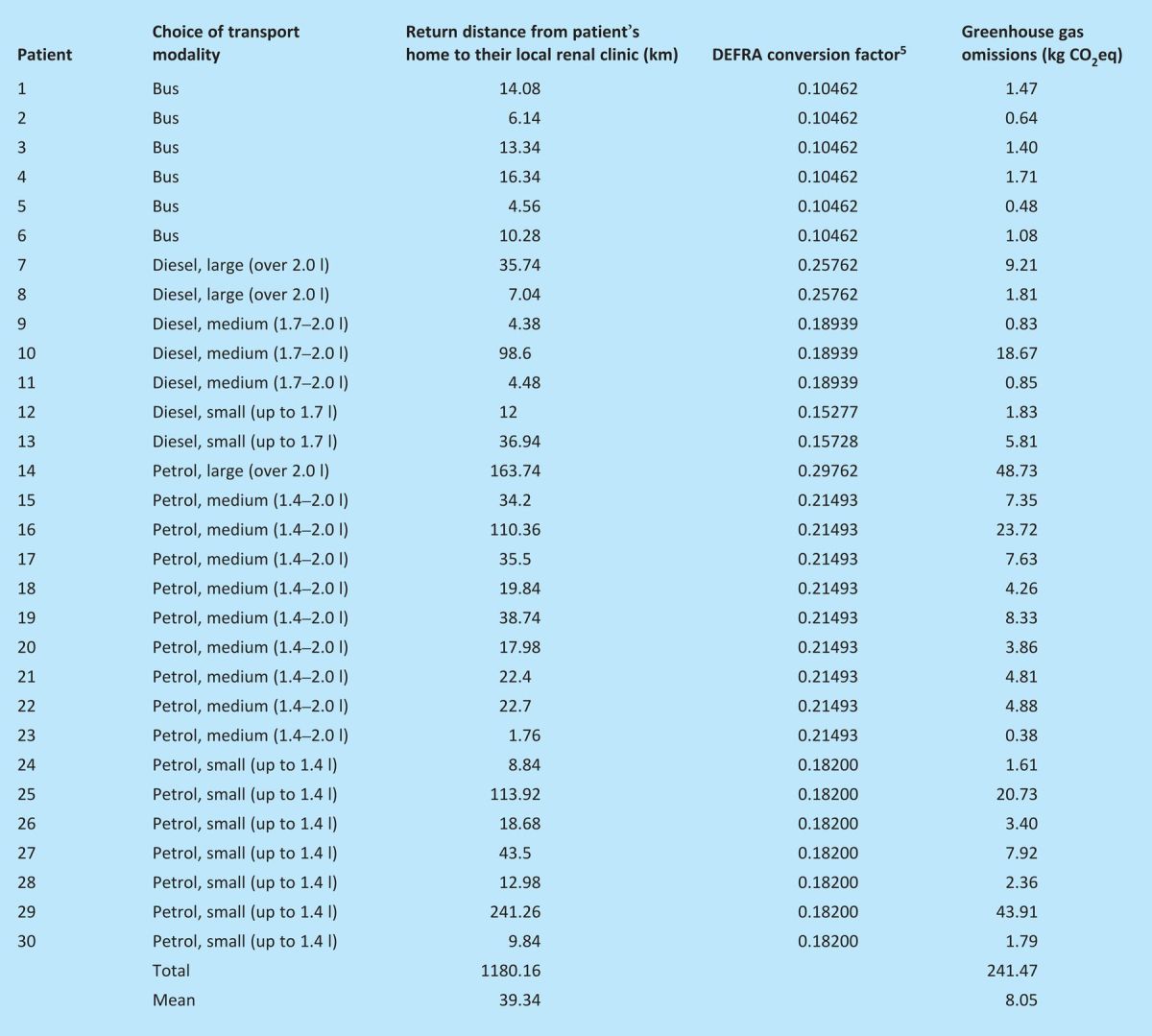
Data were collected prospectively from 30 patients attending two consecutive telephone clinics. It was assumed that, had patients attended a face-to-face clinic, they would have travelled from, and returned to, their homes. Each patient's return journey length was calculated from their postcode using Google Maps. Had these patients attended clinic, they would have travelled a total of 1180.10 km (mean 39.34 km, range 1.76–241.26 km), with only 64.74 km (5.8%) undertaken by public transport (Table 1). The greenhouse gas emissions arising from each patient's travel were calculated using DEFRA conversion factors specific to the transport modality that they would use to attend their local clinic.17 A mean value of 8.05 kg carbon dioxide equivalents (kgCO2eq) was identified. The annual 350 telephone consultations therefore result in an estimated reduction in greenhouse gas emissions of 2,818 kgCO2eq.
Table 1.
Prospectively collected data from two consecutive telephone consultation clinics
Further reductions (and time savings) result from reduced physician travel to outlying clinics as an estimated annual total of 20 clinics across two sites (Stratford and Warwick) became redundant. Assuming that the physician would have undertaken return journeys from the UHCW site by car, this further annual reduction in greenhouse gas emissions amounts to ([10 × 0.20487 × 2 × 20.4] + [10 × 0.20487 × 2 × 36.2]) 231.8 kgCO2eq (where 20.4 and 36.2 are the return distances to the outlying clinics, in km, and 0.20487 is the conversion factor for an average sized car17).
Further potential, but probably less significant, carbon savings result from the reductions in building energy use (for example, the lighting and heating requirements of a hospital waiting room) and in associated staff commuting (for example, outpatient nurses and reception staff). The overall annual carbon saving is therefore estimated to be well over three tonnes CO2eq (a volume of greenhouse gases sufficient to fill three large detached houses).
Setting up a telephone consultation service
Potential disadvantages and barriers
Telephone consultation is not appropriate when formal physical examination is a likely necessity. Its role is primarily in the management of established chronic disease, rather than where diagnostic evaluation is required. Even during follow-up, one clear drawback of telephone consulting remains the loss of visual clues to a patient's well-being.11 A thorough history is therefore important and familiarity with the patient must not be considered a substitute for this.
Cultural barriers, as well as logistical and administrative challenges, may present potential barriers to effective implementation of telephone services. For example, the clinician might ideally wish to control the process by which patients organise their subsequent appointment, a duty which previously would have been undertaken by the outpatient receptionist, in order to include the information in the clinic letter (the patient copy of which also acts as the appointment letter). Similarly, patients might find automatically generated reminder letters asking them to ‘attend’ clinics confusing; such letters should be tailored to the telephone service.
Patient selection
The UHCW service does not currently adhere to firm criteria regarding patient selection. However, the spectrum of patients to whom the service is offered has broadened as a result of positive feedback from participating patients and the increasing experience and confidence of the physicians. When the service is offered to patients, its optional nature – and the opportunity to return to face-to-face clinics at any stage – is emphasised. The service is only offered to patients with stable graft function (experience indicates a 12-month period to be sufficient). Those with complex co-morbidities, or in whom regular physical examination is a likely necessity, are less likely to be suitable.
Telephone consultations are less appropriate for patients with hearing, speech or cognitive impairment, or if a language barrier exists. Patients should ideally be well known to the department and the clinician providing telephone follow-up; both clinicians and patients place greater confidence in telephone consultations when a face-to-face relationship already exists.11 Experience suggests that telephone consultations are not well suited to managing patients with poor attendance records in face-to-face clinics, as they are also likely to be poorly compliant with telephone clinics (seven such patients have been discharged back to face-to-face follow-up from the UHCW service).
Funding
Acute trusts are rewarded for their services through the payment by results (PbR) system. Guidance on the application of PbR to non-face-to-face outpatient activity is provided in clauses 344–346 of the PbR guidance for 2011/12.18 A face-to-face consultation in kidney care commands a tariff of £128, while the tariff for all non-face-to-face activity is £23. This is derived from the average of the reference costs reported annually across all specialties. As such, it is quite possible that this figure does not reflect the true financial cost of any given non-face-to-face consultation, particularly as such activity may range from a short phone call from a junior staff member to a video-conference with a senior staff member. It is therefore important to note that the tariff for non-face-to-face activity is designated as non-mandatory and can be negotiated with primary care trust commissioning bodies.
Although beyond the scope of this report, a full economic analysis is therefore required, and should consider the changes to the staff workloads; for example, that of the outpatient department nursing staff is reduced, while that of the administration team will remain unchanged or may even increase. It might also include the implications for patients (who save on travel costs and from not taking time off work) and for trusts (for example, the trust may incur costs for blood tests undertaken elsewhere, while suffering a loss in car park revenue).
Wider implications
On 31 December 2007, there were 21,132 adults with functioning renal transplants in the UK.19 Accepting the inaccuracies resulting from geographically and demographically related differences in the distances and modalities of outpatient travel, and assuming that patients would otherwise be seen quarterly, it is estimated that if the care of 30% (6,340) of these patients were to be provided by telephone clinic model, an annual carbon saving of (6340 × 3 × 8.05) over 150 tonnes CO2eq might be realised.
The UHCW service currently provides follow-up to seven patients with stable chronic kidney disease (CKD), a condition which is also well suited to follow-up by telephone consultation. The age standardised prevalence of stage 3–5 CKD within the UK has been estimated at 8.5%, but the condition remains largely under-recognised (only 2.1% of patients with stage 3–5 CKD had a coded diagnosis of renal disease).20 The proportion of patients diagnosed with CKD is anticipated to rise, due in part to the provision of national guidance.21 Telephone consulting may become an important component of the service reconfiguration that would be required for current renal services to meet this increased demand.
Furthermore, as telephone consulting is well suited to the follow-up of patients with stable chronic conditions, its widespread adoption across different specialties (for example, to provide follow-up to patients with diabetes or heart failure) offers considerable benefits to patients and the environment.
Conclusion
Experience suggests that, implemented appropriately, the use of telephone consulting for the follow-up of renal transplant recipients is safe, empowers patients, improves access to healthcare and confers environmental benefits. More research is required to better understand the attitudes of patients to these clinic models and to validate their safety.
The NHS Next Stage Review has outlined the need to embed quality into the NHS through service change and innovation.22 Such reconfigurations, across all specialties, present an opportunity to contribute to the carbon reductions required for the NHS to meet its target of 10% less emissions by 2015.23 While the current economic climate has understandably focused consideration upon the financial impacts of reconfigurations, it is advocated that the environmental impacts of possible alternative service changes should also be evaluated and lower carbon options embraced.
References
- 1.Car J, Sheik A. Telephone consultations. BMJ 2003;326:966–9 10.1136/bmj.326.7396.966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet 2009;373:1693–733 10.1016/S0140-6736(09)60935-1 [DOI] [PubMed] [Google Scholar]
- 3.Sustainable Development Commission. (2008) NHS England carbon emissions: carbon footprinting study. London: Sustainable Development Commission, 2008. [Google Scholar]
- 4.Kasiske BL, Vazquez MA, Harmon WE, et al. Recommendations for the outpatient surveillance of renal transplant recipients. American Society of Transplantation. J Am Soc Nephrol 2000;11(Suppl 15):S1–86 [PubMed] [Google Scholar]
- 5.Christensen M, Olsen F. Out of hours service in Denmark: evaluation five years after reform. BMJ 1998;316:1502–5 10.1136/bmj.316.7143.1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction (Review). Cochrane Database Syst Rev 2004;(4):CD004180. [DOI] [PubMed] [Google Scholar]
- 7.Whitten P, Buis L. Use of telemedicine for haemodialysis: perceptions of patients and health-care providers. J Telemed Telecare 2008;14:75–8 10.1258/jtt.2007.070411 [DOI] [PubMed] [Google Scholar]
- 8.Mitchell BR, Mitchell JG, Disney AP. User adoption issues in renal telemedicine. J Telemed Telecare 1996;2:81–6 10.1258/1357633961929835 [DOI] [PubMed] [Google Scholar]
- 9.Rumpsfield M, Arild E, Norum J, Breivik E. Telemedicine in haemodialysis: a university department and two remote satellites linked together as one common workplace. J Telemed Telecare 2005;11:251–5 10.1258/1357633054471885 [DOI] [PubMed] [Google Scholar]
- 10.Jennett PA, Afflect Hall L, Hailey D, et al. The socio-economic impact of telehealth: a systematic review. J Telemed Telecare 2003;9:311–20 10.1258/135763303771005207 [DOI] [PubMed] [Google Scholar]
- 11.McKinstry B, Watson P, Pinnock H, Heaney D, Sheikh A. Telephone consulting in primary care: a triangulated qualitative study of patients and providers. Br J Gen Pract 2009;59:e209–18 10.3399/bjgp09X420941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wasson J, Gaudette C, Whaley F, et al. Telephone care as a substitute for routine clinic follow-up. JAMA 1992;267:1788–93 10.1001/jama.1992.03480130104033 [DOI] [PubMed] [Google Scholar]
- 13. www.renalpatientview.org.
- 14.Katz SE, Kaltsounis D, Halloran L, Mondor M. Patient safety and telephone medicine: some lessons from closed claim case review. J Gen Intern Med 2008;23:517–22 10.1007/s11606-007-0491-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bunn F, Byrne G, Kendall S. The effects of telephone consultation and triage on healthcare use and patient satisfaction: a systematic review. Br J Gen Pract 2005;55:956–61 [PMC free article] [PubMed] [Google Scholar]
- 16.Connor A, Lillywhite R, Cooke MW. The carbon footprint of a renal service in the United Kingdom. QJM 2010;103:965–75 10.1093/qjmed/hcq150 [DOI] [PubMed] [Google Scholar]
- 17.DEFRA 2009 guidelines to DEFRA/DECC's GHG conversion factors for company reporting www.defra.gov.uk/environment/business/reporting/conversion-factors.htm.
- 18. www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_125490.pdf.
- 19.The Renal Association, UK Renal Registry Eleventh annual report, Bristol, UK, UK Renal Registry, December 2008 www.renalreg.com/Reports/2008.html.
- 20.Stevens PE, O'Donoghue DJ, de Lusignan S, et al. Chronic kidney disease management in the United Kingdom: NEOERICA project results. Kidney Int 2007;72:92–9 10.1038/sj.ki.5002273 [DOI] [PubMed] [Google Scholar]
- 21.National Collaborating Centre for Chronic Conditions Chronic kidney disease: national clinical guideline for early identification and management in adults in primary and secondary care. London: Royal College of Physicians, 2008. [PubMed] [Google Scholar]
- 22.Department of Health High quality care for all: NHS Next Stage Review final report. London: DH, 2008. [Google Scholar]
- 23.NHS Sustainable Development Unit Saving carbon, improving health. London: NHS Sustainable Development Unit, 2009. [Google Scholar]


