Introduction
Acute liver failure (ALF) is an unpredictable and rapidly progressive life threatening multisystem condition that ensues when an insult causes diffuse necrosis of liver parenchyma disrupting hepatocyte function in patients who have no pre-existing liver injury. The subsequent development of encephalopathy and coagulopathy within days or weeks represents the key features of ALF, but critically often culminates with multi-organ failure (MOF), which impacts significantly on mortality. Timely referral to specialist centres with specialist expertise in the management of ALF and liver transplantation is crucial.
The availability of donor organs is under continued pressure in the UK and worldwide. Patients with ALF must fulfil a strict set of selection criteria based on published risk factors for prioritisation before being established on the national super-urgent transplantation waiting list.
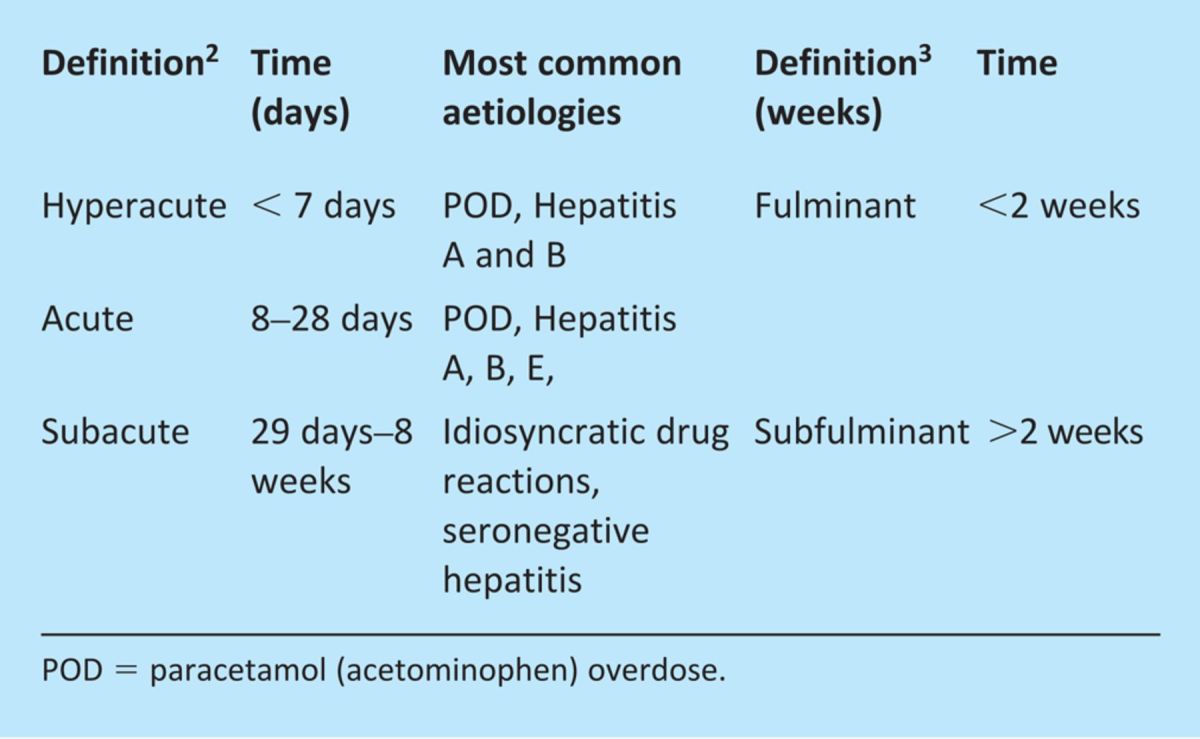
Classification and incidence of ALF
The two most common definitions for ALF concentrate on the time period from jaundice to the onset of encephalopathy (Table 1).1 ALF is rare with around 400 and 2,800 cases of ALF per year in the UK and USA, respectively.1 In the developing world the leading cause of ALF is predominated by the viral hepatitides, particularly hepatitis B and in the UK, like the USA, paracetamol (acetominophen) overdose (POD) is the leading cause.
Table 1.
Classifications of acute liver failure (ALF) (time from jaundice to onset of encephalopathy).
Aetiologies of ALF
Paracetamol (acetominophen) overdose
In the UK, POD comprises up to 50% of all poisoning admissions and around 10% of admissions in the USA.4 The assessment of the risk of developing ALF from POD, whether accidental or deliberate, is intimately related to the total dose ingested and the time from ingestion to presentation. The pathophysiological reasons behind this relate to the length of time exposed to the active unstable N-acetyl p-benzoquinone imine (NAPQI) metabolite that depletes hepatic glutathione levels. Once NAPQI is unopposed by hepatic glutathione hepatocellular damage ensues unless the antidote, a glutathione precursor, N-acetylcysteine (NAC) or methionine, is given in a timely fashion.
Viral hepatitides
All the hepatitides except for possibly hepatitis C have been implicated in cases of ALF.1 Viral hepatitis A and B are the most common causes of ALF worldwide including France and Japan with hepatitis E predominant in India. Hepatitis E is common in Asia and Africa with the risk of ALF greatest in pregnancy at more than 20%, particularly during the third trimester.
Idiosyncratic drug reactions
The administration of medicines directly affects the liver because it is the primary site of drug metabolism and elimination. Drug-induced liver injury (DILI), including cases of acetominophen toxicity, is the leading cause of ALF and indication for liver transplantation. The remainder of DILI cases comprise idiosyncratic reaction, which occurs in around 1 in 10,000 exposed patients. However, more than 1,000 drugs and herbal remedies have been implicated in DILI and altogether comprise 10% of ALF cases.5
Other
Malignancy has featured in a number of case reports in the literature that have documented a wide range of solid and haematological tumours as rare causes of ALF. Vascular insults as a cause of ALF are uncommon; however, these include ischaemic hepatitis associated with low cardiac output states and variable degrees of left and right ventricular cardiac dysfunction. Both inherited and acquired procoagulant disorders can cause veno-occlusive disorders, such as Budd-Chiari (BC) and portal vein thrombosis. Metabolic disorders are also uncommon but can be due to both inherited and acquired disorders, which include acute fatty liver of pregnancy, fructose intolerance, galactosemia, lecithin-cholesterol acyltransferase deficiency, Reye's syndrome, tyrosinemia and Wilson's disease (WD). Other rare but important causes of ALF include HELLP (haemolysis, elevated liver enzymes and low platelets) syndrome of pregnancy.
Clinical features and management
General
The management of ALF should follow some general principles implemented on initial presentation. Establishing a diagnosis of the underlying insult is crucial in determining potential therapies that could halt the injurious process and reverse liver failure. Prompt testing of hepatitis and atypical viral serology, autoantibodies, along with an illicit drugs screen, paracetamol levels, urine and serum copper where appropriate are frequently indicated. Additionally, ultrasonography of the liver and its vasculature is important. Where possible, if the history and investigations do not suggest a viral or drug-induced insult then axial imaging with contrast enhanced triple-phase computer tomography is advisable. Early recognition and the treatment of sepsis along with the support and prevention of organ dysfunction are vital in order to increase the potential for hepatic regeneration. Finally, a timely decision regarding listing for super-urgent liver transplantation is needed when it becomes clear sufficient hepatic regeneration is not going to occur. The huge potential for clinical deterioration and the limited availability of organs accounts for the narrow window of opportunity to undertake this procedure.
Cardiovascular
The circulatory hallmarks of established ALF mirror the haemodynamic changes of sepsis with an elevated cardiac output and vasoplegia. The management goals for the circulation in established ALF intuitively, in view of the similarities and despite formal validation, should follow the initial resuscitation recommendations outlined in the Surviving Sepsis Campaign (SSC). The early use of haemodynamic monitoring is recommended as it often forms a vital aspect of management providing important additional clinical indices about central circulating volumes and cardiac output. Furthermore, interrogation of myocardial function with echocardiography to evaluate left and right ventricular filling and function is also important.
There are problems associated with some the SSC parameters; central venous oxygen saturation (scvO2) is often significantly elevated reflecting the hyperdynamic circulation and microvascular shunting. The SSC threshold for lactate of 4 mmol/l, is unlikely to reflect sole circulatory disarray in ALF, but it should be assumed to be so until adequate volume resuscitation has been implemented. Relative adrenal insufficiency (RAI), defined as a total cortisol (TC) level less than 248 nmol/l after corticotropin administration, has a reported prevalence of 62% in ALF. Hydrocortisone replacement therapy is therefore, frequently indicated as it is associated with reductions in vasopressor requirements, albeit without any mortality benefit.6
Respiratory
The development of hepatic encephalopathy in ALF is one of the primary indications for intubation and ventilation to establish airway protection. Patients will also develop a spectrum of respiratory complications associated with both mechanical ventilation and critical illness. These include pleural effusions, atelectasis and poor compliance due to raised intra-abdominal pressure (IAP) or reduced thoracic compliance due to chest wall oedema. Acute lung injury (ALI) and adult respiratory distress syndrome (ARDS) complicate up to 30% of paracetamol-induced ALF cases,7 particularly those with significant intracranial hypertension (ICH) and vasopressor requirements. ICH is associated with the use of deep sedation, limited endotrachial suctioning and hypothermia that can lead to secretion retention contributing to the high incidence of gram-negative ventilator-associated pneumonias and ALI.
Conventional protective ventilation manoeuvres employed for ALI/ARDS can impact on cerebral perfusion exacerbating ICH due to elevations in CO2. Consequently, a balanced approach is often required. High positive end expiratory pressures (PEEP) are necessary to optimise recruitment and prevent atelectasis of basal lung segments. The opportunity to wean patients from the ventilator is usually once the acute phase of the liver injury has subsided or in the post-transplant period when ICH has settled. The insertion of a tracheostomy percutaneously to facilitate weaning from the ventilator can be performed safely despite the occurrence of coagulopathy and thrombocytopenia in ALF.8
Nutrition
Numerous metabolic abnormalities and their associated complications are encountered in ALF, however few studies have assessed and identified best practice. Hypoglycaemia is a significant metabolic abnormality encountered in ALF, due to the loss of hepatic glycogen stores, impaired gluconeogenesis and hyperinsulinaemia. It is important to establish early and maintain normoglycaemia with infusions of 20–50% dextrose that will continue until enteral nutrition is commenced usually within 24 hours of admission aiming to achieve 25–30 kcal/kg/day. If gut failure and poor absorption become a problem, it is safe to use total parenteral nutrition (TPN) in patients with ALF.9 The use of continuous renal replacement therapy (CRRT) necessitates supplementation with vitamins, trace elements and phosphate.10
Immunity and bacteraemia
The innate immunity undergoes significant changes in response to acute liver injury and many of these resemble the clinical features of systemic sepsis with a systemic inflammatory response syndrome. These complex immune responses include complement deficiency, neutrophil dysfunction and macrophage-mediated release of cytokines, which are all responsible for the increased incidence of bacteraemia and can affect the degree of encephalopathy. The use of empirical broad-spectrum antibiotics, the attention to appropriate nutrition, gut decontamination, oral hygiene, use of ventilator care bundles, intense daily scrutiny of the indwelling intravenous catheters and vigilant infection control measures are all important in limiting the occurrence of bacteraemia.
Acute kidney injury
The incidence of acute kidney injury (AKI) in ALF is significantly higher than that of the general critically ill population, ranging from 40–85% depending on aetiology, with POD associated with a higher incidence at around 75%.11 The mechanisms involved in the development of AKI in ALF resemble the pathophysiological models of hepatorenal syndrome and septic AKI. Vasoactive mediator-induced changes cause heightened homeostatic sympathetic nervous and renin-angiotensin system (RAS) responses culminating in intrarenal arterial vasoconstriction. Both acute tubular necrosis and septic AKI mechanism with microcirculatory changes that result in renal venous congestion and disturbed cellular energy mechanisms are all likely to play a role.12 Paracetamol nephrotoxicity is responsible for the higher incidence of AKI in POD and is due to increased renal proximal tubules cell death by mechanisms that differ to those causing hepatotoxicity.
The high incidence of AKI leads to an increased requirement for CRRT for both renal- and non-renal-related reasons. The anticoagulation of CRRT circuits is still required, despite the coagulopathy of ALF, which usually relies on the safe use of prostacyclin due to its short half-life, along with other measures such as good vascular access and pre-dilution to achieve extended filter life spans.
Coagulation
The integral relationship between clotting factor production and acute hepatocyte necrosis is key to determining both bleeding risk and prognosis. The prothrombin time (PT) is used for the prognostic assessment of ALF with a PT >36 seconds at 36 hours after ingestion predicting that 50% of patients will go on to develop ALF. Furthermore, a PT increasing on day 4 and peaking at PT >180 seconds is predictive of a 65% mortality.13 However, the role of PT in assessing bleeding risk needs to be cautioned in the context of ALF as both thrombocytopenia and platelet function seem to correlate better with bleeding risk.
Neurology
Intracranial hypertension (ICH) is still frequently responsible for cerebral death in ALF, despite a decline over the past two decades. Adverse outcomes with ICH are more common in the young where brain volumes are higher and intracranial space is at a minimum. The cause of cerebral oedema in ALF is multifactorial, but integrally related to ammoniagenesis and the inflammatory responses of ALF. A blood ammonia >200 umol/l is associated with an increased risk of cerebral herniation.14 Blood ammonia is converted to glutamine in the brain, which accumulates within astrocytes raising osmolality leading to swelling. The standards of care for ICH used in neurosurgical patients are the mainstays of treatment of ICH encountered in ALF. These include maintaining the head elevated at 30 degrees, a mean arterial pressure to achieve a cerebral perfusion pressure >55 mmHg and a partial pressure of carbon dioxide (pCO2) <4.5 KPa when autoregulation is preserved, hypothermia with a core body temperature <36°C, heavy sedation and hypernatraemia, maintained with hypertonic saline to achieve a serum sodium concentration >145 mmol/l. Often, monitoring of intracranial pressure with an intracranial pressure bolt along with additional information regarding cerebral perfusion utilising cerebral dopplers is warranted, particularly when patients are to undergo liver transplantation.
Prognositication of ALF
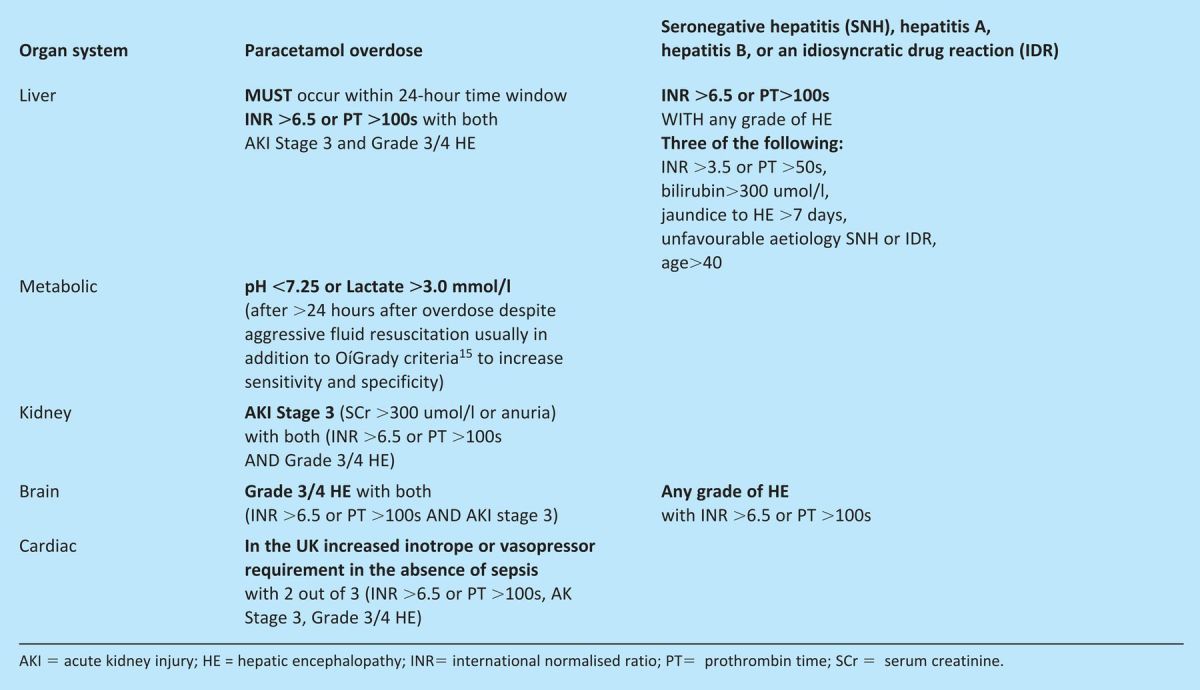
Spontaneous recovery in ALF is largely determined by the underlying pathology, therefore, establishing a diagnosis is important in determining prognosis and can influence management. Clinical criteria predicting prognosis in patients with ALF were first described at King's College Hospital, London. There are other criteria, which have been developed and used, which include Clichy, BiLE score and even the modified end-stage liver disease (MELD) score. The most widely used are the King's College Criteria (KCC), which were developed from a retrospective analysis of patients with acute liver failure medically managed between 1973–85. The identified prognostic variables were then assessed prospectively with the subsequent development of the KCC. They do not perform perfectly with up to 25% of ALF cases that fulfil KCC surviving without transplantation. The KCC were developed for both paracetamol- and non-paracetamol-related ALF and assist decisions regarding when to refer or discuss cases with specialist centres that perform OLT or to decide whom to priority list for transplantation (Table 2 and Table 3).
Table 2.
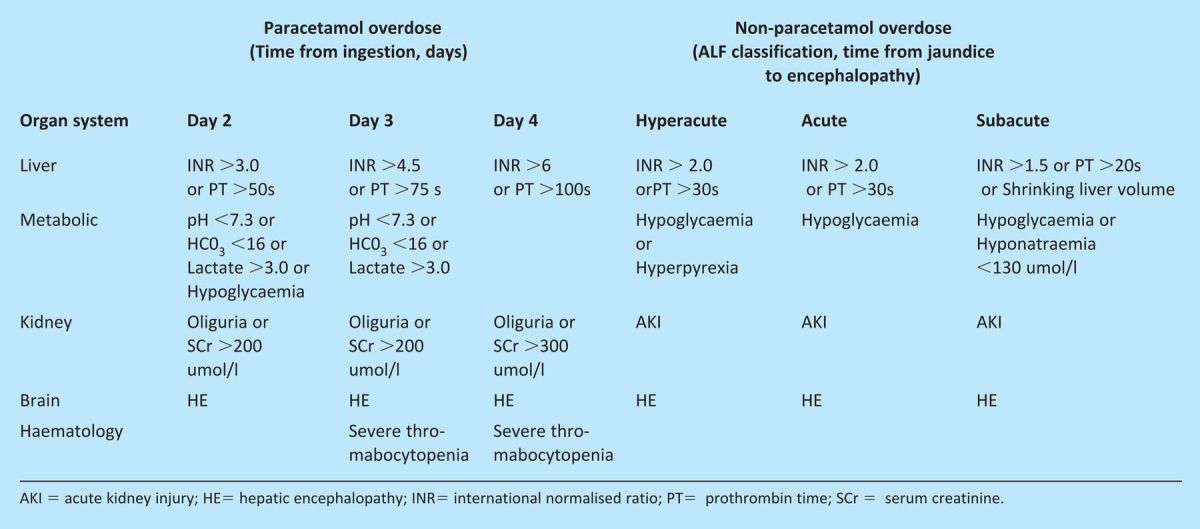
Table 3.
Summary
ALF is a multisystem disorder necessitating both predictive and reactive management strategies to support and protect organs from the initial and subsequent insults encountered. Early referral to a specialist liver centre with the option of liver transplantation is recommended. Furthermore, a good understanding of the poor prognostic variables is necessary to determine those most at risk of developing ALF in order to facilitate timely, safe transfer and listing for liver transplantation.
References
- 1.Khashab M, Tector AJ, Kwo PY. Epidemiology of acute liver failure. Curr Gastroenterol Rep 2007;9:66–73 10.1007/s11894-008-0023-x [DOI] [PubMed] [Google Scholar]
- 2.O'Grady JG, Williams R, Calne R. Transplantation in fulminant hepatic failure. Lancet 1986 10.1016/S0140-6736(86)92247-6;2:1227. [DOI] [PubMed] [Google Scholar]
- 3.Bernuau J, Rueff B, Benhamou JP. Fulminant and subfulminant liver failure: definitions and causes. Semin Liver Dis 1986;6:97–106 10.1055/s-2008-1040593 [DOI] [PubMed] [Google Scholar]
- 4.Dargan PI, Jones AL. Acetaminophen poisoning: an update for the intensivist. C. rit Care 2002;6:108–10 10.1186/cc1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russmann S, Kullak-Ublick GA, Grattagliano I. Current concepts of mechanisms in drug-induced hepatotoxicity. Curr Med Chem 2009;16:3041–53 10.2174/092986709788803097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harry R, Auzinger G, Wendon J. The clinical importance of adrenal insufficiency in acute hepatic dysfunction. Hepatology 2002;36:395–402 10.1053/jhep.2002.34514 [DOI] [PubMed] [Google Scholar]
- 7.Baudouin SV, Howdie P, O'Grady JG, Webster NR. Acute lung injury in fulminant hepatic failure following paracetamol poisoning. Thorax 1995;50:399–402 10.1136/thx.50.4.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Auzinger G, O'Callaghan GP, Bernal W, Sizer E, Wendon JA. Percutaneous tracheostomy in patients with severe liver disease and a high. Crit Care 2007 10.1186/cc6143;11:R110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salvino R, Ghanta R, Seidner DL, et al. Liver failure is uncommon in adults receiving long-term parenteral nutrition. JPEN J Parenter Enteral Nutr 2006;30:202–8 10.1177/0148607106030003202 [DOI] [PubMed] [Google Scholar]
- 10.Schmidt LE, Dalhoff K. Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology 2002;36:659–65 10.1053/jhep.2002.35069 [DOI] [PubMed] [Google Scholar]
- 11.Betrosian AP, Agarwal B, Douzinas EE. Acute renal dysfunction in liver diseases. World J Gastroenterol 2007;13:5552–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Langenberg C, Wan L, Egi M, May CN, Bellomo R. Renal blood flow in experimental septic acute renal failure. Kidney Int 2006;69:1996–2002 10.1038/sj.ki.5000440 [DOI] [PubMed] [Google Scholar]
- 13.Harrison PM, O'Grady JG, Keays RT, Alexander GJ, Williams R. Serial prothrombin time as prognostic indicator in paracetamol induced fulminant hepatic failure. BMJ 1990;301:964–6 10.1136/bmj.301.6758.964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clemmesen JO, Larsen FS, Kondrup J, Hansen BA, Ott P. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 1999;29:648–53 10.1002/hep.510290309 [DOI] [PubMed] [Google Scholar]
- 15.O'Grady JG. Acute liver failure. Postgrad Med J 2005;81:148–54 10.1136/pgmj.2004.026005. [DOI] [PMC free article] [PubMed] [Google Scholar]


