Sleep has been described as being of the brain, by the brain and for the brain.1 Sleep and wakefulness are now understood as transitions between brain states precisely defined by electrophysiological criteria. A superimposed 24-hour (circadian) rhythm is regulated from within the suprachiasmatic nucleus deep within the hypothalamus. This tiny population of cells acts as the central body clock and regulates our day–night patterns.
Sleep disturbance on a busy medical ward may be overlooked, but disorders of sleep and wakefulness, as well as circadian rhythm problems, are seen in a wide range of medical and neurological disorders. This review summarises what is currently known about the sleep disturbance seen in a number of neurological diseases and when a general physician may need to refer to the local sleep clinic.
Parkinson's disease
In 1817, James Parkinson gave his name to a progressive neurological disease characterised by stiffness, slowness and tremor. In the last 10 years, the non-motor symptoms within the disease have been recognised. Sleep disturbance, depression and cognitive impairment are all seen frequently in Parkinson's disease (PD) and are often considered to be more disabling than the abnormal movements.2 Sleep disturbance is near universal in advanced disease and some sleep symptoms can predate all other motor phenomena.
Carlos Schenck first described a group of patients with apparently idiopathic rapid eye movement (REM) sleep behaviour disorder (REMBD) (Fig 1) who went on to develop parkinsonian syndromes including dementia with Lewy bodies, PD and multiple system atrophy (MSA).3 REMBD affects approximately 0.5% of elderly males, with patients acting out increasingly violent and vivid dreams often with injury to themselves or their bed partners. It is frequently well treated with long-acting hypnotics such as clonazepam. It is now known that a patient presenting to the sleep clinic with typical REMBD will have a 50% chance of developing a parkinsonian syndrome within five years. Conversely, 40% of patients with PD have REMBD and 95% of those with MSA.
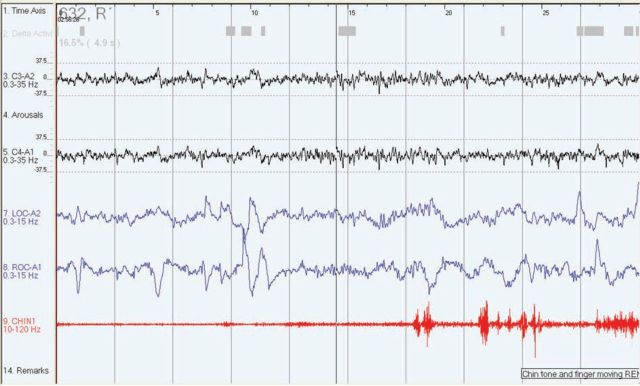
Fig 1.
A 30-second epoch from a polysomnograph demonstrating the changes in rapid eye movement (REM) behaviour disorder. The electro-oculogram channels (LOC and ROC) (blue) show the characteristic eye flicks of REM sleep. The submental electromyogram (CHIN 1) (red) should be flat but shows phasic activity as the patient is moving.
Daytime sleepiness was also highlighted with PD patients, particularly with the advent of newer dopamine agonists and the report of ‘sleep attacks’ in association with this group of drugs.4 Patients with PD need to be cautioned about possible daytime sleepiness when they start dopamine agonists. The daytime sleepiness may be accompanied by severe REMBD, nocturia, night-time pain caused by immobility, bradykinesia, sleep apnoea or restless legs – all these are reported in association with PD (Fig 2).
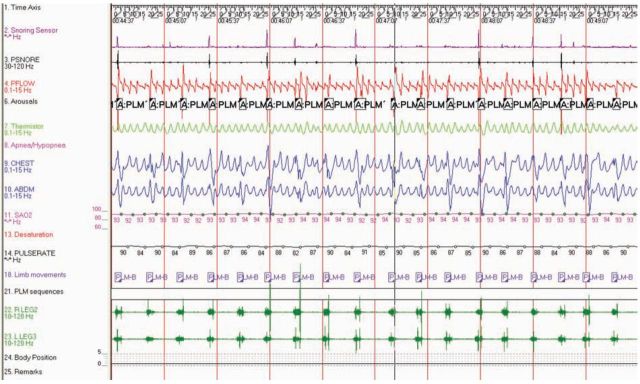
Fig 2.
Five minutes from a polysomnograph demonstrating periodic limb movements in sleep. The electromyogram signals from the anterior tibialis muscles (RLEG and LLEG) (green) show repetitive movements, in this case of both legs, which produce repetitive arousals from sleep.
Early and prominent sleep disturbance is more likely to be associated with early cognitive impairment. A careful sleep history should be taken in all patients with PD and sleep symptoms monitored throughout the disease. PD is notifiable to the Driver and Vehicle Licensing Authority and clinicians must include an assessment of sleepiness. Recent data show that PD patients themselves are poor judges of their safety behind the wheel.5
Key Points
Many neurological diseases have particular patterns of associated sleep disturbance
Rapid eye movement sleep behaviour disorder can predate Parkinson's disease (PD) – sometimes by years — and virtually all patients with PD have a number of sleep disorders in moderate to advanced disease
Fatigue is a common and significant symptom in patients with non-alcoholic fatty liver disease
Nocturnal seizures can significantly disrupt sleep and lead to daytime sleepiness; sleep apnoea can worsen seizures and is common in those with severe epilepsy
Patients with Alzheimer's disease often have circadian rhythm disorders that lead to sundowning; regular sleep-wake patterns and bright light therapy may help
Progressive neuromuscular disorders can cause nocturnal hypoventilation; early recognition and treatment can substantially improve quality of life
Epilepsy
Many patients with epilepsy have seizures during the night. A percentage of patients, especially with frontal lobe epilepsy, have seizures that are exclusively nocturnal. There is a reciprocal relationship between sleep and seizures. Sleep disturbance can increase the likelihood of a fit, particularly with the idiopathic generalised epilepsies. It has also been shown that a brief complex partial seizure early in the night profoundly affects sleep architecture and decreases sleep efficiency; many patients with nocturnal seizures complain of daytime sleepiness which can improve when fits are controlled with medication.6 Seizures are most likely to occur in the lighter stages of non-REM sleep rather than during REM sleep. Frontal lobe seizures can be brief, violent with some retained recall, and can occur several times throughout the night. They can therefore be confused with REMBD, although there is no dream recall with frontal lobe seizures. When in doubt, overnight video polysomnography is required to clarify the diagnosis.
Many of the anticonvulsants are associated with weight gain and sedation, and there is an association between obstructive sleep apnoea and severe epilepsy. In one series, up to 30% of patients awaiting epilepsy surgery had moderate or severe obstructive sleep apnoea.7 It is important to consider this treatable cause of daytime sleepiness which might be confused with side effects of anticonvulsant medication.
Dementia
Sleep disturbance is one of the most common reasons for institutionalisation of demented elderly patients. From 25–50% of the demented elderly suffer from severe nocturnal restlessness at some stage of disease,8 often called ‘sundowning’. Activity monitoring (actigraphy) in both Alzheimer's disease9 and other dementias in patients at home and in institutions confirms profoundly disrupted circadian rhythms in those with moderate and severe dementia. A recent large trial of bright light therapy and melatonin in institutionalised patients showed benefit in measures of daytime function with light therapy alone and together with melatonin.10
Huntingdon's disease
Huntingdon's disease patients often have particularly fragmented sleep, with an increase in periodic limb movements, sleep apnoea and daytime sleepiness.4
Stroke
Sleep-wake disturbance is often neglected in stroke patients but it occurs in 20–40%. Sleep apnoea, both central and obstructive, is commonly seen in the immediate aftermath of stroke – a number of studies have shown an incidence of 50–70% in the first three months following stroke. The link between stroke, hypertension and sleep apnoea is complex. In the absence of controlled trial data, continuous positive airway pressure should be considered for significant symptomatic sleep apnoea, excessive daytime somnolence or high cardiovascular risk profile.11
Traumatic brain injury
A constellation of symptoms follow traumatic brain injury (TBI), but patients commonly experience significant daytime sleepiness and can have sleep-wake reversal. Interestingly, levels of the neuropeptide hypocretin (undetectable in narcolepsy) have been shown to fall acutely following TBI and then gradually increase to normal levels in most patients studied. This provides a physiological explanation for the significant daytime sleepiness seen in many in the immediate weeks after TBI.12 For those with persistent daytime sleepiness, agents such as modafinil have been used with varying degrees of success.
Neuromuscular disease
A wide range of progressive neuromuscular disorders can cause progressive weakness of respiratory muscles. This can lead in turn to nocturnal hypoventilation and gradual progression to respiratory failure. Many patients with such diseases complain of fatigue and reduced exercise tolerance because of skeletal muscle weakness, so symptoms of nocturnal ventilation can be missed unless careful screening is carried out early in the illness. Early morning arterial blood gases and overnight oximetry are recommended in all patients with progressive weakness that affects facial, bulbar and proximal muscles. Examples of diseases that commonly cause significant respiratory failure include motor neuron disease (MND), Duchenne muscular dystrophy and myasthenia gravis.
In patients with MND, nocturnal choking and nocturnal hypoventilation are particularly common in those with moderately advanced disease. There is good evidence for symptom relief with nocturnal invasive ventilation (NIV) and increasing evidence for improved daytime function.13 Long-term effects on survival are less clear but small trials have suggested benefit.14
Myotonic dystrophy
A special note should be made of myotonic dystrophy in which there is central hypersomnolence and abnormal REM sleep as well as significant sleep disordered breathing.15 Management of this group of patients is complex and requires multidisciplinary input from therapists familiar with the condition. Modafinil helps a small percentage of patients. In the author's experience, NIV is not always tolerated even in the presence of significant respiratory failure.
Restless legs syndrome
Restless legs syndrome (RLS) is common, affecting 5–10% of the population, with associations with iron deficiency, dialysis and pregnancy. There is a family history in 50% of affected patients. It is characterised by unpleasant sensations deep within calves and thighs that cause the patient to move, and has a clear circadian pattern being worse in the evening and first half of the night. These symptoms contrast with peripheral neuropathy where dysaesthesia is usually maximal within the feet and there is no circadian pattern to symptoms or relief with movement. The associated periodic limb movements of sleep can fragment sleep enough to cause daytime sleepiness. Tricyclic antidepressants, such as amitriptyline, can make RLS worse so should be avoided, but gabapentin, dopamine agonists, such as ropinirole and pramipexole, clonazepam and opiates all help symptoms. Iron replacement should be used for ferritin levels below 45 mg/dl.16
References
- 1.Hobson JA. Sleep is of the brain, by the brain and for the brain. Nature 2005;437:1254–6 10.1038/nature04283 [DOI] [PubMed] [Google Scholar]
- 2.Aarsland D, Larsen JP, Tandberg E, Laake K. Predictors of nursing home placement in Parkinson's disease: a population-based, prospective study. J Am Geriatr Soc 2000;48:938–42 [DOI] [PubMed] [Google Scholar]
- 3.Boeve BF. REM sleep behaviour disorder: Updated review of the core features, the REM sleep behaviour disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann N Y Acad Sci 2010;1184:15–54 10.1111/j.1749-6632.2009.05115.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnulf I, Leu S, Oudiette D. Abnormal sleep and sleepiness in Parkinson's disease. Curr Opin Neurol 2008;21:472–7 10.1097/WCO.0b013e328305044d [DOI] [PubMed] [Google Scholar]
- 5.Uc EY, Rizzo M, Johnson AM, et al. Road safety in drivers with Parkinson disease. Neurology 2009;73:2112–9 10.1212/WNL.0b013e3181c67b77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manni R, Galimberti CA, Sartori I, et al. Nocturnal partial seizures and arousals/awakenings from sleep: an ambulatory EEG study. Funct Neurol 1997;12:107–11 [PubMed] [Google Scholar]
- 7.Manni R, Terzaghi M, Arbasino C, et al. Obstructive sleep apnea in a clinical series of adult epilepsy patients: frequency and features of the comorbidity. Epilepsia 2003;44:836–40 10.1046/j.1528-1157.2003.55702.x [DOI] [PubMed] [Google Scholar]
- 8.Van Someren EJ. Circadian and sleep disturbances in the elderly. Exp Gerontol 2000;35:1229–37 10.1016/S0531-5565(00)00191-1 [DOI] [PubMed] [Google Scholar]
- 9.Hatfield CF, Herbert J, van Someren EJ, Hodges JR, Hastings MH. Disrupted daily activity/rest cycles in relation to daily cortisol rhythms of home-dwelling patients with early Alzheimer's dementia. Brain 2004;127:1061–74 10.1093/brain/awh129 [DOI] [PubMed] [Google Scholar]
- 10.Dowling GA, Burr RL, Van Someren EJ, et al. Melatonin and bright-light treatment for rest-activity disruption in institutionalized patients with Alzheimer's disease. J Am Geriatr Soc 2008;56:239–46 10.1111/j.1532-5415.2007.01543.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbance in ischaemic stroke. Neurology 2009;73:1313–22 10.1212/WNL.0b013e3181bd137c [DOI] [PubMed] [Google Scholar]
- 12.Baumann CR, Werth E, Stocker R, Ludwig S, Bassetti CL. Sleep-wake disturbances 6 months after traumatic brain injury: a prospective study. Brain 2007;130 (Pt 7):1873–83 10.1093/brain/awm109 [DOI] [PubMed] [Google Scholar]
- 13.Annane D, Orlikowski D, Chevret S, Chevrolet JC, Raphaíl JC. Nocturnal mechanical ventilation for chronic hypoventilation in patients with neuromuscular and chest wall disorders. Cochrane Database Syst Rev 2007;4:CD001941. [DOI] [PubMed] [Google Scholar]
- 14.Bourke SC, Tomlinson M, Williams TL, et al. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 2006;5:140–7 10.1016/S1474-4422(05)70326-4 [DOI] [PubMed] [Google Scholar]
- 15.Laberge L, Bégin P, Dauvilliers Y, et al. A polysomnographic study of daytime sleepiness in myotonic dystrophy type 1. J Neurol Neurosurg Psychiatry 2009;80:642–6 10.1136/jnnp.2008.165035 [DOI] [PubMed] [Google Scholar]
- 16.Salas RE, Gamaldo CE, Allen RP. Update in restless legs syndrome. Curr Opin Neurol 2010;23:401–6 [DOI] [PMC free article] [PubMed] [Google Scholar]