Key points
Insomnia symptoms are the most frequently reported psychological complaints in Britain
Chronic insomnia degrades social and occupational performance, impairs personal safety, can delay recovery from acute illness episodes and is an independent risk factor for major depression
Hypnotic drugs are effective only for short-term treatment (usually up to four weeks)
Cognitive behavioural therapy for insomnia produces lasting benefits in up to 80% of treated patients
Attention to sleep hygiene should accompany all insomnia treatments
Sleep disturbances are the most commonly reported psychological symptoms in Britain.1 Prevalence estimates of chronic symptoms accompanied by daytime consequences range from 8–12% of the adult population.2 Age-specific rates, however, show a steady rise in prevalence across the lifespan, from 3–5% at age 18–25 to 25–30% age 65 and over.2 At all ages, women generally report higher (though sometimes only marginally) rates of insomnia than men. Insomnia risk is also greatly elevated among those with long-term health conditions. Analyses controlling for age and gender, for example, indicate that heart disease, memory problems, depression and pain are all independently associated with an 80–150% increased odds of insomnia symptoms.3 Caring environments also jeopardise sleep quality. Insomnia risk is significantly increased among those providing care at home for a dependent relative or spouse.4 Hospitals (through, for example, noise, unfamiliarity, patient anxiety, association with acute illness episodes, side effects of treatment regimens) remain a robust and complex cause of inpatient sleep disturbances.5
Incidence data are scarce but the General Practice Research Database suggests an incidence of all sleep disorder diagnoses of 12.5/1,000 patient years.6 Excluding non-insomnia sleep disorders (eg obstructive sleep apnoea, restless legs syndrome, narcolepsy), insomnia diagnoses probably account for at least half of these cases.
Diagnosis
Insomnia is characterised by a complaint of difficulty initiating or maintaining sleep, or of non-restorative sleep despite adequate opportunities to sleep.7,8 For a diagnosis of insomnia these difficulties should occur three or more times a week, persist for at least a month and be associated with impaired social and/or occupational functioning. Most people with insomnia report symptoms of daytime fatigue, but few (about 20–25%) report symptoms of daytime sleepiness (ie increased daytime sleep tendency). Other daytime symptoms can include mood disturbances, impaired concentration and, within the working population, degraded occupational performance.
Given this emphasis on symptom duration (≥4 weeks), most insomnias can be considered chronic. Sleep disturbances arising from episodic homeostatic (as in occupational sleep loss) or circadian (as in jet-lag) challenges should be given time to self-correct before treatments are initiated. However, short-term sleep disturbances which can arise in the context of hospitalisation may, in the patient's interest, be considered for immediate (and short-term) treatment.9
What causes insomnia?
Research evidence supports the view that chronic insomnia results from the interaction of three separate factors:
predisposing: inherent psychological vulnerability characterised by higher levels of trait anxiety, a susceptibility to cognitive intrusions and attentional bias
precipitating: sleep-disturbing physical, psychological or situational events
perpetuating: maladaptive behavioural responses to sleep disturbance which, over time, help to maintain insomnia as a chronic problem.
This interactive model helps to explain why some precipitating events (eg occupational stress, childbirth, bereavement, illness) can disturb sleep in most people but produce chronic insomnia in only a minority (the predisposed). It also recognises that behavioural (perpetuating) factors can maintain insomnia symptoms long after the precipitating factors have been resolved.
Earlier distinctions between primary insomnia (where there is no accompanying physical or psychological disorder) and secondary insomnia (where the sleep disorder is presumed to result directly from physical or psychological disorders) have proved to be of little clinical value. Review evidence indicates that causality in ‘secondary’ insomnias can rarely be established, and that both primary and ‘comorbid’ (the now preferred term) chronic insomnias share common ‘perpetuating’ factors which respond to the same treatment approaches.10 For practical purposes, therefore, insomnia may be regarded as a single clinical entity.
Impact of insomnia
Insomnia is associated with degraded quality of life, impaired social and occupational functioning, delayed recovery from acute illness episodes, increased healthcare utilisation11 and is an independent risk factor for major depression.12 Combining both direct costs (healthcare utilisation and treatments) and indirect costs (absenteeism and productivity losses), recent detailed Canadian estimates suggest that the annual economic burden per person meeting insomnia criteria is 12 times higher than for a good sleeper ($5,010/year versus $421/year). The greater proportion of this burden (76%) was found in degraded work attendance and performance.13 Recent UK data confirm these trends, showing consistent decrements in work performance among people with insomnia.14
Hypnotic drugs, the principal treatment option for insomnia in both primary and acute care, have long been associated with a range of adverse effects (and consequent indirect costs), including residual sedation, cognitive impairment, daytime anxiety, tolerance, dependence, road traffic accidents and, in older users, falls and hip fractures.11
Clinical assessment
Sleep problems can be usefully assessed using a simple ‘daily sleep diary’. Each morning patients record bed times, wake times, hours slept and sleep quality. As in other areas where problem behaviours are self-monitored (eg eating disorders, obsessive compulsive disorder), sleep diaries can be associated with some symptom improvements. The assessment of daytime experience is also important. In combination with sleep diaries, standardised measurements of sleep-related fatigue and occupational performance can provide a useful guide to both treatment and treatment outcomes. In acute care settings, however, nurse observations of patient sleep durations have proved consistently unreliable.15
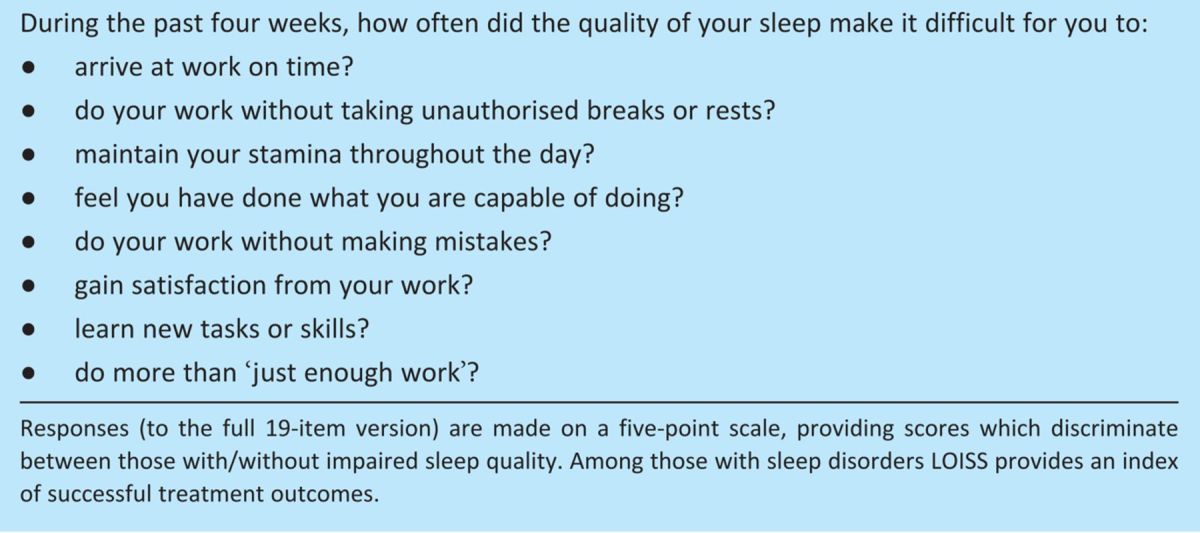
Individual variations in sleep-related occupational impairment have been assessed using the newly developed Loughborough Occupational Impact of Sleep Scale (LOISS). Respondents report how often over the past four weeks the quality of their sleep has affected aspects of occupational performance, including punctuality, absenteeism, efficiency, productivity, job satisfaction, stamina and communication (Table 1). Analyses of global LOISS scores (indicative of sleep-related occupational impairment) have shown effective discrimination between good sleepers and those with clinically disturbed sleep (n=248, mean LOISS 20.84, standard deviation (SD) 17.76 versus 45.30, SD 29.36, p<0.001), demonstrating the utility of LOISS as a screening, assessment and outcome measure.14
Table 1.
Assessing the occupational impact of sleep quality (selected items from the Loughborough Occupational Impact of Sleep Scale (LOISS)).
Treatment of insomnia
Evidence-based insomnia treatments include hypnotic drugs and the non-pharmacological approaches collectively referred to as cognitive behavioural therapy for insomnia (CBT-I). CBT-I comprises five main components:
Sleep hygiene: the ‘dos’ and ‘don'ts' of sleep management.
Sleep restriction: increasing ‘appropriate’ night-time sleepiness by limiting the opportunity to sleep.
Stimulus control: reducing the time spent in bed awake.
Cognitive therapy: controlling pre-sleep thoughts.
Relaxation: physical relaxation strategies.
Experience has shown that treatments can be effectively delivered by a range of non-specialist healthcare professionals (eg counsellors, practice nurses, health visitors, psychologists).16,17
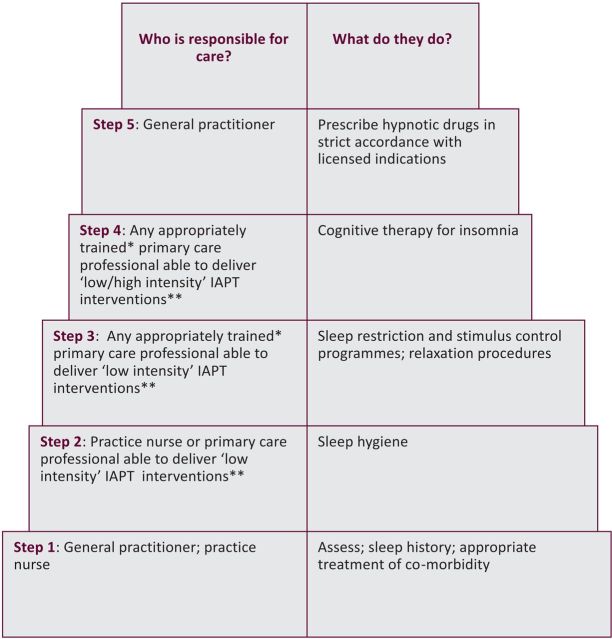
The broader issue of insomnia management has often been eclipsed by (or mistaken for) the important but narrower issue of appropriate hypnotic drug use. The National Institute for Health and Clinical Excellence's (NICE's) 2004 Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia (TA77)18 follows this general trend. Nevertheless, when considered alongside insomnia-relevant contributions from the NICE Clinical Guideline (CG 23)19 on the management of depression, and the National Service Frameworks (NSFs) for Older People20 and Mental Health,21 TA77 supplies the key recommendations for an evidence-based approach to insomnia management. These recommendations are outlined below and summarised in Fig 1 as a ‘stepped-care’ model:
Before commencing treatment, ensure that the sleep problem meets chronicity and severity criteria for insomnia.
The appropriate management of comorbidity is essential but may not resolve the accompanying sleep problem.
The provision of sleep hygiene advice is ‘… fundamental to the overall management strategy’.18 Since the advice targets ‘problem’ behaviours (eg caffeine consumption, irregular sleep habits), some prior assessment of lifestyle is appropriate. In acute care settings, night-time noise reduction and strategies to reduce daytime sleeping should also be considered.
CBT-I for insomnia (including relaxation treatments) has been shown to be effective and should be considered before hypnotic drugs are prescribed.
If patients do not respond to non-pharmacological treatments (or if non-pharmacological treatments are unavailable), hypnotics should be prescribed for short periods of time only, in strict accordance with their licensed indications.
‘Because of the lack of compelling evidence to distinguish between zaleplon, zolpidem, zopiclone or the shorter-acting benzodiazepine hypnotics, the drug with the lowest purchase cost … should be prescribed.’
Use of hypnotic drugs should not be continued beyond four weeks.22
Fig 1.
Stepped care model for insomnia management in primary care. Steps are based on UK National Institute for Health and Clinical Excellence guidance18,19 and UK Department of Health National Service Framework recommendations.20,21 The model is suitable for new cases of primary and comorbid insomnia. With tapered drug withdrawal, long-term hypnotic drug users may be offered steps 1–4. IAPT = improving access to psychological therapies.
∗Appropriately trained in cognitive behavioural therapy for insomnia.
∗∗ As defined in Ref 22.
Self-help
While CBT treatments can offer sustained benefits to the majority of insomnia patients when delivered by trained therapists, the evidence also shows that the principles of behavioural management, delivered in a structured self-help programme, can also improve sleep quality. A recently completed trial of supported self-help (within the UK SomnIA project) proved to be a practical and effective treatment for comorbid insomnia associated with chronic disease.23 The intervention consisted of six booklets addressing key components of CBT-I, plus access to a telephone support line staffed by expert patients. Control participants received standard sleep hygiene advice, in line with UK clinical guidelines. Assessments were conducted at baseline, post-treatment and at three- and six-month follow-ups. Analyses, conducted on an intention-to-treat basis, and after adjusting for age, revealed significantly improved sleep quality post-treatment for treated patients relative to controls.23
Aims of treatment
While the NICE TA77 guideline does not explicitly identify key treatment outcomes, clinical trials suggest four treatment aims valued by patients:
improved subjective sleep quality
reduced sleep latencies
reduced sleep fragmentation
improved daytime (occupational and social) functioning.
Comments
In both acute and primary care, personal and environmental factors which impact directly on sleep onset and continuity should be addressed before formal treatment is initiated. In acute settings, where sleep difficulties can reasonably be assumed to be shorter term, the use of hypnotics (in line with NICE guidelines) is appropriate. Such prescribing should be discussed with the patient with a view to discontinuing hypnotics at discharge. For longer-term insomnia-type sleep problems, psychological approaches are both effective and preferred.
Acknowledgements
The SomnIA (Sleep In Ageing) research was funded by the New Dynamics of Ageing initiative, a multidisciplinary research programme supported by the Arts and Humanities Research Council (AHRC), Biotechnology and Biological Sciences Research Council (BBSRC), Engineering and Physical Sciences Research Council (EPSRC), Economic and Social Research Council (ESRC) and Medical Research Council (MRC) (RES-339-25-0009).
References
- 1.Singleton N, Bumpstead R, O'Brien M, Lee A, Meltzer H. Office for National Statistics. Psychiatric morbidity among adults living in private households, 2000. Int Rev Psychiatry 2003;15:65–73 10.1080/0954026021000045967 [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002;6:97–111 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 3.Foley D, Ancoli-Israel S, Britz P, Walsh J. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res 2004;56:497–502 10.1016/j.jpsychores.2004.02.010 [DOI] [PubMed] [Google Scholar]
- 4.Maher J, Green H. Carers 2000. London: Stationery Office, 2002. [Google Scholar]
- 5.Young JS, Bourgeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 1: factors affecting sleep. J Hosp Med 2008;3:473–82 10.1002/jhm.372 [DOI] [PubMed] [Google Scholar]
- 6.Wallander MA, Johansson S, Ruig-mez A, Garcia-Rodriguez LA, Jones R. Morbidity associated with sleep disorders in primary care: a longitudinal cohort study. Prim Care Companion J Clin Psychiatry 2007;9:338–45 10.4088/PCC.v09n0502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Psychiatric Association Diagnostic and statistical manual of mental disorders: text revision. Fourth edition. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
- 8.American Academy of Sleep Medicine The international classification of sleep disorders, revised: diagnostic and coding manual (ICSD-R), 2nd edn.. Westchester, Il: AASM, 2005. 177–220 [Google Scholar]
- 9.Young JS, Bourgeois JA, Hilty DM, Hardin KA. Sleep in hospitalized medical patients, part 2: behavioral and pharmacological management of sleep disturbances. J Hosp Med 2009;4:50–9 10.1002/jhm.397 [DOI] [PubMed] [Google Scholar]
- 10.State-of-the-Science Panel National Institutes of Health State of the Science Conference statement on Manifestations and Management of Chronic Insomnia in Adults, June 13–15, 2005. Sleep 2005;28:1049–57 [DOI] [PubMed] [Google Scholar]
- 11.Buscemi N, Vandermeer B, Friesen C, et al. 2005. Manifestations and management of chronic insomnia in adults. Evidence Report/Technology Assessment No. 125. (Prepared by the University of Alberta Evidence-based Practice Centre, under Contract No. C400000021.) Agency for Healthcare Research and Quality Publication No. 05-E021-2. Rockville, MD:AHRQ, June. [DOI] [PMC free article] [PubMed]
- 12.Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression?. J Affect Disord 2003;76:255–9 10.1016/S0165-0327(02)00072-1 [DOI] [PubMed] [Google Scholar]
- 13.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms and good sleepers. Sleep 2009;32:55–64 [PMC free article] [PubMed] [Google Scholar]
- 14.Kucharczyk E, Morgan K, Hall A, David B. The Loughborough Occupational Impact of Sleep Scale (LOISS): a new instrument for research and clinical practice. Behav Sleep Med (in press) [DOI] [PubMed] [Google Scholar]
- 15.Aurell J, Elmqvist D. Sleep in the surgical intensive-care unit – continuous polygraphic recording of sleep in nine patients receiving postoperative care. BMJ (Clin Res Ed) 1985;290:1029–32 10.1136/bmj.290.6474.1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Espie CA, Inglis SJ, Tessier S, Harvey L. The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: implementation and evaluation of a sleep clinic in general medical practice. Behav Res Ther 2001;39:45–60 10.1016/S0005-7967(99)00157-6 [DOI] [PubMed] [Google Scholar]
- 17.Morgan K, Dixon S, Mathers N, Thompson J, Tomeny M. Psychological treatment for insomnia in the regulation of long-term hypnotic drug use. Health Technol Assess 2004;8:iii–iv,1–68 [DOI] [PubMed] [Google Scholar]
- 18.National Institute for Clinical Excellence Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia. London: NICE, 2004. Technology Appraisal Guidance 77. [Google Scholar]
- 19.National Institute for Clinical Excellence Depression: management of depression in primary and secondary care. London: NICE, 2004. Clinical Guideline 23. [Google Scholar]
- 20.Medicines and Older People Implementing medicines-related aspects of the NSF for older people. London: Department of Health, 2001. [Google Scholar]
- 21.National Service Framework for Mental Health Modern standards and service models. London: Department of Health, 2001. [Google Scholar]
- 22.Improving access to psychological therapies implementation plan: national guidelines for regional delivery. London: Department of Health, 2008. www.iapt.nhs.uk/silo/files/implementation-plan-national-guidelines-for-regional-delivery.pdf [Google Scholar]
- 23.Morgan K, Gregory P, Tomeny M, David B. Self-help CBT-I in the management of insomnia symptoms associated with chronic disease in older adults: a randomised controlled trial. Abstracts of the 20th Congress of the European Sleep Research Society, Lisbon, Portugal 14–18 September 2010. J Sleep Res 2010;9(Suppl 1):80. [Google Scholar]