Abstract
The depolarising neuromuscular blocking agent suxamethonium chloride, frequently used during endotracheal intubation, is contraindicated in patients with chronic denervation in whom it can cause a life-threatening hyperkalaemic reaction, thought to be mediated through upregulation of nicotinic α7 acetylcholine receptors. An underlying neuromuscular disorder should be considered in all patients with acute respiratory insufficiency, and an alternative neuromuscular blocking drug must be used if there is any possibility of widespread denervation.
Introduction
The diagnosis of the rapidly progressive neurodegenerative disorder amyotrophic lateral sclerosis (ALS, the most common phenotype of motor neuron disease) is frequently delayed by a year or more,1 likely due in part to the insidious and non-specific nature of the early symptoms. Where there is significant and early respiratory compromise, an underlying neuromuscular cause may not be immediately confirmed (or considered), particularly in the acute care setting. The depolarising neuromuscular blocking agent suxamethonium chloride is contraindicated in patients with chronic denervation, in whom it can cause acute hyperkalaemia.
Lesson
A 62-year-old female was admitted to the emergency department of a district general hospital with a three-day history of progressive dyspnoea, and a cough productive of green sputum over the preceding two weeks. There was no significant past medical history but, in retrospect, her relatives reported a generalised deterioration in mobility over the previous year, a weaker voice in the last six months, and progressive hand weakness over three months.
The patient was tachycardic and tachypnoeic on arrival, with reduced air entry to auscultation over the right chest. Oxygen saturation measured with pulse oximetry was 92% on room air. The admitting physician recorded tongue and upper arm fasciculations, bilateral wasting of the thenar eminences and noted generally brisk reflexes in the upper limbs and quadriceps bilaterally. Initial arterial blood gas analysis revealed significant hypoxia and hypercapnoea (pH 7.41, pCO2 6.76 kPa, pO2 7.53 kPa, HCO3 29 mmol/l). Serum potassium was 3.8 mmol/l. A chest radiograph demonstrated evidence of consolidation in the right lower lung field, and intravenous (iv) antibiotics were commenced for presumed bronchopneumonia.
The patient did not tolerate attempts to support her respiratory insufficiency with non-invasive ventilation and deteriorated, with a worsening respiratory acidosis. Initial endotracheal intubation was performed during which 100 mg suxamethonium chloride was administered intravenously without any recorded adverse effects. Two days later after an abrupt episode of oxygen desaturation, a decision was taken to replace the endotracheal tube. Upon iv administration of a further dose of 100 mg suxamethonium chloride marked generalised limb fasciculations were immediately observed, followed by a broad-complex tachycardia (rate 140 beats per minute) accompanied by systolic hypotension. Immediate serum potassium levels were recorded at 8.0 mmol/l. The patient was treated successfully with iv calcium gluconate, nebulised salbultamol, and a combination of iv insulin and dextrose solutions. Serum potassium levels rapidly returned to normal in response. The patient was transferred to a tertiary neurological centre where a clinical diagnosis of ALS was made. Despite iv antibiotics and ventilatory support the patient died one week later from overwhelming sepsis. Classical ALS was later confirmed neuropathologically. There was only mild neuronal loss from anterior horns of the spinal cord. However, diagnostic cytopathology, including Bunina bodies and cytoplasmic TDP-43 aggregates, were present in motor neurons. Skeletal muscle showed neurogenic atrophy but no acute necrosis (Fig 1). Mild frontotemporal TDP-43 pathology was also identified.
Fig 1.
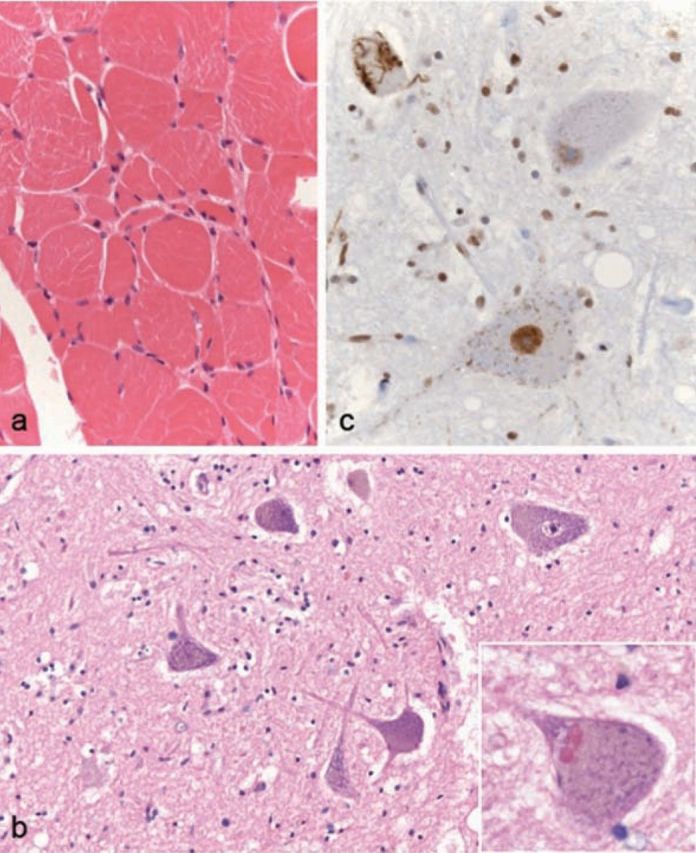
Deltoid muscle biopsy (a) shows neurogenic atrophy with some hypertrophic fibers. No acute muscle necrosis was found anywhere. (b) Anterior horns of the spinal cord showed only mild cell loss. However, cytopathology diagnostic of classical amyotrophic lateral sclerosis was present in surviving neurons, (b inset) including beaded eosinophilic Bunina bodies, and fibrillar as well as granular cytoplasmic TDP-43 pathology, (c) seen as brown reaction product. (a, b inset, c) x400, (b) x200. (c) TDP-43 polyclonal antibody (Proteintech).
Discussion
Suxamethonium chloride (or succinylcholine) is a depolarising neuromuscular blocker acting on nicotinic acetylcholine receptors (AChRs) at the neuromuscular junction (NMJ), and is routinely used as a muscle relaxant during endotracheal intubation.
A rare but life-threatening reaction to suxamethonium chloride is malignant hyperkalemia which has been reported in association with several pathological states, including denervation (eg acute axonal forms of Guillain–Barré syndrome), toxins, immobilisation, infection (including tetanus), muscle trauma or inflammation, and burn injuries. The mechanism is thought to be extracellular potassium influx through AChRs present, not only at the NMJ, but throughout the muscle membrane as a result of up-regulation (in response to denervation in this case). The nicotinic α7 AChR may have a pivotal role in the development of such hyperkalaemic reactions,2 and the reaction to suxamethonium may be dose related.3
This case received an initial dose of suxamethonium without obvious adverse effects, although a serum potassium level was not taken for some hours after this procedure, and it is entirely possible that the levels were transiently raised but without observed fasciculations or cardiac arrhythmia to prompt earlier measurement. The subsequent worsening acidosis, sepsis and immobilisation may have been significant contributors in lowering the threshold for the later catastrophic hyperkalaemic reaction. Interestingly, over-representation of rare missense variants in the genes for nicotinic AChRs have been reported in sporadic ALS patients,4 which it is believed may also be a factor in sensitivity to suxamethonium.
It seems likely that this case developed limb-onset ALS several months prior to this acute admission, and typically respiratory insufficiency is a late feature of the disease. Although the physical signs at presentation prompted suggestion of the diagnosis of ALS there was initially no clear history of chronic deterioration, and a firm diagnosis within a specialist unit was delayed until the patient was already intubated. ALS presenting as respiratory failure may occur in at least 3% of cases from clinic-based series,5 and this group may be at particularly high-risk of hyperkalaemic reactions if this diagnosis is not considered prior to intubation involving administration of suxamethonium. This case highlights the importance of considering an underlying neuromuscular cause in all cases of acute respiratory insufficiency (with or without associated infection), and avoiding the use of suxamethonium if there is any possibility of widespread denervation.
References
- 1.Iwasaki Y, Ikeda K, Kinoshita M. The diagnostic pathway in amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord 2001;2:123–6 10.1080/146608201753275571 [DOI] [PubMed] [Google Scholar]
- 2.Martyn JA, Richtsfeld M. Succinylcholine-induced hyperkalemia in acquired pathologic states: etiologic factors and molecular mechanisms. Anesthesiology 2006;104:158–69 10.1097/00000542-200601000-00022 [DOI] [PubMed] [Google Scholar]
- 3.Brown TC, Bell B. Electromyographic responses to small doses of suxamethonium in children after burns. Br J Anaesth 1987;59:1017–21 10.1093/bja/59.8.1017 [DOI] [PubMed] [Google Scholar]
- 4.Sabatelli M, Eusebi F, Al-Chalabi A, et al. Rare missense variants of neuronal nicotinic acetylcholine receptor altering receptor function are associated with sporadic amyotrophic lateral sclerosis. Hum Mol Genet 2009;18:3997–4006 10.1093/hmg/ddp339 [DOI] [PubMed] [Google Scholar]
- 5.Shoesmith CL, Findlater K, Rowe A, Strong MJ. Prognosis of amyotrophic lateral sclerosis with respiratory onset. J Neurol Neurosurg Psychiatry 2007;78:629–31 10.1136/jnnp.2006.103564 [DOI] [PMC free article] [PubMed] [Google Scholar]


