Abstract
It is a concern that increasing pressure to diagnose, treat and discharge patients rapidly is leading to unacceptably high readmission rates. Readmissions were studied over a two-month period. Patients were identified through the hospital coding system, and electronic discharge summaries provided details of each admission. In total, 69 readmissions were identified, representing 4.34% of medical admissions. Readmitted patients were older than those with single admissions (median age 75 and 71 years, respectively; p<0.05). Initial length of stay was greater in those patients who would go on to be readmitted (median six days; single admission, two days; p<0.0001). Seventy-one per cent of readmissions were deemed avoidable, with discharge before conclusive therapy being the leading factor implicated (56%). Readmission is more likely in older patients with complex care needs. Rapid throughput of patients is not associated with readmission. The majority of readmissions can potentially be avoided with judicious medical care.
Key Words: discharge planning, hospital-acquired infection, length of stay, medical admissions, medical assessment unit, medication error, readmission, rehospitalisation
Introduction
Readmission into hospital is frequently cited as an indicator of the quality of medical care.1 Although widely used, the term ‘readmission’ is poorly defined and confusion persists with regard to its precise interpretation and application.1 The lack of a standardised time frame (varying from 24 hours to one year) makes effective comparison between studies difficult. Furthermore, absence of uniform inclusion criteria makes the definition highly variable and almost indistinguishable from other common terms such as unscheduled admission and rehospitalisation.1–3
Many factors have been highlighted as contributors to patient readmission. Common causes include inappropriate or incomplete treatment, failure of adequate handover from secondary back to primary care, as well as poor social planning, particularly in the elderly.4–6
There is increasing pressure to diagnose, treat and discharge patients in the shortest possible length of time. Average length of stay targets for each medical condition contribute to this pressure, as well as an awareness that prolonged hospital admissions can result in complications such as hospital-acquired infection.
Acute medical assessment units (MAUS) are now well established in the UK. They act to decrease accident and emergency (A&E) waiting times and provide an alternative to standard inpatient hospitalisation in certain conditions that are likely to be acute and short term. This has certainly been evident in retrospective studies in the UK, showing reduced length of stay and A&E waiting times.7–8 Accelerated patient turnover has often been considered to be related to increased rates of readmission and is particularly relevant to acute medical wards, that is, discharges within the first 24 to 48 hours.
One method of reducing length of stay and readmissions is discharge intervention and planning which is a feature of many health institutions worldwide. By coordinating hospital and community services, the inherent trauma associated with transition from hospital to the community is significantly reduced.6
The aim of this retrospective observational study performed at a large London district general hospital was to formulate an appropriate definition of readmission. In doing so, the aim was to investigate the demographics of those who re-presented to hospital, the predominant cause for return, and whether rapid throughput is leading to unacceptably high readmission rates.
The criteria put forth by Landrum and Weinrich were observed throughout the analysis – readmissions studied had to satisfy the following parameters, which included1:
the need to clearly identify all hospital admissions
the establishment of a clinical diagnosis
the purpose of readmission
an agreed discharge to readmission timeframe, and
clear identification of all sources of the information obtained.
Methods
For the purposes of this retrospective, observational study, a readmission was defined as an admission into the MAU within 14 days of discharge from a medical ward within the hospital. Patients initially discharged from A&E, the A&E observation ward or a surgical ward were excluded. Also excluded were patients discharged from other hospitals who subsequently presented to Northwick Park Hospital, as well as those discharged from the hospital who went on to seek medical attention elsewhere.
Readmissions were studied over a two-month period (1 September to 31 October 2007), and all patients meeting the inclusion criteria were identified using the hospital coding system. This provided a database of information including demographic statistics (sex and age) as well as details of initial and subsequent admission (day of discharge, day of readmission, length of stay, medical specialty). The coding system was also used to obtain information about the total number of medical admissions over the same period.
Once study patients were identified, electronic discharge summaries were obtained for their initial and subsequent admissions, and these provided details of the reasons for each admission, history, examination and investigation findings, as well as diagnosis and treatment. Discharge summaries also contained medication information and, in some instances, relevant details of the patient's social circumstances.
Each discharge summary was analysed separately by three clinicians (ZS, SS and HKL) working in the MAU and aware of its practice. For each patient, each clinician gave an opinion as to whether they felt the readmission was in some way related to the index admission, as well as whether it could have been avoided with more judicious care. Where there was disagreement, the majority decision was followed. The statistical package SPSS was used for data analysis.
Results
In the two-month period, there were 1,590 medical admissions in total, of which 1,452 were single admissions, and 69 were readmissions. This gave a readmission rate of 4.34%. Of these, 39 (57%) were male, and 30 (43%) female.
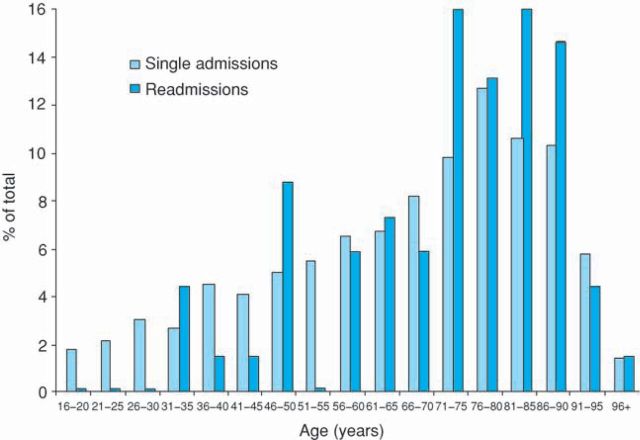
Readmissions were older than single admissions (p<0.05; Fig 1). As expected, the single admission bars reveal that admissions into acute medical care are distributed normally, with significant skew towards older age groups (median 71 years). Readmissions display more significant skew (median 75 years), and this difference is significant (p<0.05; Mann-Whitney U test).
Fig 1.
The distribution of age for single admissions (light bars; n=1,452) and readmissions (dark bars; n = 69) as a proportion of the total in each group.
Length of stay for single admissions ranged from 0 to 142 days, whereas the initial length of stay for readmitted patients was 0 to 40 days. Length of stay for single admissions was found to be shorter (median two days) than the length of initial stay for patients who were readmitted into actual medical care (median six days; p<0.0001; Fig 2). Single admissions were generally discharged more quickly (51% discharged within 48 hours) than patients who went on to be readmitted (only 29% discharged within 48 hours) (p<0.0001; Mann-Whitney U test).
Fig 2.
Length of stay for single admission (light bars; n=1,452) and initial length of stay in readmission cases (dark bars; n= 69).
Of the 69 readmissions, Friday was the most common day of discharge (n=15; 22%), with Tuesday as the most common day of readmission (n = 15; 22%).
Three patients did not have electronic discharge summaries for their index admission, and six had no discharge summary completed for their subsequent readmission, making analysis of their readmission circumstances unfeasible. Discharge summaries for the remaining 63 patients were analysed. Table 1 summarises the causes of readmission.
Table 1.
Causes of readmission.
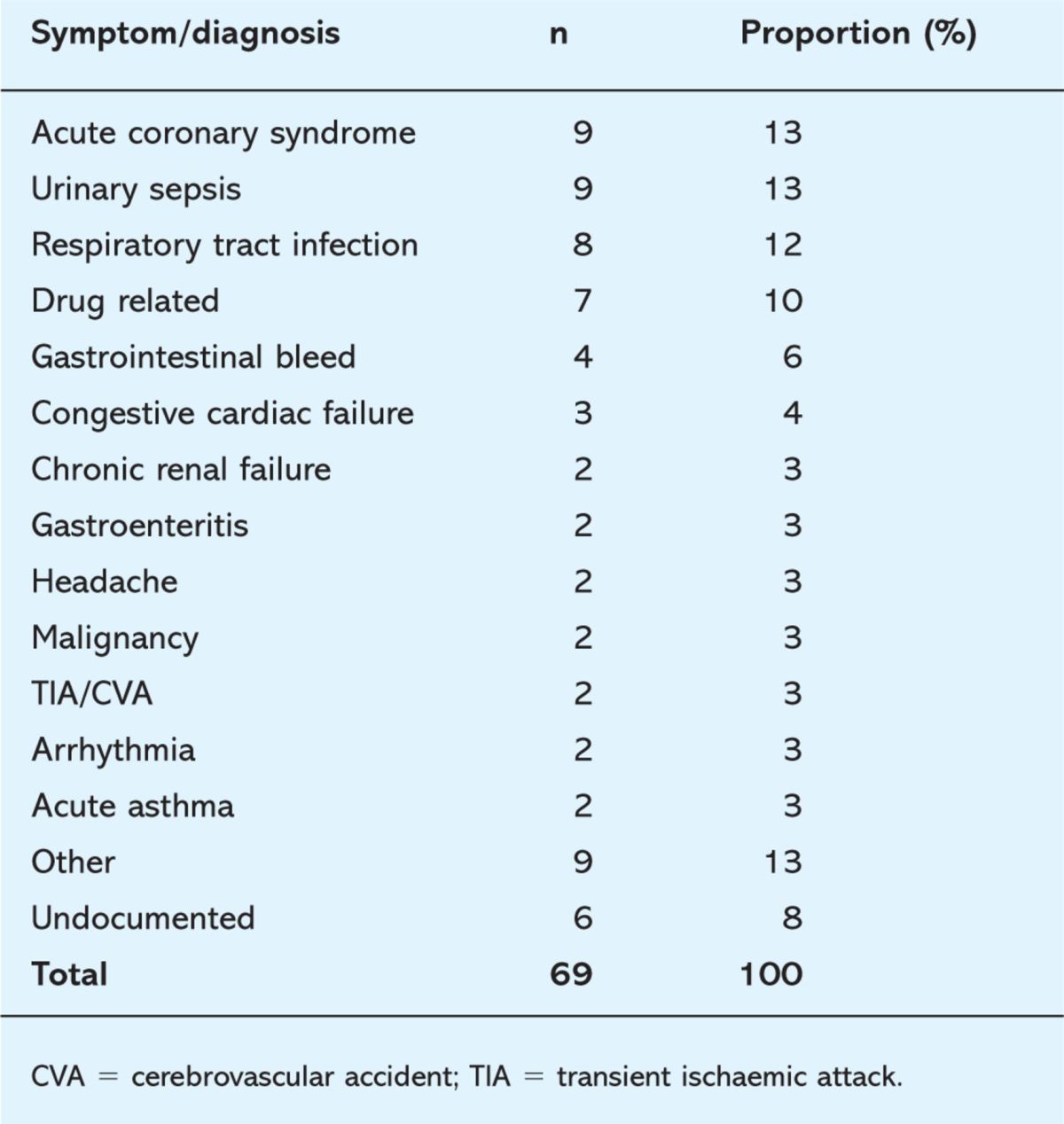
Syndromes of cardiac ischaemia were the joint most common diagnosis, an expected finding given the prevalence of individuals of Indian and Afro-Caribbean origin within the hospital's catchment area in North West London. Urinary sepsis was the other joint most common diagnosis. Respiratory tract infection, especially in the form of an acute exacerbation of chronic obstructive pulmonary disease (COPD), was also common. The term ‘other’ includes diagnoses such as acute severe eczema and deep vein thrombosis. Six patients had no recorded discharge summary.
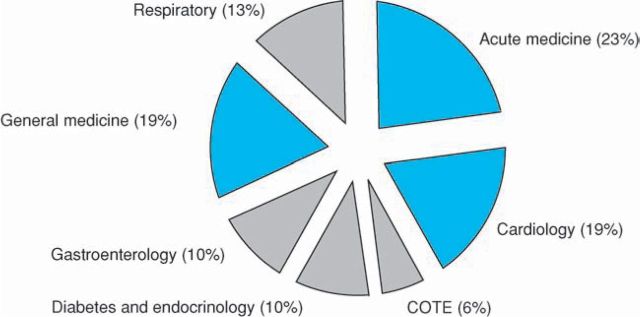
Of the 63 readmissions with electronic discharge summaries for their second admission, 55 (87%) were judged to be related to the index admission. Acute medicine was the discharging specialty with the highest readmission rate (23%), followed by cardiology (19%) and general medicine (19%) (Fig 3). The high-throughput specialties showed a matched high readmission rate. Of particular interest here is the data for acute medicine (from which 55% of patients are discharged), which only account for 23% of readmissions. Care of the elderly (COTE) showed the lowest readmission rate (n = 8; 6%).
Fig 3.
Readmissions by discharging specialty. High-throughput specialties are highlighted in blue.
The term ‘acute medicine’ encompasses patients admitted with general medical complaints who, on admission, are expected to require less than 48 hours of inpatient care. ‘General medicine’ relates to patients of rheumatology, dermatology, neurology and infectious disease specialties who are expected to require at least 48 hours of hospital care.
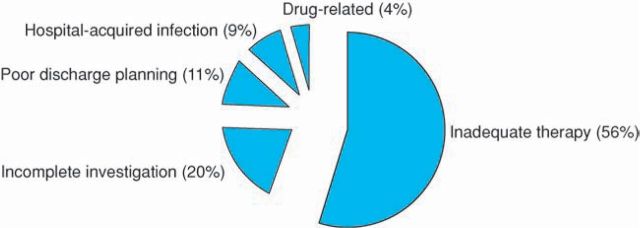
Forty-five cases (71%) of readmission were judged to be avoidable with more judicious care. Factors leading to these are summarised in Fig 4. Inadequate or incomplete treatment of the diagnosed condition was the most common cause leading to readmission (n=25; 56%) followed by insufficient investigations leading to an incorrect or incomplete diagnosis (n=9; 20%), and inadequate discharge planning in terms of suitable handover of care to community services, as well as sufficient patient education (n=5; 11%). Hospital-acquired infection (mostly of the urinary tract but also Clostridium difficile, methicillin-resistant Staphylococcus aureus and pneumonia) as well as adverse drug reactions and prescribing error accounted for a further six readmissions (13%).
Fig 4.
Factors leading to avoidable readmissions.
Discussion
The perception of increasing readmissions into the MAU led to this study. Length of hospital stay has reduced substantially over previous years, in Europe and in the USA.9,10 The concern was that increasing pressure to reduce inpatient length of stay was leading to unacceptably high medical readmissions rates.
An extensive literature search showed a paucity of studies in this field. Furthermore, in the few studies available, there was disagreement as to how to define a readmission, despite an acknowledgement by most authors that readmission rates offer an important insight into the quality of inpatient care.1 One key aspect of defining readmission is the time frame between discharge and subsequent return seeking medical care. This study defined a readmission as an admission into the MAU within 14 days of discharge from a medical ward. This duration was selected on the basis of clinical experience. Empirical research also supports this time frame, with Mistiaen and colleagues observing that post-discharge difficulties experienced by patients are significantly greater at seven days post-discharge than at 30 days.11
The observed readmission rate of 4.34% was lower than the figure predicted based on experience, given that it was precisely the high perceived readmission frequency that had led to the study being undertaken initially. The readmission rate provides some comfort that a high level of successful discharge is being achieved. Nevertheless, the figure needs to be accepted with caution. It would inevitably vary with changes in the inclusion criteria, and rough estimates put the 28-day readmission rate for this hospital at around the 10% mark. Similarly, gross differences in the interpretation of the term mean the figure is not directly comparable to other studies. Finally, as explained earlier, this study did not look at patient re-presentation to other hospitals, nor those presenting to the study hospital after treatment elsewhere. These variables could contribute to a higher readmission figure.
The finding that patients in the readmission group are significantly older than those with single admission is expected and supported in the literature.4 Elderly patients have increased care needs because of co-morbidity, polypharmacy and greater requirement for social care on discharge, which make readmission more likely.
Nevertheless, length of stay data provided unexpected findings. At the outset, it was expected that a rapid throughput of patients placed them at risk of readmission. This study observed that patients readmitted into acute medical care were significantly more likely to have had a longer initial length of inpatient stay. This new finding is likely to represent the complex medical, psychological and social care needs of this high-risk group. Despite significantly greater inpatient time and specialised care, many patients failed to manage in the community.
Interestingly, when contrasting readmissions by discharging specialty in their initial admission, the acute medicine department was responsible for 23% of readmissions, despite it overseeing 55% of medical discharges. It should be noted also that the COTE department had the least proportion of readmissions of all medical subspecialties. This, it is envisaged, is testament to the efforts invested by the multidisciplinary team in arranging adequate discharge plans for this high-risk population.
Readmissions were assessed separately by three clinicians to make a subjective decision as to whether each case could have been avoided. In total 45 cases (71%) were seen as avoidable. Failure to fully treat the diagnosed condition was the most common cause of avoidable readmission, followed by insufficient investigations leading to an incorrect or incomplete diagnosis (see appendix for examples).
Eleven per cent of readmissions were judged to result primarily from incomplete discharge planning. This topic has been investigated thoroughly, and several studies have demonstrated the efficacy of certain discharge planning and aftercare initiatives.6 Parker and colleagues conducted a systematic review looking at the effects of educational interventions on patient functioning after discharge from hospital.12 Three out of four studies looked at the effect of inpatient education on medication compliance after discharge. They showed that compliance improved significantly and patients demonstrated a greater understanding of the drug's purpose.
This study has shown that older patients with more complex care needs are more likely to be readmitted. Surprisingly, a rapid throughput of patients is not associated with readmission but the increased pressure to discharge patients rapidly could be leading to incomplete investigation, with inadequate therapy given to fully treat a diagnosis once made. Importantly, this study has demonstrated that most readmissions can be avoided with more judicious multidisciplinary medical care.
Appendix: case examples
Below are three case studies which highlight what is meant by avoidable readmissions.
Case example 1: inadequate therapy
A 65-year-old gentleman with known COPD managed on combination inhalers presented to A&E with a four-day history of increasing shortness of breath. On examination, he was febrile and hypoxic, with oxygen saturation of 80% on air as measured by pulse oximetry. An electrocardiogram (ECG) showed evidence of right-ventricular hypertrophy, and chest X-ray revealed right-sided lower zone consolidation. A diagnosis of an acute exacerbation of COPD was made, and he was treated with oral co-amoxiclav and clarithromycin, as well as his regular inhalers. He was discharged one day later with a course of oral antibiotics and a reducing course of prednisolone. Arterial blood gas sampling prior to discharge revealed PaO2 of 7.8 kPa. He was readmitted one day after this incident with ongoing shortness of breath, when he was commenced on nebulisers and aminophylline. After an inpatient stay of seven days, he was discharged with an outpatient assessment for long-term oxygen therapy (LTOT). Failure to recognise that the patient required oxygen, which could have been provided at home by the early discharge team, led to the readmission.
Case example 2: incomplete investigation
A 76-year-old female with known rheumatoid arthritis was admitted into acute medical care after presenting with a 10-day history of increasing shortness of breath. On examination, she had a respiratory rate of 28 breaths per minute, and crepitations in both lung bases. A diagnosis of pneumonia was made despite her being afebrile throughout with no evidence of focal consolidation on chest X-ray. She was treated with oral co-amoxiclav, and discharged after two days in hospital. She re-presented to A&E complaining of continuing shortness of breath, when a computed tomography chest scan suggested the presence of a pericardial effusion, which was later confirmed on pericardiocentesis. Examination of the chest X-ray from her first admission showed she indeed had a globular cardiac shadow. She improved with treatment, and was discharged 18 days later. Failure to question the initial incorrect diagnosis, despite considerable clinical reasons to search for an alternative, led to this readmission.
Case example 3: medication error
A 83-year-old female with known heart failure presented to A&E with a two-hour history of central chest pain. ECG revealed a sinus tachycardia and troponin-I was positive at 12 hours (0.08). This presentation was diagnosed as a non-ST elevation myocardial infarction, and she was treated as per hospital acute coronary syndromes protocol, and discharged four days later. Within 24 hours of discharge, she was readmitted with increasing shortness of breath, and examination and chest X-ray confirmed pulmonary oedema. A diligent house officer then noted that her usual frusemide had been omitted from her initial discharge summary, and she had thus gone without the drug for a day. She remained in hospital for a total of five days, and was discharged after treatment with diuretics. In this case, a poorly completed discharge summary contributed to a readmission as a result of medication error.
References
- 1.Landrum L, Weinrich S. Readmission data for outcomes measurement: Identifying and strengthening the empirical base. Qual Manag Health Care 2006;15:83–95. [DOI] [PubMed] [Google Scholar]
- 2.Ashton CM, Wray NO. A conceptual framework for the study of early readmission as an indicator of quality of care. Soc Sci Med 1996;43:1533–41. 10.1016/S0277-9536(96)00049-4 [DOI] [PubMed] [Google Scholar]
- 3.Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care 1997;35:1044–59. [DOI] [PubMed] [Google Scholar]
- 4.Witherington EMA, Pirzada OM, Avery AJ. Communication gaps and readmission to hospital for patients aged 75 years and older: observational study. Qual Saf Health Care 2008;17:71–5. 10.1136/qshc.2006.020842 [DOI] [PubMed] [Google Scholar]
- 5.Van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med 2002;17:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res 2007;7:47. 10.1186/1472-6963-7-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moloney ED, Bennett K, O'Riordan D, Silke B. Emergency department census of patients awaiting admission following reorganisation of an admissions process. Emerg Med J 2006;23:363–7. 10.1136/emj.2005.028944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moloney ED, Bennett K, Silke B. Effect of an acute medical admission unit on key quality indicators assessed by funnel plots. Postgrad Med J 2007;83:659–63. 10.1136/pgmj.2007.058511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, Regional Office for Europe 2008.
- Centers for Disease Control and Prevention, National Centre for Health Statistics 2008.
- 11.Mistiaen P, Duijnhouwer E, Prins-Hoekstra A, Ros W, Blaylock A. Predictive validity of the BRASS index in screening patients with post-discharge problems. Blaylock Risk Assessment Screening Score. J Adv Nurs 1999;30:1050–6. [DOI] [PubMed] [Google Scholar]
- 12.Parker SG, Peet SM, McPherson A. et al A systematic review of discharge arrangements for older people. Health Technol Assess 2002;6:1–183. [DOI] [PubMed] [Google Scholar]