Abstract
John Hughlings Jackson (1835–1911) first clearly described apraxia in 1861, though he did not provide the specific name. Apraxias are subtle motor disorders in which there is an interruption of the organisation of movement mainly located in the left hemisphere. Hugo Karl Liepmann (1863–1925) was responsible for their elucidation, distinguishing ideomotor, limb-kinetic or innervatory, and ideational apraxias that affect distinct central associational areas of the cortex with characteristic clinical results. This notion was later expanded and clarified by Geschwind's ‘disconnection syndromes’. This article summarises the history of this important and common pattern of motor dysfunction.
Key Words: apraxia, disconnection, Hugo Karl Liepmann, syndromes
History
A variety of apraxias commonly complicate strokes and other focal brain lesions. They comprise a variety of high-level motor disorders. In the absence of paralysis, motor or sensory ataxia, a patient exhibits:
failure to produce the correct movement in response to a verbal command
failure to imitate correctly a movement performed by the examiner
failure to perform a movement correctly in response to a seen object
failure to handle an object correctly.1
Apraxia reflects both the nature of the errors made by the patient and the means by which they are elicited.2 Hugo Karl Liepmann (Fig 1) was mainly responsible for their recognition.3–6 Liepmann joined the famous Wernicke's clinic in 1895 and moved to Berlin four years later. Wernicke had correlated discrete cortical lesions with clinical motor signs and proposed that the brain contained ‘fundamental psychic elements’ or ‘memory images’ related to motor acts and sensory experiences. These memory images areas were localised in primary sensory and motor areas with sound images in the cortical terminals of the acoustic nerve, and visual images, in the cortical endings of the visual cortex. He had, however, emphasised that higher functions were not localised in specific regions but were the result of associative connections between motor and sensory memory image areas:
Any higher psychic process, exceeding these mere primary assumptions, could not, I reasoned, be localised, but rested on the mutual interaction of these fundamental psychic elements mediated by means of their manifold connections via the association fibres.7
Fig 1.
Hugo Karl Liepmann.
Earlier physicians must have observed and been puzzled by patients who, while retaining power in their muscles and their coordination were unable to make skilled sequences of movement and could not properly use tools or even copy patterns of movement. Liepmann's studies of the motor system led him to posit a basis for the apraxias, later recognised by Geschwind as a ‘disconnection theory’. Liepmann's conclusions have been amply confirmed.
Evolution of the apraxia
In 1861 John Hughlings Jackson was probably the first to clearly relate the picture of apraxia in the sense described by Liepmann8:
In some cases of defect of speech the patient seems to have lost much of his power to do anything he is told to do, even with those muscles that are not paralysed. Thus, a patient will be unable to put out his tongue when we ask him, although he will use it well in semi-involuntary actions – for example, eating and swallowing. He will not make the particular grimace he is told to do, even when we make one for him to imitate. There is power in his muscles and in the centres for coordination of muscular groups, but he – the whole man, or the ‘will’ – cannot set them agoing…. In a few cases patients do not do things so simple as moving the hand (ie the non-paralysed hand) when they are told…. A speechless patient who cannot put out his tongue when told will sometimes actually put his fingers in his mouth as if to help get it out; and yet, not infrequently, when we are tired of urging him, he will lick his lips with it.9
Since then the concepts and classification of apraxia have continually evolved. The German psychiatrist Carl Maria Finkelnburg observed in 1870 that gestures of communication in aphasiacs were clumsy and incomprehensible. He deduced that they suffer from a general ‘asymbolia’ preventing the use and comprehension of communicative signs.10
In 1871 Heymann Steinthal (1823–99), a German linguist, introduced the word apraxie (from the Greek αηραεια, inaction) to denote the faulty use of everyday objects, such as a fork and knife by patients with aphasia; it was, he thought, owing to a failure to appreciate the desired movement or handling of an object.11 He described ‘the disturbance of relations between movements and the objects with which they are associated’, and considered the errors an ‘augmentation’ of aphasia. In 1899, D De Buck had also described apraxia and used the term parakinesia in a patient who ‘though retaining the concepts for her actions, did not succeed in awakening the corresponding kinetic image’.12 The centre for kinetic images was, he believed, dissociated from ideation, and associated with damage of the occipital and parietal cortex. In 1905 Arnold Pick reported a patient who had lost the ability to use implements, eg he combed his hair with the wrong side of the comb and held a pistol in his mouth.13 Pick viewed this as a motor asymbolia, akin to agnosia (Finkelnburg). Meynert too had described ‘motor asymbolia’, and Nothnagel ‘psychic paralysis’.
Liepmann's studies
Liepmann's first apraxia paper in 1900 was based on a 48-year-imperial councillor (Regierungsrat) who, at first, appeared to be demented but in whom his examination showed several discrete defects of motor function and perception.3 The Regierungsrat, after a stroke was unable to button his shirt, even after the paresis in his right arm had largely resolved. When his hand was placed on the button, his fingers performed the necessary movements, but he was unable to proceed to the next button on his own initiative. Similar disturbances were found when he tried to light a cigar. Although the patient's spontaneous movements were normal (eg using a spoon while eating), when asked to perform or copy gestures with his hand (eg point to your nose) or manipulate imaginary objects (eg show how you use a harmonica), he did so in an odd clumsy fashion. The patient appeared perplexed by the command, but had no visual impairment and no paralysis; Liepmann thought there must be a disconnection of visual, auditory and somatosensory areas from the motor cortex. His patient failed to recognise commonplace objects presented visually, although several tests indicated that his visual perception remained largely intact. Liepmann commented:
Part of what left hand ‘can do’ is not a possession of the right hemisphere which directs its mobility, but a possession which is borrowed from the left hemisphere. The right hand centre … remains during the whole life in a certain dependency on the left hemisphere.3
He predicted cortical lesions underlying the apraxic signs elicited and two years later these lesions were fully confirmed at autopsy.14 Wernicke was delighted with his former pupil's work, which Geschwind described as ‘the most brilliant example of psychological analysis on an anatomical basis, which Wernicke had founded in principle a quarter of a century earlier’.15 In 1907 Liepmann, working with Otto Mass, described the clinical features of ‘dysconnection’ of the hemispheres in a patient with a lesion of the corpus callosum, demonstrated at autopsy.16 Goldstein, another pupil of Wernicke, reported another proven case of disconnection that he called ‘motor apraxia’.17
Liepmann found right-handed patients with left hemisphere lesions – especially of the supramarginal gyrus – were often apraxic in the unparalysed left hand. But those with right hemisphere lesions were not apraxic in their left hand. He concluded that apraxia was a defect dependent on lesions of the dominant left hemisphere, which contained the memory traces for organisation of skilled movements. His later work convinced him that corpus callosum lesions (Fig 2) interrupted the organisation of movement located in the left hemisphere from the motor area in the right, causing ideomotor apraxia in the left arm and hand.6 He distinguished18,19:
ideomotor apraxia in which the difficulty lies in determining what the nature of single movement shall be, so that ideational and kinaesthetic memories are severed
limb-kinetic or innervatory apraxia in which a disturbance of kinaesthetic images of limb movements which caused slow, awkward movements and loss of delicate movements
ideational apraxia, a separate pattern of motor disorganisation in which faulty conception of the movement as a whole and the relationship of its spatial and temporal components to one another disrupted the sequence of movements.
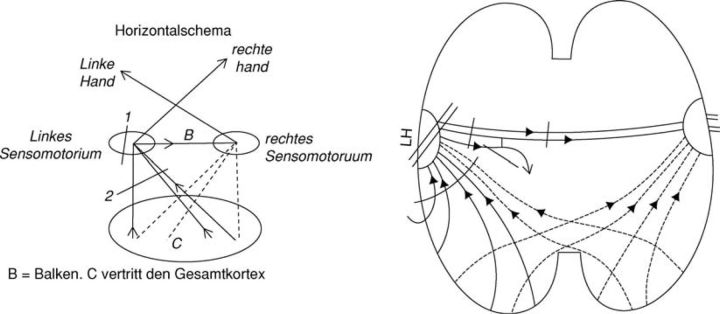
Fig 2.
Liepmann's schema showing callosaL motor signalling. Note the arrows between the two hemispheres, direction from left to right. Reproduced with permission from S. Karger AG, Basel.3,5
Liepmann also described echolalia and wrote other valued neurological papers.
Liepmann's concept
In essence, Liepmann's concept was that the idea or plan of the action, or movement – including its spatial, temporal and form – were located in the left hemisphere. In order to carry out a skilled movement, this plan first had to be retrieved, then associated through left sensorimotor cortical connections, which in turn carried the information to the left primary motor areas. When the left limb performed the movement, the information had to be transmitted from the left to the right via the corpus callosum to activate the right motor cortex. The different apraxias resulted from lesions of the supramarginal gyrus region, and/or the corpus callosum.
Leiguarda and Marsden admirably summarised his conclusions.2 Liepmann thought that the idea or plan of a movement, containing the space–time picture of the movement was stored in the left parietal lobe. To execute a skilled movement, that space–time plan had to be retrieved and associated via cortical connections with the innervatory pattern stored in the left sensorimotorium (the precentral and postcentral gyri and the pes of the superior, middle and inferior frontal convolutions), which conveys the information about the formulae to the left primary motor areas.2 When the left limb performs the movement, the information has to be transmitted from the left to the right sensorimotorium through the corpus callosum to activate the right motor cortex.4–6 Ideational apraxia was considered a disruption of the space–time plan or its activation, so that the creation of the idea of the movement was impossible. In ideomotor apraxia the space–time plans are preserved but unable to guide the innervatory engrams to execute movements because they are disconnected from them. The patient knows what to do but not how to do it. When the disruption of the innervatory engrams interferes with the selection of the required muscle synergies to perform the skilled movements, limb-kinetic apraxia results. Ideomotor and limb-kinetic apraxia were both considered motor apraxia and often coexisted.6
Apraxia, shown by imitation, object use and pantomime, has been found in 50% of patients with left hemisphere damage and in <10% with right hemisphere damage. This suggests that some patients have bilateral representation of praxis.20 Subsequently, the dominance of the left hemisphere in praxis was generally accepted, though Liepmann conceded a possible role for the right hemisphere in left-sided apraxia.14 Von Monakow, who initially criticised Liepmann, actually confirmed his results. Kurt Goldstein in 1908, soon after Liepmann, published a case of callosal disconnexion with motor disturbances.17 Geschwind and Kaplan provided a brilliant analysis of a comparable instance of apraxia caused by callosal infarction. Their case illustrated that the unqualified designation ‘apraxic’ was inadequate:
The left hand in this patient was apraxic to verbal command but not on imitation or object handling; the right hand failed to perform correctly when a response was demanded from this hand to somesthetic stimuli applied to the left hand. Rather than use the term ‘apraxia’ it is therefore preferable to specify the stimulus-response combinations which fail.21
Sperry and colleagues were later to demonstrate that if the two hemispheres of the brain are separated by severing the corpus callosum, the transfer of information between the hemispheres ceases, and the coexistence in the same individual of two ‘functionally different brains’ can be demonstrated with definite behavioural phenomena.22 Geschwind supported Liepmann's ideas and advanced his own neuronal disconnection theory for limb praxis similar to Wernicke's concepts for language.23,24 Geschwind, like Kinnier Wilson, also pointed out the limitations of classification25:
This formal listing of types of apraxia probably had in practice the unfortunate effect of overshadowing Liepmann's much more important detailed analyses of the mechanisms underlying disturbances in motor performances.23
Recent functional imaging studies correlated with neuropsychological deficits have not clarified the fundamental nature of the many different patterns of apraxia in relation to its varied anatomical lesions. Positron emission tomography, single photon emission computed tomography and other studies are of limited value, because most patients examined have deficits additional to apraxia, including dystonia, rigidity and cortical sensory loss; further, many published functional imaging studies have been in the resting state, and not during tests of praxis.26 Thus, the relationship between the metabolic or electrophysiological investigations and the presence of apraxia is not yet defined.
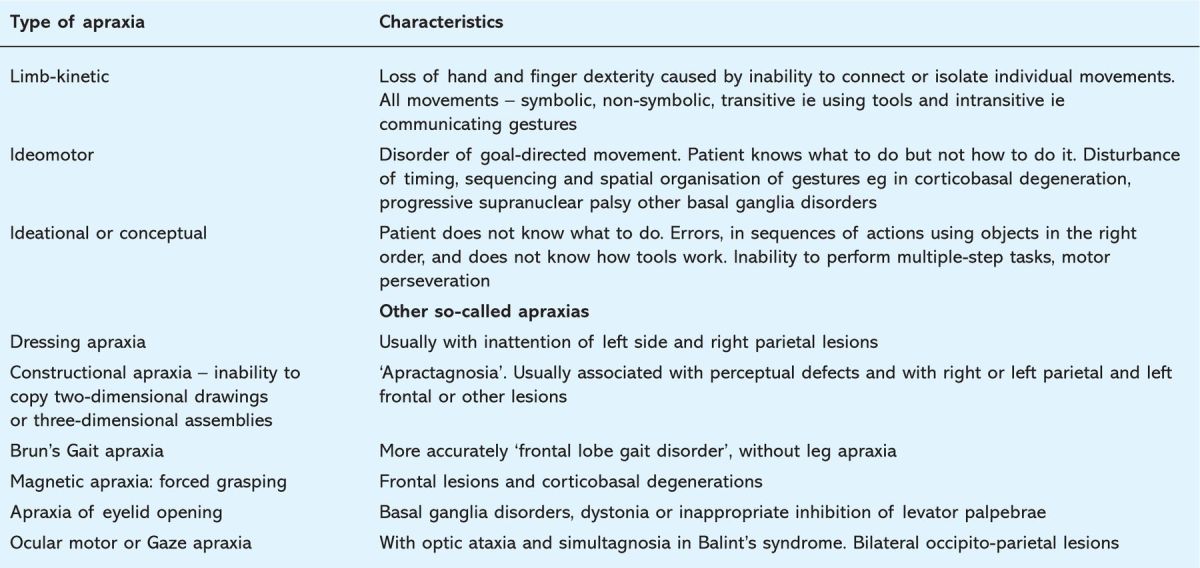
Brain diseases that damage the multiple parallel parietofrontal circuits devoted to specific sensorimotor transformations cause different praxic deficits, depending on the context in which the movement is performed and the cognitive demands of the action. Constructional, gait, facio-buccal, and ocular apraxias have their own distinctive clinical and neuropathological features. Whether they should fall within the general motor apraxias is arguable – an issue beyond the remit of this paper. There remains no consensus on the classification of apraxias (Table 1).
Table 1.
Characteristics of apraxias.
Hugo Karl Liepmann
Liepmann was born in 1863 in Berlin to cultured Jewish parents. After schooling, he graduated and obtained a PhD in philosophy, which remained a lifelong interest and was a background for his later investigations of ideation and psychophysical concepts. Seeking more tangible objectives for study, he read medicine, graduating in Berlin in 1894. He studied anatomy with Weigert, then went to Breslau under the wing of Wernicke. After four years he returned to Berlin to work at the psychiatric hospital of Dalldorf where he began his work on apraxia. He became Privatdozent at Berlin's University in 1901, but was never promoted to Professor Ordinarius because, according to Oskar Vogt, he was denied an academic post unless he was prepared to change from the Jewish to the Protestant faith which he refused to do. He later became director of the D Stadt, Irrenanst at Berlin-Herzberge, a mental institution, where he remained until he developed Parkinsonism, which precipitated his retirement. Goldenberg provided a full account of his life, and his style as a clinician, and reviewed his ideas on cerebral localisation of psychological function and apraxia.19 Goldstein reported that he had such high ethical standards that during the blockade of Germany in 1915–16 he voluntarily starved himself (losing 60 pounds in weight), refusing to eat more food than his patients were allowed. His daughter Kate, wrote in an epilogue: ‘his professional aspirations were continually thwarted in the context of anti-Semitism of his day and that this continual disappointment threw a shadow over Hugo Liepmann's life’.27 An English translation of his essays on apraxia has been published.28 His last years were clouded by professional frustrations and illness. Parkinson's disease crept up on him enforcing slowly increasing disabilities that culminated in his suicide in 1925. Kurt Goldstein remarked:
Liepmann's work will remain one of the landmarks in the progress of our knowledge of the function of the brain. He is a worthy representative of a great epoch in neurology.29
References
- 1.Geschwind N, Damasio AR. Apraxia. In: Vinken PJ, Bruyn GW, Klawans HL. (eds). Handbook of clinical neurology, vol 45 Amsterdam: Elsevier, 1985:423–32. 10.1007/978-94-010-2093-0_14 [DOI] [Google Scholar]
- 2.Leiguarda RC, Marsden CD. Limb apraxias. Higher-order disorders of sensorimotor integration. Brain 2000;123:860–79. 10.1093/brain/123.5.860 [DOI] [PubMed] [Google Scholar]
- 3.Liepmann H. Das Krankheitsbild der Apraxie (‘motorischen Asymbolie’) auf Grund eines Falles von einseitiger Apraxie. (The syndrome of apraxia (motor asymbolia) based on a case of unilateral apraxia). Translated by Bohne WHO, Liepmann K, Rottenberg DA. from Monatsschrift für Psychiatrie und Neurologie, 1900, vol 8:15–44. In: Rottenberg DA, Hochberg FH. (eds). Neurological classics in modern translation. New York: Hafner Press, 1977. [Google Scholar]
- 4.Liepmann H. Der weitere Krankheitsverlauf bei dem einseitig Apraktischen und der Gehirnbefund auf Grund von Serienschnitten. Monatschrift fur Psychiatrie und Neurologie 1905;17:289–311, 19: 217–43. [Google Scholar]
- 5.Liepmann H. Drei Aufsätze aus dem Apraxiegebiet. Berlin: Karger, 1908. [Google Scholar]
- 6.Liepmann H. Apraxie. Ergebn ges Med 1920;1:516–43. 10.1159/000203164 [DOI] [Google Scholar]
- 7.Wernicke K. Some new studies on aphasia. Fortschr Med 1885; 824–30. Translated in: Eling P. (ed), Reader in the history of aphasia. Amsterdam: John Benjamins, 1994: 90–8. [Google Scholar]
- 8.Lange J. In: Brown J. (ed). Agnosia and apraxia: selected papers of Liepmann, Lange and Potzl. New York: Erlbaum, 1988:136. [Google Scholar]
- 9.Jackson JH, 1861. Cited by Wilson SAK. A contribution to the study of apraxia with a review of the literature. Brain 1908;31:164–216. [Google Scholar]
- 10.Finkelnburg CM, 1870. Cited by Goldenberg G. Apraxia and beyond: life and work of Hugo Liepmann. Cortex 2003;39:509–24. [DOI] [PubMed] [Google Scholar]
- 11.Steinthal H. Abriss der Sprachwissenschaft (vol I: Einleitung in die Psychologie und Sprachwissenschaft, 1871), 2nd edn. Berlin: F Dummlers, 1881:167–71. [Google Scholar]
- 12.De Buck D. Les parakinésies. J Neurologique Belge 1889;20:361–74. [Google Scholar]
- 13.Pick A. Studien über motorische Apraxie und ihr nahestehende Erscheinungen: ihre Bedeutung in der Symptomatologie psychopathischer Symptomen-Komplexe. Leipzig: Deuticke, 1905. [Google Scholar]
- 14.Catani M, Ffytche DH. The rises and falls of disconnection syndromes. Brain 2005;128:2224–39 10.1093/brain/awh622 [DOI] [PubMed] [Google Scholar]
- 15.Geschwind N. Selected papers on language and the brain. Dordrecht, Holland: Reidel, 1974:52. 10.1007/978-94-010-2093-0 [DOI] [Google Scholar]
- 16.Liepmann H, Mass O. Ein Fall yon linksseitiger Agraphie. und Apraxie bei rechtsseitiger Lihmung. Monatsschr Psychiatr Neurol 1907;10:214–22. [Google Scholar]
- 17.Goldstein K. Zur Lehre der motorischen Apraxie. J Psychol Neurol 1908;11:169–87. [Google Scholar]
- 18.Brain WR. In: Speech disorders, aphasia, apraxia and agnosia. London, Butterworths, 1961:143–51. [Google Scholar]
- 19.Goldenberg G. Apraxia and beyond: life and work of Hugo Liepmann. Cortex 2003;39:509–24 10.1016/S0010-9452(08)70261-2 [DOI] [PubMed] [Google Scholar]
- 20.De Renzi E, Lucchelli F. Ideational apraxia. Brain 1988;111:1173–85. 10.1093/brain/111.5.1173 [DOI] [PubMed] [Google Scholar]
- 21.Geschwind N, Kaplan E. A human cerebral deconnection syndrome: a preliminary report. Neurology 1962;12:675. [DOI] [PubMed] [Google Scholar]
- 22.Sperry RW, Gazzaniga MS, Bogen JE. Interhemispheric relationships: the neocortical commissures; syndromes of hemisphere disconnection. In: Vinken PJ, Bruyn GW. (eds). Handbook of clinical neurology. Amsterdam: North-Holland Publishing Company, 1969:4, 177–84. [Google Scholar]
- 23.Geschwind N. Dysconnexion syndromes in animals and man. Part II. Brain 1965;88:604–26. [DOI] [PubMed] [Google Scholar]
- 24.Wernicke K. Recent works in aphasia. Originally published as Einige neue Arbeiten über Aphasie. Fortschritte der medizin. In: Wernicke's works on aphasia. The Hague: Mouton, 1977:173–205. [Google Scholar]
- 25.Wilson SAK. A contribution to the study of apraxia with a review of the literature. Brain 1908;31:164–216. 10.1093/brain/31.1.164 [DOI] [Google Scholar]
- 26.Zadikoff C, Lang AE. Apraxia in movement disorders. Brain 2005;128:1480–97. 10.1093/brain/awh560 [DOI] [PubMed] [Google Scholar]
- 27.Liepmann K, 1977 Cited by Code C, Wallesch C-W, Joanette Y, Lecours AR. Classic cases in neuropsychology. Hove: Psychology Press, 1996. [Google Scholar]
- 28.Liepmann H. Translations from Liepmann's essays on apraxia. London: Department of Psychology, University of Western Ontario, 1980 [Google Scholar]
- 29.Goldstein K. In: Haymaker W, Schiller F. (eds). The founders of neurology, 2nd edn. Springfield: Charles C Thomas, 1970:473–5. [Google Scholar]