Abstract
A cornerstone of the development of acute medicine has been the principle of consultant presence within the acute medical unit (AMU). There is the hypothesis that consultant supervision improves patient care. This view is not currently supported by firm scientific evidence. When Ipswich AMU opened in 2004, there was a consultant presence on some weekdays only. Admission data were collected and assessed with respect to the presence or absence of the consultant. Overall length of stay was significantly lower, by a mean of 1.3 days, when there was a consultant present, and 9% more patients were discharged on the same day of their assessment (95% confidence interval 5.7% to 12.6%, p<0.001) without affecting readmission or mortality. These results suggest the absence of a consultant leads to fewer same-day discharges and causes the inappropriate admission of patients not needing inpatient management. Further study is required to determine whether these findings are shared by other AMUs.
Key Words: acute, admission, consultant, cost, discharge, mortality, readmission
Introduction
The specialty of acute medicine has developed rapidly over the past few years. Acute medical units (AMUs) are now found in virtually every secondary and tertiary referral hospital in the UK.1 The specialty is an integral part of the Acute Care Common Stem training programme and training numbers in acute medicine continue to expand rapidly.2
Prior to the development of acute medicine, the traditional model would involve a team of junior doctors admitting patients during the day. The on-call consultant would arrive to conduct an admissions ward round in the evening or the following morning at which time definitive patient management decisions would be made.
One of the cornerstones of the development of acute medicine has been direct consultant presence within the AMU in order to expedite the clinical decision-making process.3 It has been postulated that this will bring a range of benefits including reduction in admission and readmission rates, reduced length of stay and improved patient care (including reduced mortality).1,3 However, there is at present little supportive evidence for these intuitive benefits.
In many AMUs, a consultant-led service has been introduced as the units themselves have developed. This has presented a challenge in studying the effect of the consultant presence alone. A group in Bournemouth found that following the introduction of an acute physician there was a reduction in medical outliers.4 There was also a fall in the admission rate year on year. However this fall coincided with a progressive expansion of the AMU bed numbers. It is therefore unclear whether the consultant presence or the expansion of the admission unit facilities improved the discharge rate. Internationally, Moloney and colleagues showed that introduction of an admissions unit in Dublin without a consultant presence led to a reduction in length of hospital stay with resulting cost benefits.5 A study in a rural district hospital in Australia showed that the presence of an emergency physician resulted in reduced admission rates, reduced ordering of pathology tests and also a reduction in specialty referral.6 The majority of published data to date focuses on the effect of the existence of the admissions unit rather than the putative benefit of the grade of clinical staff supporting it.7
At the Ipswich Hospital, a purpose-built AMU was opened in late 2004. Part of the initial design of this unit incorporated a single consultant presence on four days out of five during the working week. The consultant would be present on the unit from 09.00 until 17.00. The main aims of the consultant presence within the AMU were to expedite the clinical decision-making process and improve patient care by targeting early review of each patient as they arrived in the unit. This early consultant review would lead to earlier ordering of diagnostic investigations. The consultant would order the majority of diagnostic imaging and follow it up in real time, although no designated investigation capacity was allotted to the acute medicine consultant nor were there any formal arrangements for early reporting of scans. The same proactive ethos would be used when dealing with referral to medical specialties and social care. The consultant would use one-to-one contact to ensure rapid and timely review of patients within the AMU.
Each day's medical take would be coordinated around an admissions list in the AMU reception area. Following review, the consultant would identify whether a patient was likely to require discharge, short-stay admission or long-stay admission. The nurse coordinator would then, at an early stage, be able to plan likely admission destination or discharge arrangements. The consultant did not have access to a rapid returns clinic. On occasion, when clinical review was indicated, the patient could be brought back to the AMU on an ad hoc basis.
On the days when the consultant was not on duty, there would be no routine consultant presence until a post-take ward round commenced at 19.00. However, in all other aspects the AMU would be run in the same way. This design gave a unique opportunity to compare outcomes on the weekdays when a consultant was and was not present on the AMU, over the same time period.
Method
The Ipswich Hospital information department provided a list of admissions to the AMU from 1 January 2005 to the 31 August 2005, between the hours of 09.00 and 16.30. The data for weekends and bank holidays, when a skeleton service was in operation, were removed. The list was divided into two groups: weekdays when the consultant was (Monday, Tuesday, Thursday and Friday) and was not (Wednesdays and other weekdays when the consultant was on annual leave) present on the unit.
Pearson's chi-squared test was used to assess for any differences in demographic (sex and age) and admission characteristics (day and method of admission) between the two patient groups. The arithmetic mean was chosen as the recommended statistic to describe length of stay. Trends in mean length of stay across each demographic and admission characteristic, and diagnostic group were analysed as differences in two means or trends across categories with confidence intervals (CIs) and p values obtained using the nonparametric bootstrap percentile method.8 Length of stay was further assessed between groups in terms of percentage of Day 0, 1, 2, 3, 4–7 and over 7 discharges. Readmission and mortality rates were estimated for each group and compared by estimating the difference in proportions with 95% CI. All tests were two sided and assessed at the 5% level of significance.
Results
Basic demographics
A total of 2,928 patients were assessed in the AMU during the period of analysis: 2,064 (70%) were assessed on a day when there was a consultant presence in the AMU and 864 (30%) were assessed when there was not.
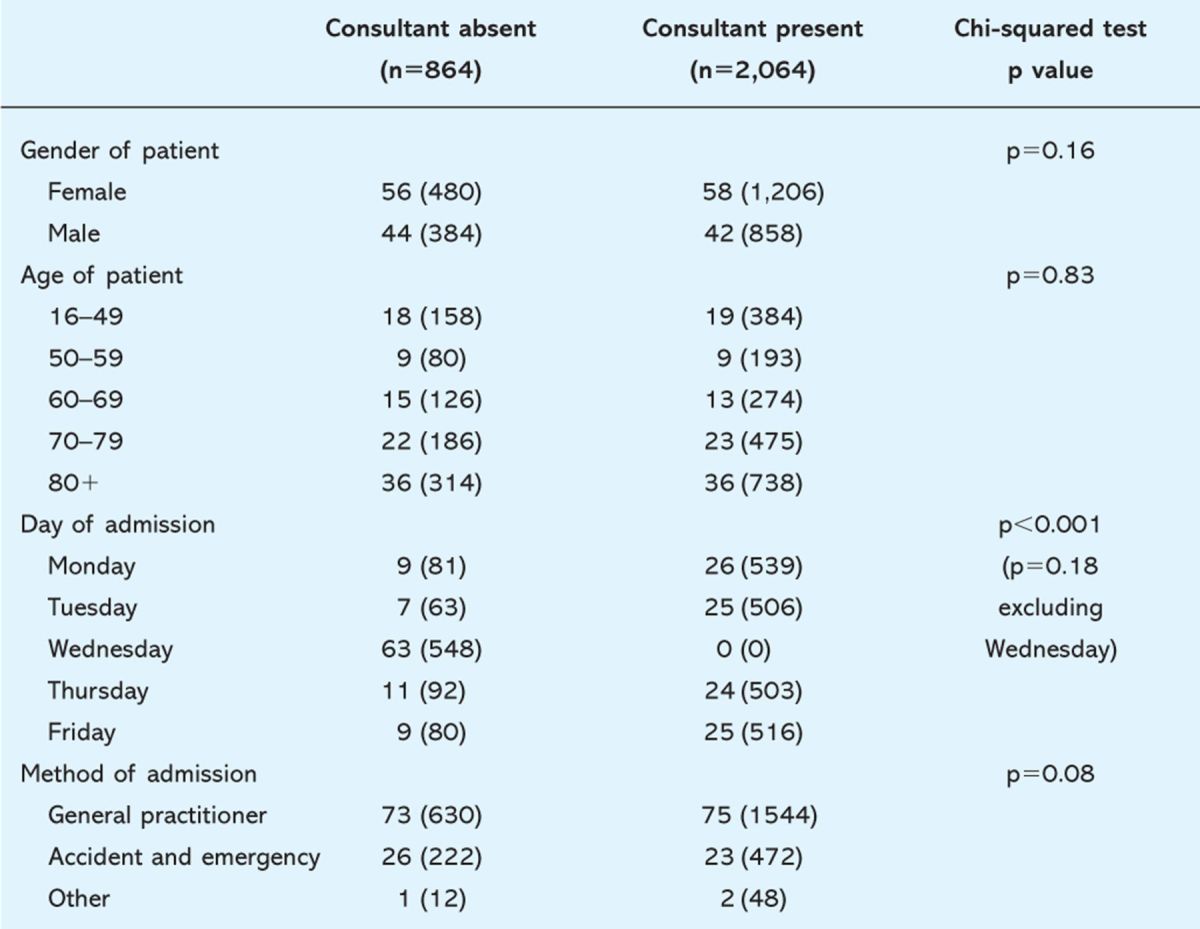
Demographic and admission characteristics were analysed to check that their distribution was similar in both groups. There were no statistically significant differences in terms of gender, age and method of admission (Table 1). There was a statistically significant difference in distribution of days of the week between the two groups. However, it was known when the study was designed that the consultant was never present on the AMU on Wednesdays, and there was no evidence of a difference across the other days of the week.
Table 1.
Comparison of patient demographic and admission characteristics by presence of consultant. Summary statistics are percentages (number in brackets).
Length of stay
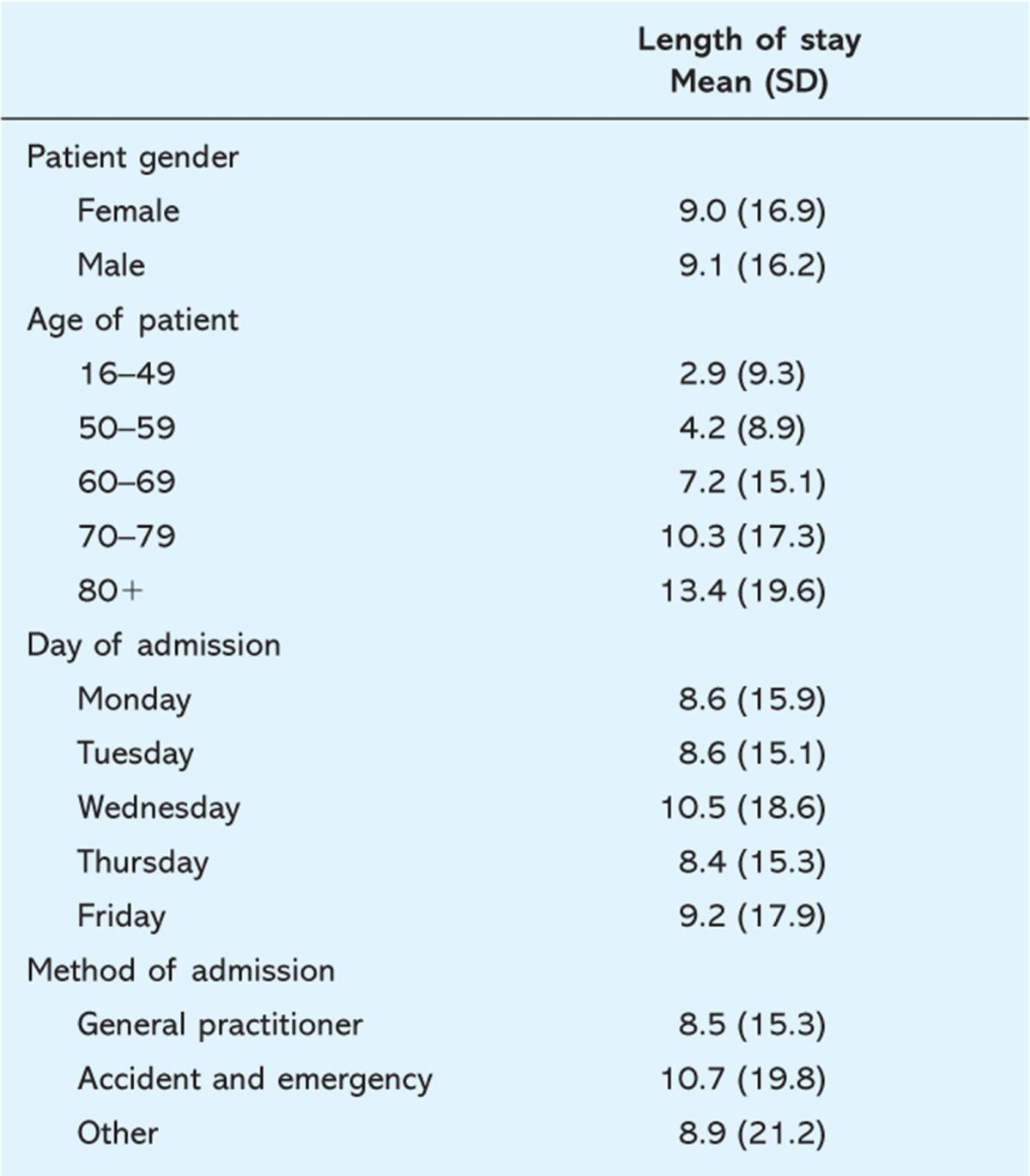
The effect of demographic variables and admission characteristics on length of stay was initially evaluated. It was found that there was no evidence of a difference in mean length of stay between men and women (p = 0.82) or by day of the week admitted. Those admitted from accident and emergency tended to have a longer length of stay (p = 0.01). There was a strong trend in mean length of stay with increasing patient age (p<0.001, Table 2). However, the age of patients and the method of admission were very similarly distributed between the groups (Table 1). It has been concluded that these factors have not confounded any potential association between the presence of a consultant and length of stay.
Table 2.
Length of stay in association with patient demographic and admission characteristics. Summary statistics are mean (standard deviation (SD) in brackets).
Effect of consultant presence
Mean length of stay (excluding inpatient deaths) was significantly lower when the consultant was present on the AMU: 7.72 v 9.06 days with a reduction (95% CI) of 1.34 days (0.01 to 2.67), p = 0.048.
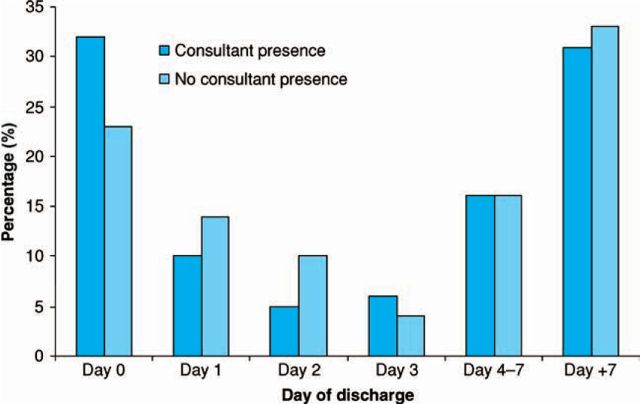
The greatest effect was seen in those who had shorter admission durations. Although the percentage discharged in less than three days was very similar between the two groups, 46.6% and 46.9% (Table 3), the results suggest that the presence of a consultant increases those discharged immediately and reduces those admitted for one to two days (Fig 1). The proportion discharged on Day 0 when the consultant was present was 32.2% (95% CI: 30.2% to 34.2%). The proportion discharged on Day 0 when the consultant was absent was 23.0% (95% CI: 20.2% to 25.8%). This difference in proportion discharged on Day 0 when the consultant was present compared to when absent was highly statistically significant (95% CI 5.7% to 12.6%, p<0.001). In particular, in the group with the consultant presence, 4.1% fewer patients stayed for one day of admission and a further 4.8% fewer patients stayed for two days.
Table 3.
Distribution of length of stay by consultant group. Summary statistics are mean (standard deviation (SD) in brackets).
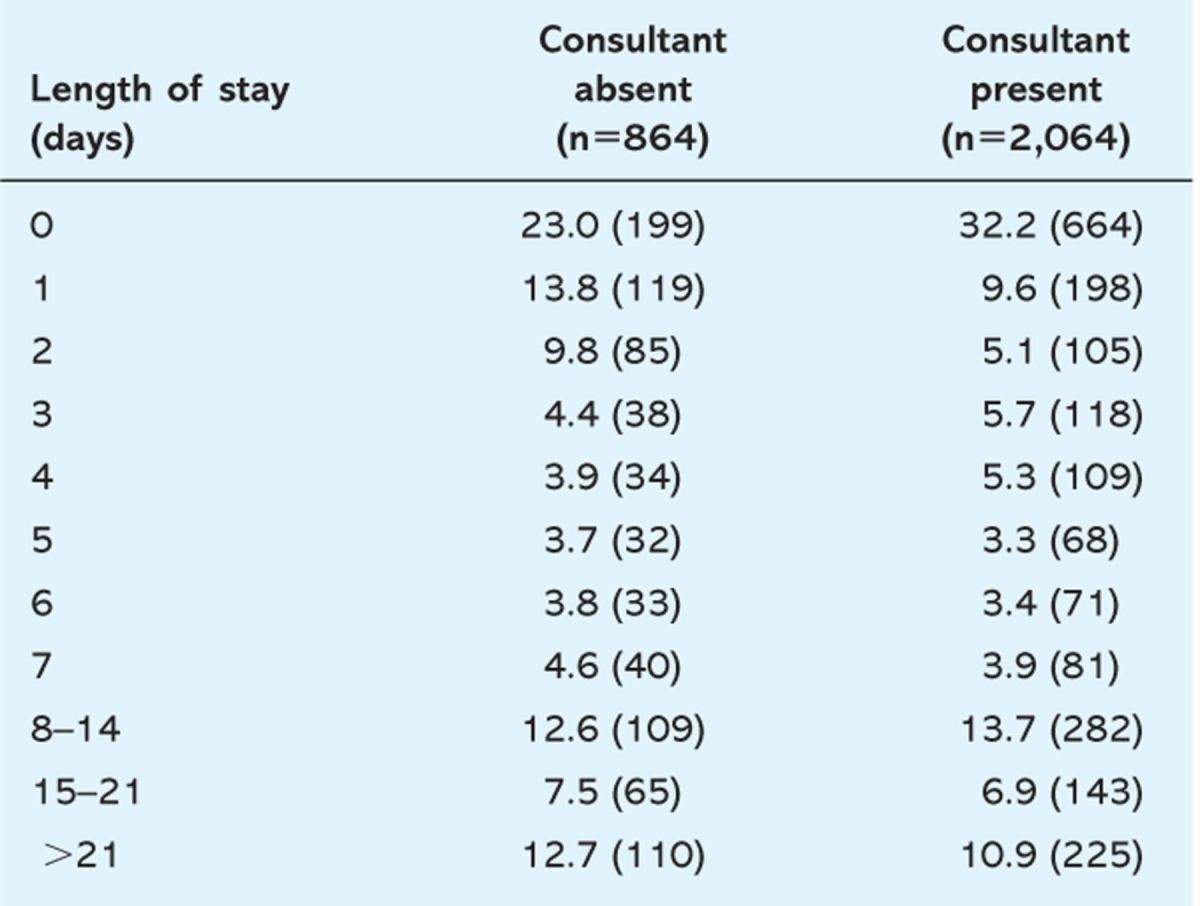
Fig 1.
Comparison of length of stay (days) by whether consultant present or absent.
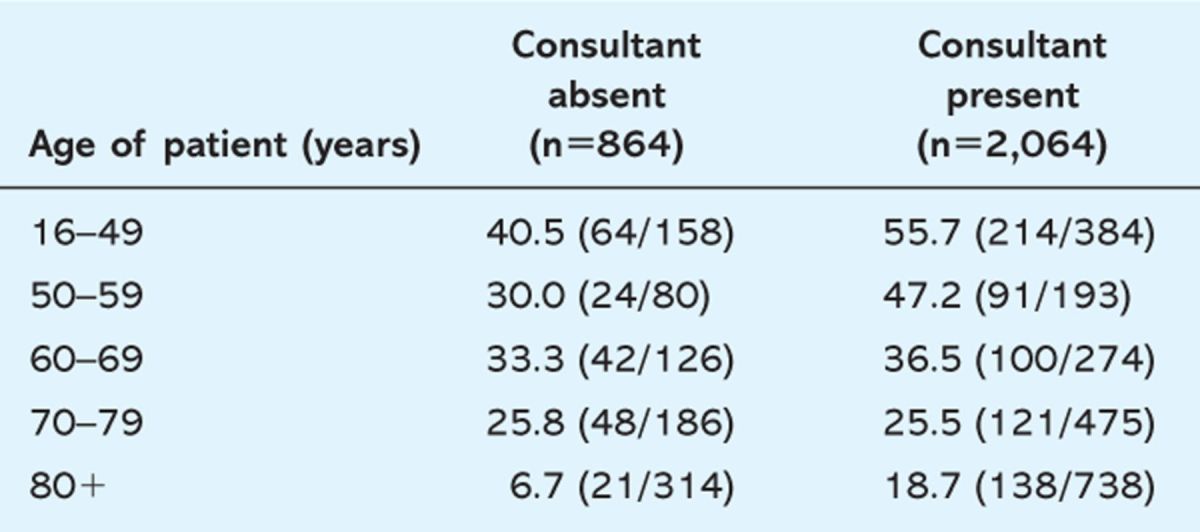
The proportion of those immediately discharged was consistently higher when the consultant was present across days of the week, method of admission and differing diagnostic groups. However, there was significant variation (p=0.001) across age groups in the differential in rate of immediate discharge (Table 4). In particular, immediate discharge was more cautious in those aged 80 or over when the consultant was absent, and when the consultant was present a greater proportion of patients aged less than 60 were discharged on the day of admission.
Table 4.
Proportion of patients discharged on day of admission by whether consultant present or absent stratified by age of patient. Summary statistics are percentages (number in brackets).
Readmissions
The percentage of patients being readmitted within 30 and 60 days of discharge were analysed within each group. Of the patients assessed when the consultant was present, 10.5% were readmitted within 30 days of discharge. When there was no consultant presence on the day of admission, 10.2% of patients were readmitted within 30 days of discharge (Table 5).
Table 5.
Proportion of patients readmitted by whether consultant present or absent.
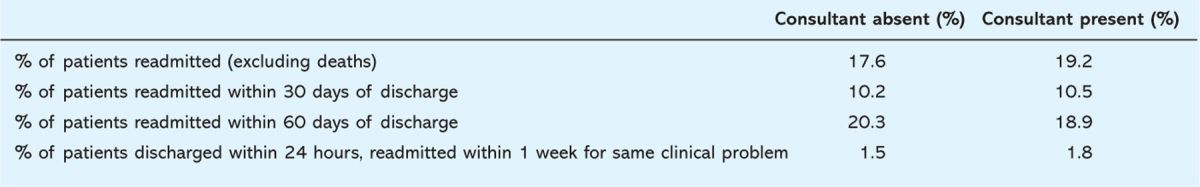
Early readmission rates of patients that had been sent home within 24 hours of admission were also analysed. In total, 2.4% of these patients were readmitted within one week when the consultant was present and 2.1% were readmitted in the consultant's absence.
Following case notes review, it was noted that 1.8% of these Day 0 discharges were readmitted within a week for the same clinical problem when the consultant was present. In total, 1.5% of patients were readmitted within one week with the same clinical problem when the consultant was absent (p = 1).
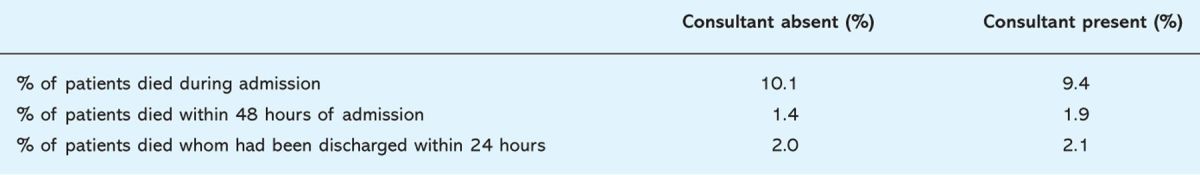
Mortality
Of the patients admitted when the consultant was present on the day of admission, 9.4% died during that admission. Of patients admitted when there was no consultant present, 10.1% died during their admission. This was not statistically significant (p = 0.55).
It was postulated that a senior clinical presence in the AMU may affect the rates of mortality immediately following admission. Mortality within 48 hours of admission was therefore calculated. Given the differing Day 0 discharge rates, mortality in those patients who had been discharged within 24 hours was also analysed (Table 6). There were no significant differences.
Table 6.
Proportion of patients who died by whether consultant present or absent.
Discussion
It appears that the presence of a consultant in the AMU does affect the patient journey. Overall length of stay in patients who were discharged alive was significantly reduced when the consultant was present on the day of admission.
The most significant effect of a consultant presence within the AMU was seen in short-stay patients. Our study has shown that the percentage of patients staying in hospital for 72 hours or less were the same whether a consultant was present within the AMU or not. However when the consultant was not present, 9% fewer patients were discharged on the same day of their assessment. This might suggest that, in the absence of a consultant in the AMU, patients who could have been discharged the same day were admitted overnight and discharged the following day. The lack of senior support until the 19.00 post-take ward round did appear to lead to delayed management decisions. Even if patients were identified as fit for discharge, arranging patient care and transport may not have been possible at this late hour.
It was observed that despite 9% more patients being discharged on the same day of assessment when the consultant was present, this had no statistically significant affect on rates of readmission. There were no significant differences in mortality rates between the two groups either.
There are clear limitations to this study. Although we have shown that the consultant impacted on the patient journey, it is not known whether the presence of different consultants will have the same impact. This is an observational study and there remains a difference in the particular weekday on which the data were collected. More information is needed regarding the nature of patients discharged on the same day of assessment as well as the particular interventions that facilitated the discharge.
When considering these results within the scope of previous work,1,4,5 there is now clear evidence to support both the concept of AMUs and the seniority of staffing required to ensure the maximum benefits are achieved. This study suggests the main effect of a consultant in the AMU is to prevent admission without any deleterious effects on mortality or readmission rates. There is also a significant, if less dramatic effect, on reducing overall length of admission. These findings have significant cost implications. Further study is required to determine whether the findings are shared by other AMUs.
Reference
- 1.National Confidential Enquiry into Patient Outcome and Death. Emergency admissions: a journey in the right direction? London: NCEPOD, 2003. [Google Scholar]
- 2.Joint Royal Colleges of Physicians Training Board. Acute medicine curriculum for higher medical training. London: JRCPTB, 2003. [Google Scholar]
- 3.Royal College of Physicians. Acute medicine: making it work for patients - A blueprint for organisation and training. Report of a working party. London: RCP, 2002. [Google Scholar]
- 4.Armitage M, Raza T. A consultant physician in acute medicine: the Bournemouth Model for managing increasing numbers of medical emergency admissions. Clin Med 2002; 2(4): 331–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moloney ED, Smith D, Bennett K. Impact of an acute medical admission unit on length of hospital stay, and emergency department ‘wait times’. QJM 2005; 98(4): 283–9. [DOI] [PubMed] [Google Scholar]
- 6.Donald KJ, Smith AN, Doherty S, Sundararajan V. Effect of an on-site emergency physician in a rural emergency department at night. Rural Remote Health 2002; 5(3):380. [PubMed] [Google Scholar]
- 7.Cooke MW, Higgins J, Kidd P. Use of emergency observation and assessment wards: a systematic literature review. Emerg Med J 2003; 20(2): 138–42. 10.1136/emj.20.2.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ 2000; 320:1197–200. 10.1136/bmj.320.7243.1197 [DOI] [PMC free article] [PubMed] [Google Scholar]