Autosomal dominant polycystic kidney disease (ADPKD) is an inherited disease with a prevalence of 1:400 to 1:1,000 live births.1 It is the most common genetic cause of renal failure, accounting for 10% of patients on dialysis. ADPKD is a systemic disorder characterised by progressive kidney enlargement, cyst formation in other organs (liver, pancreas) and non-cystic complications (arterial aneurysm).
Genetics and pathophysiology
Inheritance of ADPKD is autosomal dominant with 100% disease penetrance. Each offspring has a 50% chance of inheriting the disease. There is a 5% rate of new mutation. Mutations in either of two genes coding for membrane proteins can lead to ADPKD:1
PKD1 (chromosome 1613.3), 85–90% of cases, encodes for the polycystin-1 protein
PKD2 (chromosome 4q21), 10–15% of cases, encodes for the polycystin-2 protein.
A small number of families unlinked to either gene could indicate the potential existence of a third gene (PKD3). PKD1 and PKD2 gene mutations have similar clinical phenotype, but PKD2 patients have a more favourable course. The mean age of onset of end-stage renal failure (ESRF) is 53 years for PKD1 and 69 years for PKD2. Unlike PKD1, women with PKD2 have a later onset of ESRF than men.
Natural history
Patients are usually asymptomatic until the middle decades, but 2–5% present in childhood with significant morbidity. By the age of 60, 50% of patients with ADPKD will require renal replacement therapy. Poor prognostic indicators for renal survival include male sex, black race, haematuria before age 30, multiple pregnancies, hypertension before age 35, proteinuria, renal size and PKD1 mutation. ADPKD patients do not have a higher risk of mortality than other patients with ESRF. The main cause of mortality is cardiovascular disease (36% of cases).2
Clinical features
Pain
Renal: acute pain due to infection, stones, intracystic haemorrhage and urinary tract obstruction; chronic pain due to pressure, stretching of the renal capsule or structural distortion.
Non-renal: liver and pancreatic enlargement or infection.
Hypertension
Hypertension is a common early finding – in 60% of patients with normal renal function.
Urinary tract infection
About 30–50% of patients will have an episode of urinary tract infection in their lifetime.
Cyst haemorrhage and haematuria
Gross haematuria occurs in 30–50% of ADPKD patients, with rising incidence as kidney size increases. It usually occurs spontaneously but may be related to physical activity, trauma, stones, infection or tumour.
Nephrolithiasis
Nephrolithiasis occurs in 20–30% of patients. The presence of renal calculi should be considered if acute pain, acute deterioration in renal function and haematuria are present.
Massive polycystic kidneys and large renal cysts
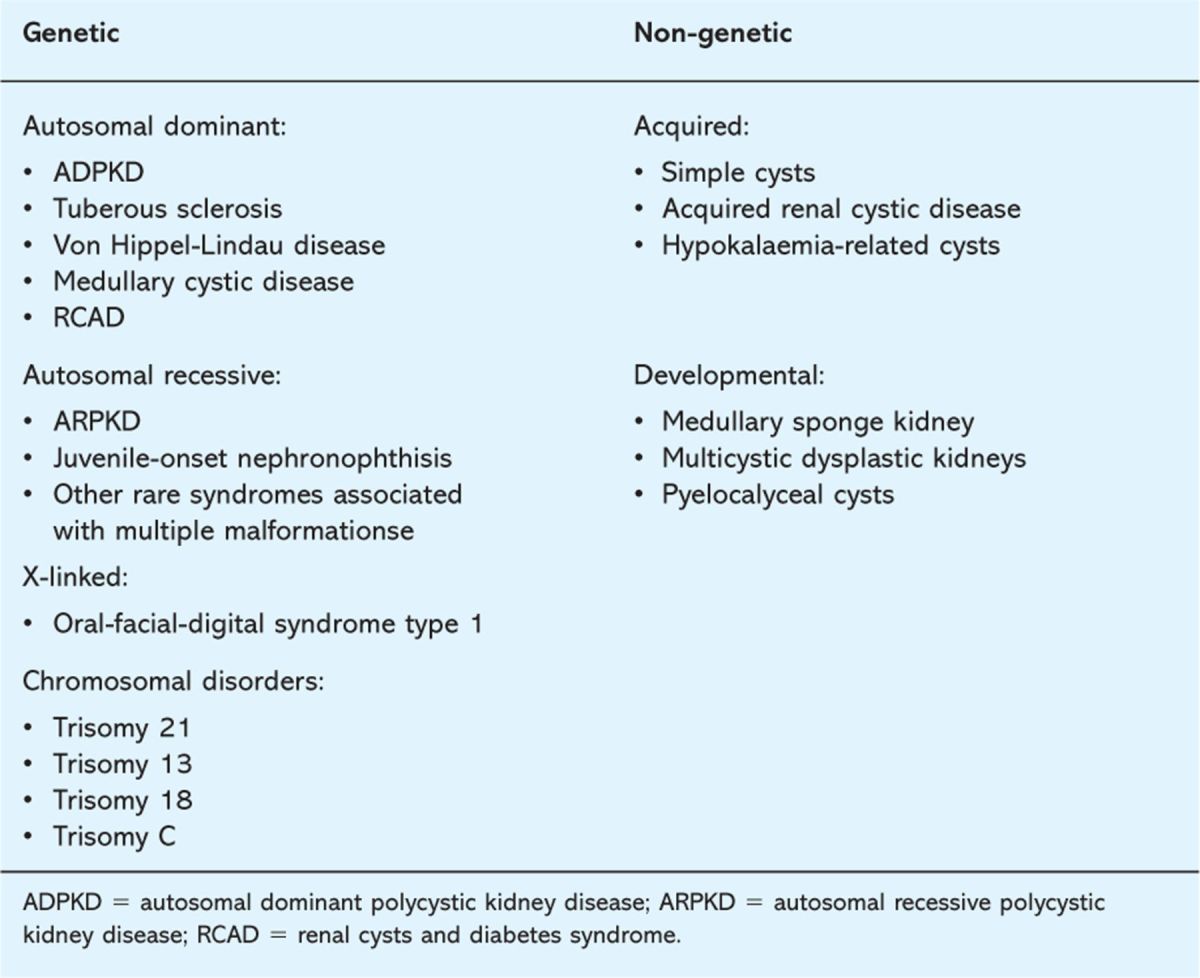
Abdominal discomfort or pain can be caused by massive cysts. Renal cysts are not unique to ADPKD. Other potential causes are given in Table 1.
Table 1.
Renal cystic diseases.
Cancer
There is no evidence for an increased risk of renal cell carcinoma in the ADPKD population, but haematuria and flank pain with anorexia and weight loss should prompt further investigation.
Liver cysts
Hepatic cysts are the most common extrarenal manifestation, increasing with older age (58% in the third decade and 94% in the fourth decade on magnetic resonance imaging (MRI).3 They occur more frequently and severely in females, correlating with oestrogen exposure (eg pregnancy, contraceptive pill).4 They are usually asymptomatic and do not lead to hepatic failure. Pain from compression, feeling of satiety, cystic haemorrhage and infection are the most common symptoms. Rarely, massive polycystic liver disease (female preponderance) can result in portal hypertension.3 Rare cases of congenital hepatic fibrosis have also been described.5
Intracerebral aneurysms
Intracerebral aneurysms (ICA) occur in 6% of ADPKD patients without a family history of ICA and in 16% of patients with a positive family history of ICA.6 However, the most common neurological event in ADPKD is hypertensive haemorrhage or ischaemic stroke.
Symptoms of chronic kidney disease
Lethargy, poor appetite, reduced urine volume, fluid retention etc are all symptoms of chronic kidney disease (CKD).
Pancreatic cysts
Although pancreatic cysts occur in 9% of patients older than 20 years, this is not related to pancreatic dysfunction.7
Investigation
Table 2 lists the investigations used in assessing ADPKD patients.
Table 2.
Investigations.

New unified diagnostic ultrasound criteria for at-risk PKD1 and PKD2 individuals have recently been reported (Table 2).8 The previously used criteria had a sensitivity of 100% in PKD1 patients aged 30 years or older but false-negative rates for PKD2 (23%) and PKD1 (5%) in younger patients. Where the family history is unknown or negative, these new criteria may not apply and mutation analysis may be indicated for either disease exclusion or diagnostic purposes.8,9 Clinically, the presence of bilateral enlarged cystic kidneys with hepatic cysts and absence of positive extrarenal manifestations (suggesting an alternative cystic disease) make the diagnosis highly probable.
Fig 1.
End-stage autosomal dominant polycystic kidneys.
The Consortium for Radiologic Imaging Studies of PKD (CRISP) suggests that the rate of disease progression can be monitored through serial MRI kidney volume measurements prior to significant decline in glomerular filtration rate.10
Management
There is no cure for ADPKD. Treatment is aimed at blood pressure control, prompt treatment of infections and disease complications, and the management of CKD.
Pain
Pain should be treated with simple analgesia. Lifestyle modification and avoidance of aggravating activities can also be useful.3 Patients may require pain clinic referral and surgical management (cyst decompression, renal denervation or nephrectomy).
Hypertension
The aim is to achieve a blood pressure below 130/80 mmHg.15 There is no specific evidence that any particular antihypertensive drug is more effective in ADPKD. A trial currently in progress, Halt Progression in PKD (HALT-PKD), is investigating whether the use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers confers additional benefit.
Urinary tract infection
Urine cultures may be persistently negative in cyst infection. Ureteric obstruction from stone or clot with associated infection should be excluded. Patients will require prompt antibiotic treatment adjusted to renal function and culture results. Cyst infection requires antibiotics that penetrate the cyst (eg macrolides, ciprofloxacin, trimethoprim etc). A prolonged course of antibiotics may be required. Surgical intervention is occasionally indicated. In the presence of recurrent infection, it would be prudent to consider long-term prophylactic antibiotics.15
Cyst haemorrhage and haematuria
Conservative management with bed rest, hydration and analgesia is the mainstay of therapy for cyst haemorrhage and haematuria as bleeding is normally self-limiting and resolves within days.15 Further investigation to exclude malignancy may be considered if episodes are frequent and/or prolonged (especially in patients over 50 years old) or if other systemic symptoms are present. Rarely, haemodynamically significant bleeding can occur, requiring hospital admission, transfusion and computed tomography with or without angiography. Persistent haemorrhage may require segmental arterial embolisation (coils) or nephrectomy.
Fig 2.
Ultrasound scan showing multiple cysts within the kidney.
Fig 3.
Computed tomography scan showing bilateral enlarged polycystic kidneys.
Nephrolithiasis
Renal stones normally resolve with conservative measures: hydration, treatment of infection and analgesia. More complicated cases should be referred for extra-corporeal shockwave lithotripsy and percutaneous nephrostolithotomy.3
Massive polycystic kidneys and large renal cysts
Cyst reduction by alcohol sclerosis, percutaneous drainage or laparoscopic deroofing are options. Laparoscopic renal denervation can be considered in rare cases of uncontrolled pain.3 Nephrectomy is indicated for massive kidneys (occupying surgical space) in a transplant work-up, severe resistant recurrent infection, severe pain or malignancy.
Key Points
Autosomal dominant polycystic kidney disease is a common genetic disease due to mutations in two genes, PKD1 and PKD2
Patients may present with or develop significant extrarenal manifestations
The main aim of therapy is directed at blood pressure control, prompt treatment of infections, addressing cardiovascular risk and treating the complications of chronic kidney disease
Renal ultrasound remains the major screening method
Unified diagnostic criteria for at-risk individuals have been published
Liver cysts
Infection will require antibiotics with good cyst penetration, often given for a long course. If the infection does not settle, patients may require cyst drainage or hepatectomy in rare cases. If there are problems with satiety that impact on nutrition or severe discomfort, a surgical debulking procedure could be considered.3
Intracerebral aneurysms
The likelihood of rupture of an aneurysm smaller than 7 mm in diameter is 0.1% per year in patients with no history of subarachnoid haemorrhage. The potential benefits of prophylactic surgery have to be balanced against the risks of the surgical complications. Conservative management is recommended for aneurysms smaller than 7 mm in the anterior circulation.16,17 Larger aneurysms are treated by coil embolisation or surgical clipping.
If an aneurysm larger than 7 mm in diameter is detected, follow-up surveillance scans will be required.17 Control of hypertension and hyperlipidaemia, and termination of smoking are advised. The risk of a new aneurysm developing after an initial negative study is about 2.6% at 10 years in patients with a positive family history of ICA.18
Chronic kidney disease and renal replacement therapy
Both peritoneal dialysis and haemodialysis can be used in ADPKD patients. Transplantation is the treatment of choice but pre-emptive nephrectomy may be required if kidneys are massively enlarged. There is no difference in patient or graft survival in ADPKD patients compared with other ESRF populations.15 However a threefold increased risk of developing new-onset diabetes after transplantation in ADPKD has recently been reported.19
Family screening
Patients should be advised to inform at-risk blood relatives of the diagnosis and the need for screening. At consultation, the inheritance pattern should be explained, with advice on methods of presymptomatic diagnosis, including the possibility of prenatal diagnosis. Each at-risk individual should be informed of the consequences of diagnostic screening, including the possibility of false-negative ultrasound tests in younger patients.
Making a decision to diagnose
Pros
early management of complications
family planning
absence of ADPKD reassures patient.
Cons
psychological consequences as no specific treatment or cure is available at present
insurance and employment issues.
Family members who opt not to have screening should be advised to have yearly checks on renal function, blood pressure and urinalysis, and to inform their general practitioner of their risk of developing ADPKD.
Fig 4.
Pathological specimen of PKD2 knockout mouse kidneys showing kidney enlargement due to multiple cysts.
Pregnancy
There should be preconception counselling and referral to specialist renal and obstetric services. Prenatal diagnosis by chorionic villous sampling can be done at the ninth week of pregnancy. This is not performed routinely due to high intrafamilial phenotypic variability. Prenatal screening may be considered in families with one severely affected child (early-onset PKD) who have a calculated 45% recurrence risk for following pregnancies.20
The risk of worsening renal function and complications in pregnancy are higher in the presence of moderate-to-severe renal impairment, proteinuria and hypertension. Hypertensive complications, including new and worsening hypertension, have been reported in 25% of patients, with pre-eclampsia in 11%.
Future prospects
Several promising candidate drugs have commenced phase 3 clinical trials, based largely on their efficacy in rodent models of PKD:
A multicentre trial of tolvaptan, a vasopressin type 2 receptor antagonist, commenced in 2007.21
Octreotide, a somatostatin analogue,22 has been shown to inhibit kidney growth in a small phase 2 crossover study.
Rapamycin,23 phase 3 clinical trials of sirolimus and everolimus (a derivative of rapamycin) have commenced.
Reference
- 1.Ong AC, Harris PC. Molecular pathogenesis of ADPKD: the polycystin complex gets complex. Kidney Int 2005; 67: 1234–47. 10.1111/j.1523-1755.2005.00201.x [DOI] [PubMed] [Google Scholar]
- 2.Fick GM, Johnson AM, Hammond WS, Gabow PA. Causes of death in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 1995; 5:2048–56. [DOI] [PubMed] [Google Scholar]
- 3.Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet 2007; 369:1287–301. [DOI] [PubMed] [Google Scholar]
- 4.Vora N, Perrone R, Bianchi DW. Reproductive issues for adults with autosomal dominant polycystic kidney disease. Am J Kidney Dis 2008; 51:307–18. 10.1053/j.ajkd.2007.09.010 [DOI] [PubMed] [Google Scholar]
- 5.Cobben JM, Breuning MH, Schoots C, ten Kate LP, Zerres K. Congenital hepatic fibrosis in autosomal-dominant polycystic kidney disease. Kidney Int 1990; 38:880–5. 10.1038/ki.1990.286 [DOI] [PubMed] [Google Scholar]
- 6.Pirson Y, Chauveau D, Torres V. Management of cerebral aneurysms in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 2002; 13:269–76. [DOI] [PubMed] [Google Scholar]
- 7.Torra R, Nicolau C, Badenas C. et al Ultrasonographic study of pancreatic cysts in autosomal dominant polycystic kidney disease. Clin Nephrol 1997; 47:19–22. [PubMed] [Google Scholar]
- 8.Pei Y, Obaji J, Dupuis A. et al Unified criteria for ultrasonographic diagnosis of ADPKD. J Am Soc Nephrol 2008; 20:205–12. 10.1681/ASN.2008050507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravine D, Gibson RN, Walker RG. et al Evaluation of ultrasonographic diagnostic criteria for autosomal dominant polycystic kidney disease 1. Lancet 1994; 343:824–7. 10.1016/S0140-6736(94)92026-5 [DOI] [PubMed] [Google Scholar]
- 10.Grantham JJ, Torres VE, Chapman AB. et al Volume progression in polycystic kidney disease. N Engl J Med 2006; 354:2122–30. 10.1056/NEJMoa054341 [DOI] [PubMed] [Google Scholar]
- 11.Rossetti S, Consugar MB, Chapman AB. et al Comprehensive molecular diagnostics in autosomal dominant polycystic kidney disease. J Am Soc Nephrol 2007; 18:2143–60. 10.1681/ASN.2006121387 [DOI] [PubMed] [Google Scholar]
- 12.Garcia-Gonzalez MA, Jones JG, Allen SK. et al Evaluating the clinical utility of a molecular genetic test for polycystic kidney disease. Mol Genet Metab 2007; 92:160–7. 10.1016/j.ymgme.2007.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Connor A, Lunt PW, Dolling C. et al Mosaicism in autosomal dominant polycystic kidney disease revealed by genetic testing to enable living related renal transplantation. Am J Transplant 2008; 8:232–7. 10.1111/j.1600-6143.2007.02030.x [DOI] [PubMed] [Google Scholar]
- 14.Consugar MB, Wong WC, Lundquist PA. et al Characterization of large rearrangements in autosomal dominant polycystic kidney disease and the PKD1/TSC2 contiguous gene syndrome. Kidney Int 2008; 74:1468–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grantham JJ. Clinical practice. Autosomal dominant polycystic kidney disease. N Engl J Med 2008; 359:1477–85. [DOI] [PubMed] [Google Scholar]
- 16.Gibbs GF, Huston J, 3rd, Qian Q. et al Follow-up of intracranial aneurysms in autosomal-dominant polycystic kidney disease. Kidney Int 2004; 65:1621–7. 10.1111/j.1523-1755.2004.00572.x [DOI] [PubMed] [Google Scholar]
- 17.Wiebers DO, Whisnant JP, Huston J., 3rd et al Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003; 362:103–10. 10.1016/S0140-6736(03)13860-3 [DOI] [PubMed] [Google Scholar]
- 18.Schrier RW, Belz MM, Johnson AM. et al Repeat imaging for intracranial aneurysms in patients with autosomal dominant polycystic kidney disease with initially negative studies: a prospective ten-year follow-up. J Am Soc Nephrol 2004; 15:1023–8. 10.1097/01.ASN.0000118527.74850.66 [DOI] [PubMed] [Google Scholar]
- 19.Hamer RA, Chow CL, Ong AC, McKane WS. Polycystic kidney disease is a risk factor for new-onset diabetes after transplantation. Transplantation 2007; 83:36–40. 10.1097/01.tp.0000248759.37146.3d [DOI] [PubMed] [Google Scholar]
- 20.Zerres K, Rudnik-Schöneborn S, Deget F. Childhood onset autosomal dominant polycystic kidney disease in sibs: clinical picture and recurrence risk. German Working Group on Paediatric Nephrology (Arbeitsgemeinschaft für Pädiatrische Nephrologie). J Med Genet 1993; 30:583–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang X, Gattone V, 2nd, Harris PC, Torres VE. Effectiveness of vasopressin V2 receptor antagonists OPC-31260 and OPC-41061 on polycystic kidney disease development in the PCK rat. J Am Soc Nephrol 2005; 16:846–51. 10.1681/ASN.2004121090 [DOI] [PubMed] [Google Scholar]
- 22.Grantham JJ. Does extended-release somatostatin slow the growth of renal cysts in autosomal-dominant polycystic kidney disease? Nat Clin Pract Nephrol 2006; 2:66–7. 10.1038/ncpneph0082 [DOI] [PubMed] [Google Scholar]
- 23.Wahl PR, Serra AL, Le Hir M. et al Inhibition of mTOR with sirolimus slows disease progression in Han:SPRD rats with autosomal dominant polycystic kidney disease (ADPKD). Nephrol Dial Transplant 2006; 21:598–604. 10.1093/ndt/gfi181 [DOI] [PubMed] [Google Scholar]






