Abstract
Ward rounds are a vital part of hospital medicine and junior doctors play a key role in their delivery. Despite the importance of ward rounds to patient care and experience, we believe that junior doctors may lack the training and skills to carry them out most effectively. We designed a simulation-based training session focusing on ward round skills themed to key patient safety issues and have delivered the training to over 100 learners (medical students and foundation year one doctors). Few learners had any prior training in ward rounds. The session was highly valued by all participants and surveys completed both before and after the session showed statistically significant improvements in confidence in leading and documenting ward rounds. In addition, 94% of final year medical students and 93% of doctors felt such training should be included in the undergraduate curriculum. We believe there is a current gap in training around ward round skills and would strongly encourage simulation-based ward round training to be developed for undergraduates. Further sessions following qualification may then consolidate and develop ward round skills adapted to the level of the doctor.
KEYWORDS : Ward round, simulation, junior doctors, education
Introduction
As the predominant point of doctor–patient interaction, ward rounds can significantly influence patient experience as well as ensure high-quality, safe care for patients.1,2 The joint RCP/RCN publication Ward rounds in medicine: principles for best practice3 highlights the significant variation in terms of current organisation and practice of ward rounds. It recommends rounds that have clear structure and strong leadership for maximum effectiveness. Most consultant job plans allow for only two ward rounds a week, so many rounds are led by junior doctors.
Whether leading or participating, the roles that junior doctors play in ward rounds are central to their delivery. In return, ward rounds offer many teaching and learning opportunities.4 In recent years ward rounds have become both time pressured and discharge focused, so additional effort is required to ensure that their educational potential is not lost. Medical students first encounter ward rounds during undergraduate placements but, to our knowledge, receive little in the way of formal training and may lack essential ward-round skills at qualification.5 As postgraduates, communication skills and patient safety feature heavily in foundation curricula, but the ability to lead or participate in a structured, safe, ward round is not specifically referred to.6
Hectic and time-pressured situations can compromise quality and increase the chance of error. In ward rounds this could translate into hurried, unsafe practice in which key elements are missed, eg it has been demonstrated that less thorough ward rounds can lead to poorer outcome in surgical patients.7 Just as importantly, chaotic rounds are likely to have a negative effect on patient experience. Medical ward safety checklists have been developed as one way of ensuring systematic review following the successes of the WHO Surgical Safety Checklist.8 There are several forms of ward safety checklists, which are often tailored to the individual specialty or organisation. Some are mnemonic and others evaluative, aiming to reduce errors of omission.9 They also serve as a valuable teaching and training tool.10 Supporters of medical checklists exalt their value in terms of small interventions made that improve patient care, but empirical evidence for reducing morbidity and mortality is still awaited. Simply introducing a checklist is not enough; realisation of its true potential requires education, communication and culture change.11
Simulation with deliberate practice has been accepted as a superior training method when compared with conventional clinical education.12 It is widely used in in anaesthetics, intensive care and emergency medicine, and increasingly in general medicine. A simulated ward environment has been validated as a means of assessing ward-based processes of surgical care.13 We believe that the opportunity to learn through focused, repetitive practice in a safe environment is ideally suited to the teaching of ward-round etiquette for all specialties.
Methods
To improve ward-round practice at our Trust and adopt the use of a ward safety checklist, an educational session was designed, in a simulated environment, for final year medical students and junior doctors. To do this it was first necessary to determine the current level of knowledge and practice among the junior doctors. In June 2012, 6 months before the initial pilot sessions were run, junior doctors working in the trust were invited to participate in an anonymous online survey, with the aim of understanding current practice and areas of focus for the design of the educational session; 72 junior doctors responded to the survey (58% response rate). Of these 35% were foundation year 1 and 65% were foundation year 2 grade or above. Of the respondents, 55% were working in the medical division whereas the remainder worked in other specialties (eg surgery, emergency medicine, general practice). Of all the respondents, 15% had had some form of training in performing ward rounds. Of junior doctors, 49% rated themselves as confident leading the ward round (rating themselves 4 or 5 (on a 5-point scale)), and 63% stated that they always reviewed thromboprophylaxis although only 38% reviewed allergy status or prescription charts routinely; 28% reviewed resuscitation status and 48% reviewed ceiling of care for the patients.
Current practice
Surrey and Sussex Healthcare NHS Trust runs acute services at East Surrey Hospital in Surrey, which serves a population of approximately 550,000. Consultant-led ward rounds occur as a minimum twice a week, and many specialties use daily consultant-led board rounds. At other times ward rounds are led by registrar or senior house officer grade (core medical trainee, specialty trainee 1/2, foundation year 2) doctors. All consultant rounds aim to have at least one other person in attendance (physician associates and other junior doctors). Many wards aspire to having a senior nurse on the round, including elderly care and gastroenterology, but this not universal. The use of ward safety checklists, in the form of stickers that are completed as part of the ward-round documentation, is standard practice within the medical division.
Development of the ward-round simulation training
We developed a three-hour, simulation-based, ward-round session. Learners were split into two groups, with each group attending two sessions: a group tutorial and a simulation session. Half the group had the tutorial first and the other half the simulation. The tutorial was problem based and discussed common ward-based scenarios and patient safety issues relevant to ward-round activities. The simulation session involved three ward-round encounters with an actor (a physician associate) in the role of the patient within a simulated ward environment. Learners who were not taking part in the scenario acted as observers through a viewing window. Each observer was given a specific area to focus and make comment on, eg patient safety or communication skills. A learner was nominated to be the ward-round leader and to delegate role and responsibilities to the ‘ward team’. Roles included one person to document, one to complete the safety checklist and another to check the patient folder containing observations and drug chart. False documentation was provided for the patient, including medical clerking and ward-round notes, modified early warning scores, fluid and prescription charts, and investigation results.
Themed scenarios were developed, eg a patient with uncontrolled pain, another with a drug error and another with an antibiotic-related drug rash. Ward safety checklists were used in each scenario to introduce the idea of structure and format. Learners were assigned different roles within the scenarios but, due to group size, not all learners had the opportunity to lead. The ‘de-brief’ allowed leaders, participants and observers to talk through the scenario, assess their performance and revise the key learning points.
Sessions were run for four groups of final year medical students (n = 72) during 2012–13 and for all foundation year 1 doctors (n = 30) during their induction in August 2013. Learners were invited to complete anonymous feedback surveys both before and after the training. They were asked about previous ward-round training and completed ratings of confidence in leading and documenting ward rounds.
Statistical analysis
As the surveys were voluntary not all students responded to the pre- and post-surveys. Survey results before and after training were analysed using R Version 3.02 and the coin package. Participant's confidence was measured using a Likert scale (1–5, with 5 being the highest value). As the surveys were anonymous it was not possible to analyse them as paired groups (before and after training) or use statistical tests that assume normal continuous distribution of data points. Instead rank transformations were applied to the values and these were compared using the Wilcoxon–Mann–Whitney test, with exact p values derived using the coin package in R. Statistical significance was taken as p<0.05.
Results
Pre-training medical student and foundation year 1 doctor survey (at induction)
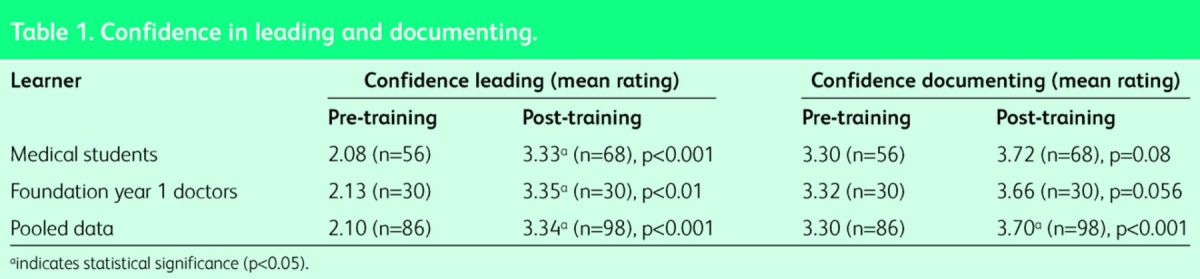
Of the 72 medical students, 56 completed the pre-training survey as well as all 30 foundation doctors. Only 9% of medical students and 27% of foundation doctors had prior ward-round training. Only five medical students and one foundation doctor had prior training in simulation format. Self-rated confidence in leading rounds was poor (medical students mean rating 2.08 and foundation doctors 2.13). Confidence was higher in documenting the ward round (medical students mean rating 3.30 and foundation doctors 3.32).
Post-training analysis (completed at the end of the session)
Of the 72 final year medical students, 68 completed a post-training survey as well as all 30 foundation doctors. The average simulation group size was eight, with half the group working as the ward team and the other half as observers. Only three people had the opportunity to lead the simulated round in each session. Learners were asked to rate the educational session as a whole (the tutorial and the simulation training). Of students and foundation doctors, 100% felt that the session was useful and 93% rated the session as very good or excellent. Self-rated confidence in leading ward rounds increased significantly in the medical student and foundation year doctors. Results suggested improved confidence in documentation, but this did not reach statistical significance when analysed as two groups. Statistically significant improvements in confidence in both leading and documenting rounds were seen when both datasets were combined (Table 1).
Table 1.
Confidence in leading and documenting.
Of the respondents, 85% felt that the ward safety checklist improved confidence on the ward round. Of the students, 92% felt that further sessions would be useful and 94% that it should be incorporated into their undergraduate teaching. In addition, 90% of foundation doctors would value further sessions; similarly 90% felt that the training should be offered before starting the foundation year, and 93% would encourage incorporation into the undergraduate curriculum.
The six-month survey
Foundation doctors who took part in the induction session were invited to complete a survey at six months; 17 responses were received. Of the 17, 11 (65%) felt that the training had been useful in preparing them for their ward-round duties and the mean confidence rating was 3.19 for leading and 4.13 for documenting the ward rounds.
Discussion
The surveys issued to junior doctors and final year medical students highlight a possible gap in training around ward-round practice. This may explain the low levels of confidence in leading a ward round. As a result, medical students and foundation doctors may miss the opportunity to participate fully in ward-round encounters and this may be to their educational disadvantage. Without clearly assigned roles and responsibilities, it is also easy to see how key elements of a round could be overlooked. Junior doctors are an obvious vehicle for changing culture towards patient safety14 and the ward-round training can allow reinforcement of key patient safety issues via the theming of scenarios. One of our scenarios, for example, focused on safe prescribing.
Low-cost and low-technology simulation can be highly effective in situations where non-practical skills are tested15 and use of this format for ward-round training appears to be useful to all our learners. The sessions are easily reproducible without the need for state-of-the-art simulation facilities and do not have a high financial cost. Our training sessions were run by a lecturer, two facilitators and an actor (who was a physician assistant). Training for larger groups does, however, increase the time and faculty requirement to run the sessions. Feedback from the medical students suggests that they would prefer small groups to allow more opportunity to lead a scenario. Although this would, no doubt, enrich the training experience, our results showed that the training improved confidence in all learners irrespective of the role that they played.
Although the training appeared to increase confidence in leading and documenting a ward round, demonstration of improved competence is more difficult in practice. Audit of the junior doctor ward round notes and direct observation are at best only crude measurements of competence because external factors are likely to influence the interaction and the vital patient's perspective is missed. The lack of clear definition as to what constitutes a ‘good’ ward round makes it difficult to derive measurable quality standards. What is a ‘good’ ward round for the doctor may not be ‘good’ for the patient.
The ward-round simulation training may be more effective if delivered earlier in undergraduate training. Students may further their knowledge, confidence and experience by better integration and participation during hospital attachments and, as doctors, may settle into the foundation year more readily. Our six-month survey, although small, demonstrates that learners felt that the session had been useful in preparing them for their role, but the confidence scores suggest that further sessions during the foundation year may help to consolidate the learning.
The training may also benefit other members of the multidisciplinary team and reaffirm their value in the ward-round process. The training should not be an isolated session but part of an ongoing programme adapted to the level of the learner. Our trust has now joined neighbouring trusts, and Brighton and Sussex Medical School and, with facilitation by Kent Surrey and Sussex Deanery, will be developing a quality ward-round project to deliver multidisciplinary ward-round training across the region during 2014–15.
Conclusion
We suggest that many junior doctors lack confidence to perform and lead ward rounds, perhaps due to a lack of undergraduate experience and training. As a result junior-led ward rounds may affect patient safety and experience. Simulation ward-round training is well received by medical students and junior doctors, and improves confidence in leading and documenting ward rounds. In a busy modern hospital where continuity of care is often suboptimal, it is imperative that the junior staff providing much of the patient contact are confident and trained to do so. The author suggests that ward-round training is essential for all medical students and junior doctors if we are to ensure the safety of patients in the hands of future doctors.
Acknowledgements
We acknowledge the help of Dr Des Holden, Medical director of the Surrey and Sussex Healthcare NHS Trust, Dr Martin Parry, Associate director of the South West Thames Foundation School, Dr Wes Scott-Smith and Dr Neal Gent who form part of the Quality Ward Round Project and Dr Gordon Caldwell of the Western Sussex NHS Foundation Trust.
References
- 1 .Herring R, Desai T, Caldwell G. Quality and safety at the point of care: how long should a ward round take? Clin Med 2011;11:20–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2 .Cohn A. Restore the prominence of the medical ward round. BMJ 2013;347:f6451. [DOI] [PubMed] [Google Scholar]
- 3 .Royal College of Physicians and Royal College of Nursing Ward round in medicine: principles for best practice. London: RCP, 2013. Available online at www.rcplondon.ac.uk/resources/ward-rounds-medicine-principles-best-practice [Accessed 15 March 2014]. [Google Scholar]
- 4 .Claridge A. What is the educational value of ward rounds? A learner and teacher perspective. Clin Med 2011;11:558–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5 .Nikendei C, Kraus B, Schrauth M, Briem S, Jünger J. Ward rounds: how prepared are the future doctors? Med Teach 2008;30:88–91. [DOI] [PubMed] [Google Scholar]
- 6 .Academy of Medical Royal Colleges The UK foundation programme curriculum 2012. London: Academy of Medical Royal Colleges, 2012. Available online at www.foundationprogramme.nhs.uk/pages/home/curriculum-and-assessment/curriculum2012 [Accessed 15 March 2014]. [Google Scholar]
- 7 .Pucher PH, Aggarwal R, Darzi A. Surgical ward round quality and impact on variable patient outcomes. Ann Surg 2014;259:222–6. [DOI] [PubMed] [Google Scholar]
- 8 .Weiser T, Haynes A, Lashoher A, et al. Perspectives in quality: designing the WHO Surgical Safety Checklist. Int J Qual Health Care 2010;22:365–70. [DOI] [PubMed] [Google Scholar]
- 9 .Hales, B, Terblanche M, Fowler R, Sibbald W. Development of medical checklists for improved quality of patient care. Int J Qual Health Care 2008;20:22–30. [DOI] [PubMed] [Google Scholar]
- 10 .Mohan N, Caldwell G. A considerative checklist to ensure safe daily patient review. Clin Teach 2013;10:209–13. [DOI] [PubMed] [Google Scholar]
- 11 .Amin Y, Grewcock D, Andrews S, Halligan A. Why patients need leaders. Introducing a ward safety checklist. J R Soc Med 2012;105:377–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12 .McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results that traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med 2011;86:706–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13 .Pucher PH, Aggarwal R, Srisatkunam T, Darzi A. Validation of the simulated ward environment for assessment of ward-based surgical care. Ann Surg 2014;259:215–21. [DOI] [PubMed] [Google Scholar]
- 14 .Lemer C, Moss F. Patient safety and junior doctors: are we missing the obvious? BMJ Qual Saf 2013;22:8–10. [DOI] [PubMed] [Google Scholar]
- 15 .Zendejas B, Wang AT, Brydges R, et al. Cost: the missing outcome in simulation based medical education research: a systematic review. Surgery 2013;153:160–6. [DOI] [PubMed] [Google Scholar]


