ABSTRACT
Vitamin B12 deficiency is a common condition which can present with non-specific clinical features, and in severe cases with neurological or haematological abnormalities. Although classically caused by pernicious anaemia, this condition now accounts for a minority of cases and vitamin B12 deficiency occurs most often due to food-bound cobalamin malabsorption. Since missing the diagnosis can result in potentially severe complications, including degeneration of the spinal cord and pancytopaenia, vitamin B12 deficiency must be diagnosed early and managed appropriately. Intramuscular injections have been the mainstay of treatment, but oral replacement therapy can be effective in many cases. There is accumulating evidence that high vitamin B12 levels (values varied from 350-1,200 pmol/l) are associated with haematological and hepatic disorders, in particular with malignancy. This review focuses on the developments in the clinical features and management of vitamin B12 deficiency over the last decade.
KEYWORDS : B12, cobalamin, deficiency, vitamin
Introduction
Vitamin deficiencies are a common problem worldwide, with vitamin B12 deficiency being recognised as a health concern nearly 100 years ago. The definition of vitamin B12 (cobalamin) deficiency varies with the assay used.1 Diagnostic criteria include a serum cobalamin <148 pmol/l (200 ng/l) in the presence of signs and symptoms and/or haematological indices of vitamin B12 deficiency, or a serum cobalamin <148 pmol/l in conjunction with elevated serum homocysteine or methylmalonic acid (MMA).2 Although serum homocysteine concentrations of 15 μmol/l and MMA levels of 0.27 μmol/l indicate the upper limit of normality, it is important to note that the British Society for Standards in Haematology (BCSH) recommend that laboratories in which these metabolites can be measured establish their reference ranges on an individual basis.2 In this review, the terms vitamin B12 and cobalamin will be used interchangeably, with ‘vitamin B12’ used for clinical purposes and ‘cobalamin’ for laboratory measurements.
In the United States, it has been demonstrated that the prevalence of vitamin B12 deficiency varies by age range, affecting at least 3% of those aged 20–39 years old, 4% of those aged 40–59 years, and 6% of those 60 years or over.3 Marginal depletion, defined in this study as a serum cobalamin of 148–221 pmol/l, affects 15% of those aged 20–59 years old and more than 20% of those aged 60 years or over.
Vitamin B12 metabolism
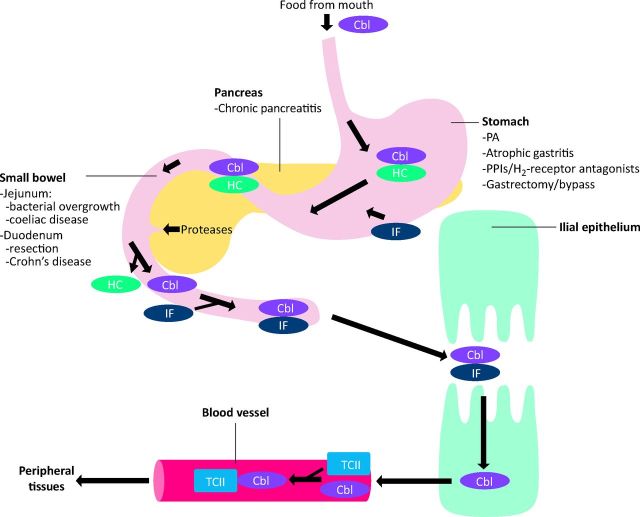
Vitamin B12 is obtained from dietary sources such as meat, eggs and dairy products.4 Individuals consume about 2.4 μg vitamin B12 per day, of which only 50-60% is absorbed.5 The sequence of events which results in the absorption of vitamin B12 is depicted in Fig 1,6 with the intracellular metabolism detailed in Fig 2.1,7
Fig 1.
Pictorial representation of the absorption of vitamin B12 (cobalamin). Dietary vitamin B12 is found in association with food proteins, and must be released on exposure to the low pH within the gastric lumen to facilitate absorption in the small bowel. Once liberated, vitamin B12 is immediately bound by haptocorrin (transcobalamin I) and remains attached until proteolytic cleavage of the complex in the duodenum. Here, it is available to bind intrinsic factor (IF), a second carrier protein, synthesised by the parietal cells of the gastric mucosa. IF is necessary for uptake of vitamin B12 in the terminal ileum. On traversing the brush border, vitamin B12 dissociates from IF, and enters the circulation where it binds transcobalamin II or haptocorrin. Transcobalamin II and haptocorrin are responsible for delivery of cobalamin to peripheral tissues and the liver, respectively. Cbl = cobalamin; HC = haptocorrin; IF = intrinsic factor; PA = pernicious anaemia; PPI = proton pump inhibitor; TCII = trancobalamin II.
Fig 2.
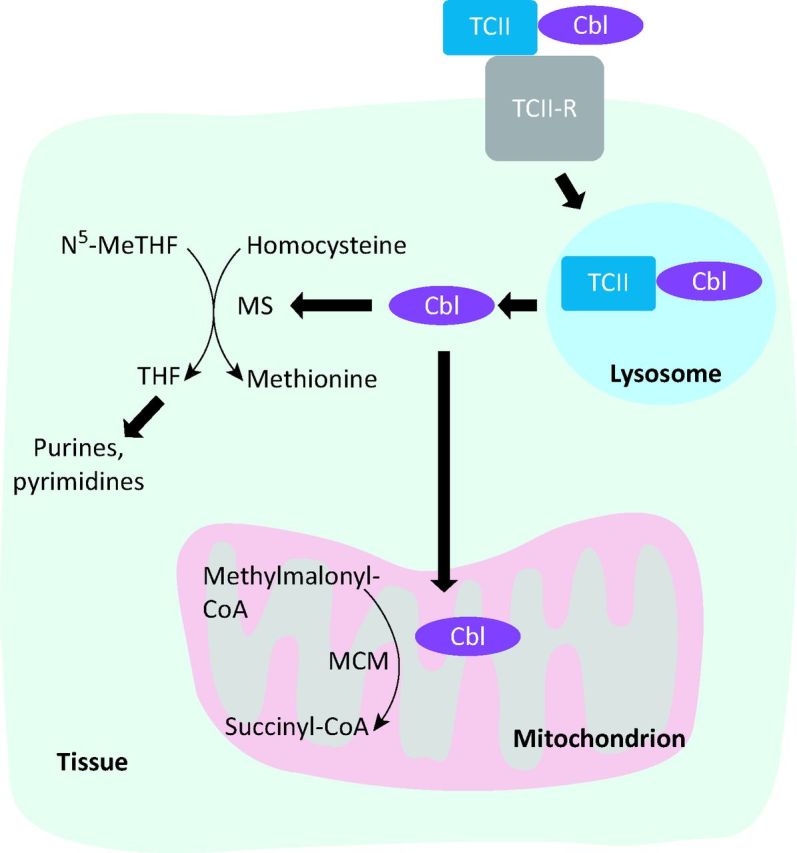
Intracellular metabolism of vitamin B12. Following transport to peripheral tissues, free vitamin B12 is generated. In the cytosol, vitamin B12 (Cbl) is used as a cofactor by MS to react homocysteine with N5-MeTHF to produce methionine and THF. Synthesis of THF affords the downstream generation of purines and pyrimidines required for DNA and RNA synthesis, explaining the clinical features of deficiency. The only other vitamin B12-dependent reaction is the conversion of methylmalonyl CoA to succinyl CoA by methylmalonyl CoA mutase, occurring in the mitochondria. Cbl = cobalamin; MCM = methylmalonyl-CoA mutase; MS = methionine synthase; N5-MeTHF = N5-methyltetrahydrofolate; TCII = transcobalamin II; TCII-R = transcobalamin II receptor; THF = tetrahydrofolate.
Following absorption, large amounts of vitamin B12 are stored in the liver; consequentially, any reduction in vitamin B12 intake may take 5–10 years to manifest itself clinically.8 A small proportion (1–5%) of free vitamin B12 is absorbed from the intestine by passive diffusion in an intrinsic factor (IF)-independent process. This supports the use of oral formulations instead of intramuscular injections for the vitamin deficiency (discussed later).
What causes vitamin B12 deficiency?
The complex absorption mechanisms render various ways by which vitamin B12 deficiency can develop, as detailed in Fig 1 and Table 1.1,2 In the classical ‘pernicious anaemia’, autoimmune destruction of parietal cells and consequent impairment of IF secretion is the cause.9 Although a well known cause of vitamin B12 insufficiency,10 pernicious anaemia now accounts for a minority of all cases. Vitamin B12 deficiency also occurs from poor dietary intake in malnourished patients, such as the elderly, and with alcohol excess.
Table 1.
Causes of low vitamin B12 levels.
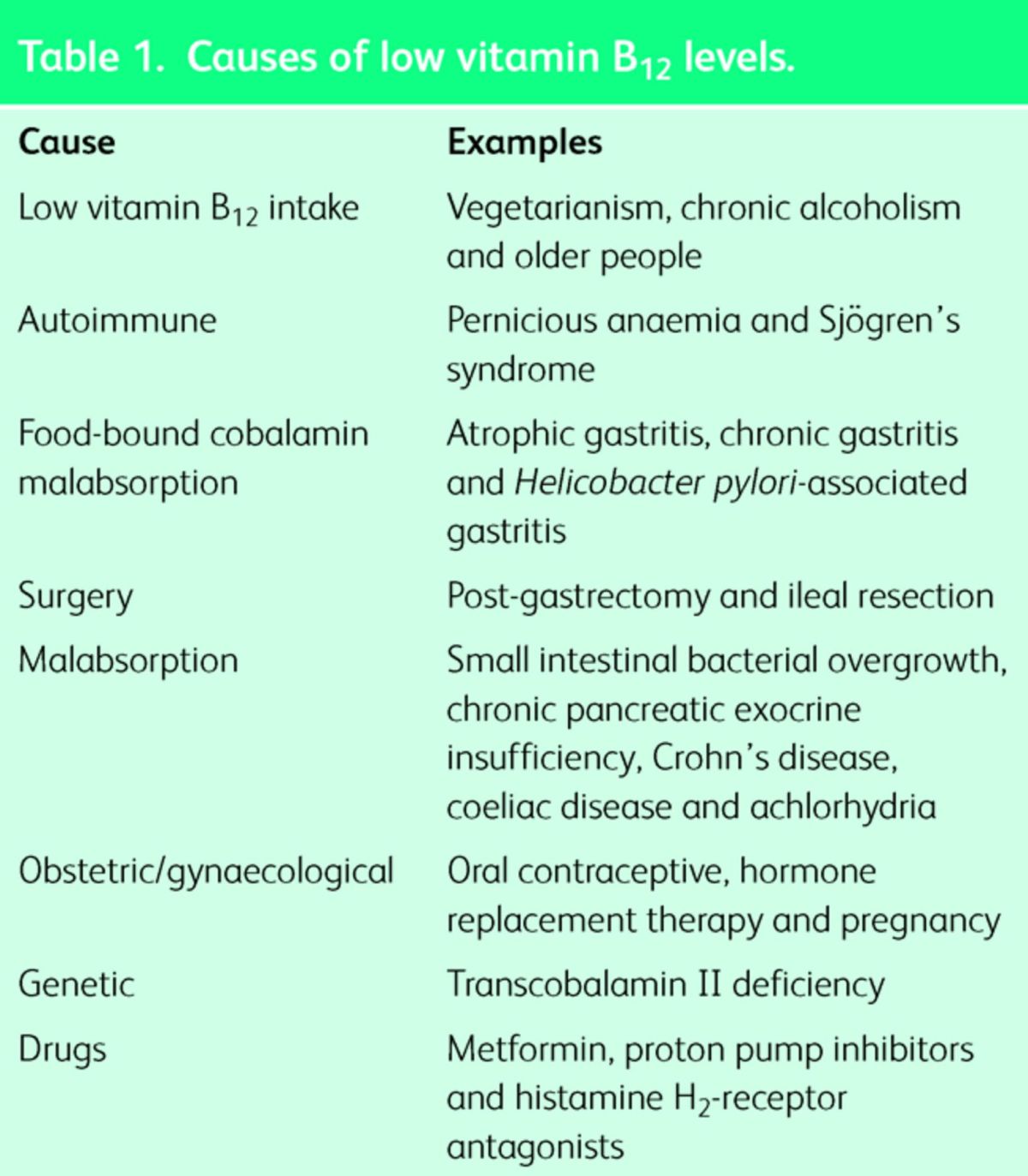
The commonest cause nowadays is food-bound cobalamin malabsorption (FBCM).1 In FBCM, there is impaired release of vitamin B12 from ingested food.1 One factor common to many of the conditions which can lead to FBCM is the inability to release vitamin B12 from its transport proteins. For example, achlorhydria, gastritis, gastrectomy and use of proton pump inhibitors (PPIs) or antacids, result in decreased secretion of hydrochloric acid, thereby reducing the liberation of vitamin B12 from food proteins.8 An IF-dependent transport mechanism remains intact in this setting, explaining the milder symptoms observed in these patients. A recent trial demonstrated a dose- and time-dependent association between use of PPIs or histamine H2-receptor antagonists and the future development of vitamin B12 insufficiency.11 The risk decreased significantly following drug discontinuation. Widespread use of acid-suppressing agents can thus lead to vitamin B12 deficiency which may go unnoticed due to lack of awareness. Use of metformin also has a similar impact on vitamin B12 levels, as revealed by de Jager et al who found that metformin was associated with a significant decrease in serum cobalamin, with a greater risk of deficiency in the future.12 The change in cobalamin was accompanied by a rise in serum homocysteine, which the authors noted may further increase the risk of development of cardiovascular disease in patients with type 2 diabetes mellitus. A recent systematic review confirmed the link between metformin treatment and low serum cobalamin levels, but highlighted that an association between vitamin B12 deficiency and clinical symptoms remains controversial.13
When should vitamin B12 deficiency be suspected?
Lack of vitamin B12 is characterised by haematological and neurological effects, ranging from milder manifestations such as fatigue and paraesthesiae, to severe features like pancytopaenia and degeneration of the spinal cord.1 Symptoms are detailed in Table 2,1,10,14 but the following may also be considered in relation to vitamin B12 deficiency.
Table 2.
Clinical manifestations of vitamin B12 deficiency.
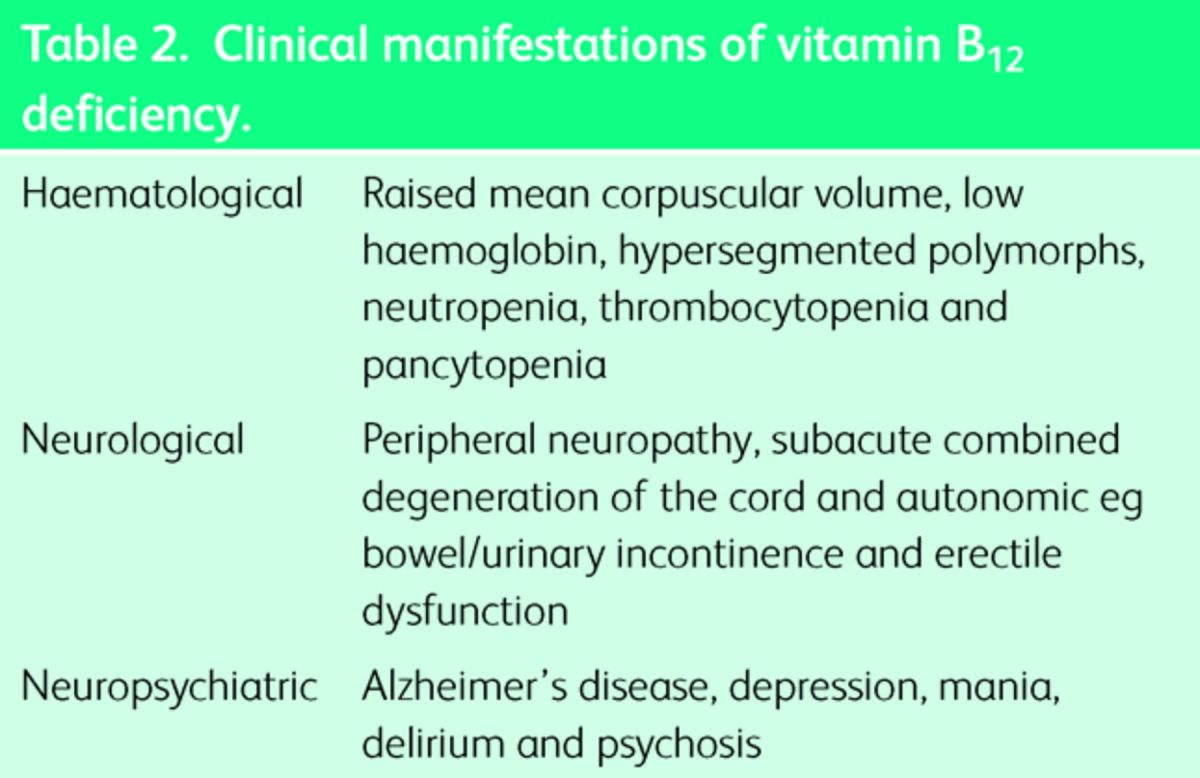
No particular correlation between haematological and neurological features has been demonstrated, such that those with neurological symptoms may have no haematological abnormalities, and vice-versa.15 Given that a diagnosis of vitamin B12 deficiency is most commonly made on discovery of macrocytic anaemia, rather than due to the neurological manifestations, it is possible that significant proportions of patients who are vitamin B12-deficient remain undiagnosed and risk developing irreversible neurological complications.
There is evidence to suggest that vitamin B12-insufficient patients may be at increased risk of osteoporosis.16
With pernicious anaemia there is a risk not only of gastric carcinoma, but also other autoimmune conditions, such as thyroid disease, type 1 diabetes mellitus and vitiligo.10
Although it is well established that hyperhomocysteinaemia is strongly associated with atherosclerosis, the relationship between low serum cobalamin levels and atheromatous disease remains a contentious issue. Despite the concomitant increase in serum homocysteine levels seen with vitamin B12 deficiency, there is evidence to suggest that a deficit of cobalamin does not increase the risk of cardiovascular disease.17
How is vitamin B12 deficiency diagnosed?
In the right clinical setting, identification of macrocytic anaemia and the blood film findings of hypersegmented (more than 5 lobes) neutrophils suggest vitamin B12 deficiency. But the definitive test is determination of serum cobalamin levels, which if <148 pmol/l, is highly sensitive for the diagnosis. Recently, the BCSH has produced guidelines to assist laboratory diagnosis.2 It is recommended that serum cobalamin and folate levels be assessed in tandem, due to the overlap in metabolic pathways.2 There are some caveats to be remembered.
Falsely low cobalamin levels may occur in folate deficiency,2 haptocorrin deficiency, multiple myeloma and oral contraceptive therapy.18
Serum MMA concentrations may be elevated in renal insufficiency which can make interpretation difficult.14
At present, no ‘gold standard’ test exists for the diagnosis of vitamin B12 deficiency and as a consequence, the diagnosis requires consideration of both the clinical state of the patient and the results of investigations.
Tests for pernicious anaemia
To afford the distinction between pernicious anaemia and other causes of low cobalamin levels, it is necessary to test for serum autoantibodies.5 The anti-IF antibody test is a relatively insensitive (50–70%) yet highly specific (>95%) investigation;5 in contrast, the anti-PC antibody test has a sensitivity of >90% but a specificity of only 50%.8 For this reason, the anti-IF antibody assay is the preferred test according to the BCSH, and assessment of anti-PC antibody titres is not recommended.2 Unfortunately, no test is currently available for FBCM; the Schilling test was used to exclude IF-mediated vitamin B12 malabsorption, but it is not currently clinically available.5
Newer tests
Most assays for assessing serum vitamin B12 levels measure cobalamin bound to both transcobalamin II and haptocorrin, that is, total serum cobalamin.19 Newer tests afford the measurement of holotranscobalamin II – the proportion of transcobalamin II conjugated to vitamin B12.6 This form of assay could potentially be performed following oral administration of cobalamin to assess intestinal uptake as a means to diagnose vitamin B12 malabsorption.
The conundrum of subclinical cobalamin deficiency
In addition to a symptomatic lack of vitamin B12, there exists a state in which, despite the biochemical anomalies, no clinical manifestations are present, termed ‘subclinical cobalamin deficiency’ (SCCD).20 SCCD is more common than symptomatic vitamin B12 deficiency. Rather than being associated with an IF-mediated inability to absorb vitamin B12, in 30–40% of cases SCCD occurs as a consequence of FBCM. At present, it is thought that SCCD is a transient phenomenon that does not progress to overt vitamin B12 deficiency. Even so, a search should be instituted to exclude treatable causes. Patients with a serum cobalamin within the range of 110–148 pmol/l should be re-checked in 1–2 months, and those with subsequently normal cobalamin levels do not require further investigation.2 However, patients with persistently suboptimal cobalamin levels should be tested for anti-IF antibody titres and given low-dose oral cobalamin as cover. These patients are recommended to return to the doctor if neurological symptoms develop. If anti-IF levels are positive then the patient should be managed as for pernicious anaemia; if negative, then cobalamin levels should be reassessed after 3–4 months and, if persistently low, further biochemical investigations are warranted to confirm biochemical deficiency.
How should vitamin B12 deficiency be treated?
At present, regardless of the underlying cause, patients in the UK are treated with intramuscular cobalamin according to the following recommendations.21
For those with no neurological involvement, the usual regimen is hydroxocobalamin 1 mg on alternate days for two weeks, followed by three-monthly injections of hydroxocobalamin 1 mg.
This regimen should be given for life if owing to pernicious anaemia.
If the deficiency is due to another cause, then treatment should continue until sustained improvement in haematological indices is seen.
In cases where there are neurological features, the same dose is given until no further symptomatic improvement is seen, followed by two-monthly injections.
Referral to secondary care is recommended if severe neurological symptoms are present, the patient is pregnant or if there is any uncertainty about the diagnosis.
Gastroenterology investigations are warranted if there is suspicion of malabsorption, gastric cancer or coeliac disease.
Often, management of underlying conditions, such as provision of antibiotics for bacterial overgrowth,5 and cessation of offending drugs can prove useful.
Can we give oral vitamin B12?
Despite the ‘dependence’ on intramuscular administration, there is accumulating evidence that oral cobalamin therapy may be as effective. As long as 60 years ago, identification of the alternative IF-independent mechanism for vitamin B12 absorption resulted in the discovery that if large enough doses were given, in the range of 100-100,000 μg (although only 1% of the cyanocobalamin was absorbed), it was sufficient to provide the daily requirement.22 More recently, Andrès et al demonstrated the efficacy of oral cobalamin in ameliorating both the biochemical and clinical manifestations of vitamin B12 deficiency in two separate trials.23,24 Durable improvement in serum cobalamin levels was seen following daily administration of oral cyanocobalamin 2,000 μg, which, at four-month follow-up, resulted in even greater serum levels than those generated in response to parenteral therapy.22 In addition, a similar proportion of subjects demonstrated improvement in neurological symptoms, such as bilateral paraesthesiae and ataxia, in both groups (22% in the oral arm vs 27% in the intramuscular arm). A similarly designed trial by Castelli et al produced comparable findings with the provision of 1,000 μg orally per day.25 The obvious advantages of oral therapy are patient convenience, reduction in healthcare costs for administering injections, as well as reduction in risk of bleeding in those who may be anticoagulated.26
The recent BCSH guidelines recommend that although not suitable for treating pernicious anaemia, oral cobalamin may be considered as an option for maintenance or correction of asymptomatic vitamin B12 deficiency.2 Further, the BCSH also suggest that low-dose (50 μg) oral cobalamin may be prescribed for FBCM.
Why the reluctance?
Only Sweden and Canada routinely prescribe oral vitamin B12.27 Possible reasons underlying the aversion of doctors to prescribe oral cobalamin include a lack of dissemination of evidence in favour of oral therapy, and issues regarding inefficient absorption, especially in co-morbid conditions such as coeliac disease.26 An additional concern is that all present trials have been conducted in a hospital environment where drug administration is monitored. In the primary care setting, where vitamin B12 deficiency occurs most frequently, it would not be as simple to assess the level of adherence to treatment. A large randomised, controlled multicentre trial is currently recruiting participants to test the efficacy of oral compared with intramuscular cobalamin in the primary care setting.27 The results of this study are eagerly awaited.
Are high serum vitamin B12 levels significant?
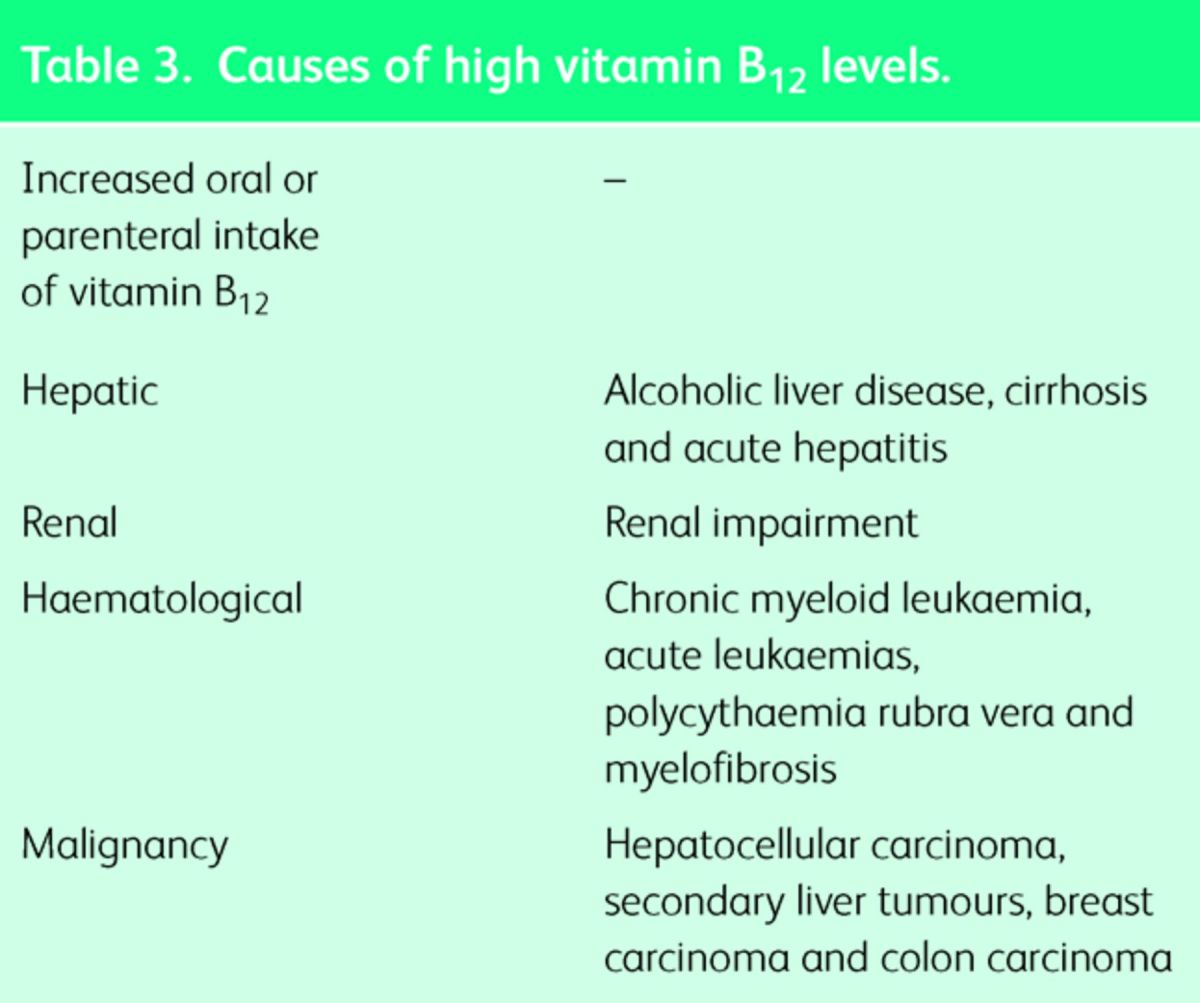
There is mounting evidence that raised serum vitamin B12 levels are a common finding (values varied from 350 to 1,200 pmol/l), with a prevalence of up to 14% in hospitalised patients referred for vitamin B12 measurement28 and even up to 50% of older inpatients.29 An elevation in serum vitamin B12 levels may arise from increased oral or parenteral intake, decreased uptake by the liver or kidney, greater release from cells (especially hepatocytes), or a rise in the synthesis of the transcobalamins by hepatocytes or granulocytes.28 Table 328 lists the causes of raised vitamin B12 levels. Although, elevated B12 levels are associated with liver disorders and haematological disorders, other malignancies may cause an elevated B12 as a reactive feature (like an acute phase protein). Further trials are required to elucidate whether development of cancer is definitively correlated with high vitamin B12 levels per se, or rather due to raised serum folate. A recent extended follow-up of two vitamin B intervention trials from Norway noted that additional treatment with folic acid (and not just B12) was associated with increased cancer incidence, cancer mortality and all-cause mortality.30 Over the past decade, there has been significant interest in the use of cobalamin as a marker of mortality, as studies have demonstrated an association between high vitamin B12 levels and mortality in hospitalised older patients,29 as well as in those admitted to intensive care.31 Once again, these are preliminary findings which need validation in good trials before widespread acceptance.
Table 3.
Causes of high vitamin B12 levels.
Paradoxically, investigation of patients with symptoms of vitamin B12 deficiency may actually reveal elevated levels of serum cobalamin, with a parallel rise in the markers MMA and homocysteine. Such functional cobalamin deficiency may arise when there is increased binding of vitamin B12 to haptocorrin as opposed to transcobalamin II, with subsequent reduction in delivery of the vitamin to peripheral cells.28 Unless accompanied by the clinical manifestations of vitamin B12 deficit, functional cobalamin deficiency is usually asymptomatic. In this situation, the BCSH recommend that homocysteine and MMA levels be assessed, with a trial of hydroxocobalamin therapy instituted.2
Conclusions
In the general population, vitamin B12 insufficiency is a relatively common finding, with an increased incidence with age. The majority of cases result in mild symptoms and are due to FBCM, while pernicious anaemia is much rarer nowadays but is associated with severe deficiency. One of the greatest issues in this area is knowing what ‘normal’ vitamin B12 levels should be and the consequential paucity of diagnostic criteria. Taking into consideration a thorough history and clinical manifestations is therefore paramount. A trial of cobalamin therapy can be very helpful in these cases. In the future, assays for markers such as holotranscobalamin should become available to determine more specifically the cause of the deficit, enabling treatment that is tailored to the patient. In addition, there will hopefully be a shift from injections to daily tablets, a move which should improve patient comfort.
Learning points
Food-bound cobalamin malabsorption is the commonest cause of low serum cobalamin levels, while pernicious anaemia accounts for the majority of cases of severe vitamin B12 deficiency.
Neurological symptoms can develop in patients without haematological manifestations like anaemia and macrocytosis.
Sequelae of untreated vitamin B12 deficiency includes not only permanent neurological symptoms, but also osteoporosis and cardiovascular disease.
In the UK, current management relies exclusively on intramuscular injection, but evidence suggests that oral therapy is as efficacious as parental treatment.
High serum cobalamin levels are associated with liver disease, malignancy and haematological dyscrasias, and may be positively correlated with risk of mortality.
References
- 1 .Dali-Youcef N, Andrès E. An update on vitamin B12 deficiency in adults. Q J Med 2009;102:17–28. [DOI] [PubMed] [Google Scholar]
- 2 .Devalia V, Hamilton MS, Molloy AM; The British Committee for Standards in Haematology. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Brit J Haematol 2014;166:496–513. [DOI] [PubMed] [Google Scholar]
- 3 .Allen LH. How common is vitamin B-12 deficiency? Am J Clin Nutr 2009;89:693S–696S. [DOI] [PubMed] [Google Scholar]
- 4 .Antony AC. Vegetarianism and vitamin B-12 (cobalamin) deficiency. Am J Clin Nutr 2003;78:3–6. [DOI] [PubMed] [Google Scholar]
- 5 .Carmel R. How I treat cobalamin (vitamin B12) deficiency. Blood 2008;112:2214–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6 .Nielsen MJ, Rasmussen MR, Andersen CB, Nexø E, Moestrup SK. Vitamin B12 transport from food to the body's cells - A sophisticated, multistep pathway. Nat Rev Gastroenterol Hepatol 2012;9:345–54. [DOI] [PubMed] [Google Scholar]
- 7 .Berg J, Tymoczko J, Stryer L. Biochemistry, 5th edn New York: WH Freeman, 2003. [Google Scholar]
- 8 .Andrès E, Loukili NH, Noel E, et al. Vitamin B12 (cobalamin) deficiency in elderly patients. Can Med Assoc J 2004;171:251–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9 .Toh BH, van Driel IR, Gleeson PA. Pernicious anaemia. N Eng J Med 1997;337:1441–8. [DOI] [PubMed] [Google Scholar]
- 10 .Stabler SP. Vitamin B12 deficiency. N Eng J Med 2013;368:149–60. [DOI] [PubMed] [Google Scholar]
- 11 .Lam JR, Schneider JL, Zhao W, Corley DA. Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. J Am Med Assoc 2013;310:2435–42. [DOI] [PubMed] [Google Scholar]
- 12 .de Jager J, Kooy A, Lehert P, et al. Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: Randomised placebo controlled trial. Brit Med J 2010;340:c2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13 .Liu Q, Li S, Quan H, Li J. Vitamin B12 status in metformin treated patients: Systematic review. PLoS One. 2014;9:e100379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14 .Lachner C, Steinle NI, Regenold WT. The neuropsychiatry of vitamin B12 deficiency in elderly patients. J Neuropsychiatry Clin Neurosci 2012;24:5–15. [DOI] [PubMed] [Google Scholar]
- 15 .McCadden A. Vitamin B12 in neurology and ageing: Clinical and genetic aspects. Biochimie 2013;95:1066–76. [DOI] [PubMed] [Google Scholar]
- 16 .Tucker KL, Hannan MT, Qiao N, et al. Low plasma vitamin B12 is associated with lower BMD: The Framingham Osteoporosis study. J Bone Miner Res 2005;20:152–8. [DOI] [PubMed] [Google Scholar]
- 17 .van Oijen MGH, Vlemmix F, Laheij RJF, Paloheimo L, Jansen JBM, Verheugt FWA. Hyperhomocysteinaemia and vitamin B12 deficiency: The long-term effects in cardiovascular disease. Cardiology 2007;107:57–62. [DOI] [PubMed] [Google Scholar]
- 18 .Chatthanawaree W. Biomarkers of cobalamin (vitamin B12) deficiency and its application. J Nutr Health Aging 2011;15:227–31. [DOI] [PubMed] [Google Scholar]
- 19 .Arendt JF, Nexø E. Unexpected high plasma cobalamin — Proposal for diagnostic strategy. Clin Chem Lab Med 2013;51:489–96. [DOI] [PubMed] [Google Scholar]
- 20 .Carmel R. Subclinical cobalamin deficiency. Curr Opin Gastroenterol 2012;28:151–8. [DOI] [PubMed] [Google Scholar]
- 21 .NICE Anaemia – Vitamin B12 and folate deficiency. NICE Clinical Knowledge Summaries, November 2014. Available online at http://cks.nice.org.uk/anaemia-b12-and-folate-deficiency [Accessed 4 December 2014]. [Google Scholar]
- 22 .Kuzminski AM, Del Giacco EJ, Allen RH, Stabler SP, Lindenbaum J. Effective treatment of cobalamin deficiency with oral cobalamin. Blood 1998;92:1191–8. [PubMed] [Google Scholar]
- 23 .Andrès E, Kurtz J, Perrin A, et al. Oral cobalamin therapy for the treatment of patients with food-cobalamin malabsorption. Am J Med 2001;111:126–9. [DOI] [PubMed] [Google Scholar]
- 24 .Andrès E, Loukili NH, Noel E, et al. Effects of oral crystalline cobalamin 1000 μg/d in the treatment of pernicious anemia: An open-label, prospective study in ten patients. Curr Ther Res 2005;66:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25 .Castelli MC, Friedman K, Sherry J, et al. Comparing the efficacy and tolerability of a new daily oral vitamin B12 formulation and intermittent intramuscular vitamin B12 in normalizing low cobalamin levels: A randomized, open-label, parallel-group study. Clin Ther 2011;33:358–71. [DOI] [PubMed] [Google Scholar]
- 26 .Butler CC, Vidal-Alaball J, Cannings-John R, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: A systematic review of randomized controlled trials. Fam Pract 2006;23:279–85. [DOI] [PubMed] [Google Scholar]
- 27 .Sanz-Cuesta T, González-Escobar P, Riesgo-Fuertes R, et al. Oral versus intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency: A pragmatic, randomised, multicentre, non-inferiority clinical trial undertaken in the primary healthcare setting (Project OB12). BMC Public Health 2012;12:394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28 .Andrès E, Serraj K, Zhu J, Vermorken AJM. The pathophysiology of elevated vitamin B12 in clinical practice. Q J Med 2013;106:505–15. [DOI] [PubMed] [Google Scholar]
- 29 .Tal S, Shavit Y, Stern F, Malnick S. Association between vitamin B12 levels and mortality in hospitalized older adults. J Am Geriatr Soc 2010;58:523–6. [DOI] [PubMed] [Google Scholar]
- 30 .Ebbing M, Bønaa KH, Nygård O, et al. Cancer incidence and mortality after treatment with folate and vitamin B12. J Am Med Assoc 2009;302:2119–26. [DOI] [PubMed] [Google Scholar]
- 31 .Sviri S, Khalaila R, Daher S, et al. Increased vitamin B12 levels are associated with mortality in critically ill medical patients. Clin Nutr 2012;31:53–9. [DOI] [PubMed] [Google Scholar]