ABSTRACT
Recent studies have shown that the claim that King George III suffered from acute porphyria is seriously at fault. This article explores some of the causes of this misdiagnosis and the consequences of the misleading claims, also reporting on the nature of the king's recurrent mental illness according to computer diagnostics. In addition, techniques of cognitive archaeology are used to investigate the nature of the king's final decade of mental illness, which resulted in the appointment of the Prince of Wales as Prince Regent. The results of this analysis confirm that the king suffered from bipolar disorder type I, with a final decade of dementia, due, in part, to the neurotoxicity of his recurrent episodes of acute mania.
KEYWORDS : Acute intermittent porphyria, bipolar disorder, computer diagnostics, King George III, senile dementia, variegate porphyria
A professional is a man who can do his job when he doesn't feel like it.
An amateur is a man who can't do his job when he does feel like it.
HS Torrens (2006)1
Introduction
The lengthy reign of King George III (1760–1820) coincided with a succession of important military and political events, including the loss of the American colonies, the defeat of Napoleon, the development of the Industrial Revolution and the founding of the British Empire. Historians have discussed, at length, the role of George III in the decisions leading to these and other events. The nature of his recurrent ill health is clearly relevant, but, surprisingly, has been little explored by professional historians, who have been content to follow the views of the porphyria claimants despite their limited training in historical methods and modern medical diagnostic techniques.
Background
The amateur historians Ida Macalpine and Richard Hunter initially claimed a diagnosis of acute intermittent porphyria as the cause of King George III's recurrent mental illness, which they later changed to the rarer and milder variegate porphyria.2,3 My colleagues and I have shown these diagnoses to be unsustainable in studies that were reported in this journal in 2011 and elsewhere4–7 and that were recently highlighted in an article relating to George III by John Cannon in the Oxford dictionary of national biography.8 In spite of these reports, recent publications have cited claims of porphyria as the definitive cause of the king's illness. The recent exhibition on Georgian London at the British Library and the associated guide book9 both highlight porphyria as the cause of the king's illness, and recent correspondence with the relevant library curator confirms the British Library's unwavering adherence to the porphyric claims, although the contradictory evidence is on their own shelves! Similarly, a recent visit to Kew Gardens – the grounds of Kew Palace, which was the focus for the king's illness in 1788–9 – identified the diagnosis of porphyria in the palace itself, the guide book10 and the welcoming greetings of the guides.
Reasons for the persistent adherence to the claims of porphyria are unclear. Following Macalpine and Hunter's publications in the British Medical Journal in 1966 and 1968,2,3 their claims were challenged by authorities on porphyrin from the UK and abroad on the basis of clinical, laboratory and genetic evidence.11 However, Macalpine and Hunter garnished support from distinguished physicians, fellows of the Royal Society and even the Nobel laureate Hans Krebs. Non-medical historians past and present, including Alan Bennett, Jeremy Black, John Brooke, Antonia Fraser and Roy Porter, have enthusiastically adopted Macalpine and Hunter's diagnosis, clearly without detailed reading of the more than 100 volumes of medical notes concerning George's illnesses. In contrast, medical historians with an interest in psychiatry – including Arnold Chaplin, the FitzPatrick Lecturer of 1917–18 – have all, since the first study in 1831, clearly shown a diagnosis of bipolar disorder (or the contemporary synonym).12 In contrast, the only mental disorder sometimes associated with acute porphyria, even in complete remission, is anxiety.13
In order to provide an objective diagnosis of the king's mental disorder, current techniques of cognitive archaeology14 – including computer diagnostics15 and handwriting analysis16 – are currently being applied to the primary source data.
Methods and results
Primary medical sources alone are the basis for our study, as secondary sources may be misleading and are best avoided in research of medical history. In addition, internationally accepted diagnostic criteria (International and statistical classification of diseases and health-related problems, tenth edition (ICD-10) and Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR)) are used where possible.17,18 Recently, computer-based diagnostic programs have become available, which should minimise any observer bias.
The computer diagnostic program Operational Criteria Checklist for Psychotic Illness (OPCRIT) was developed for case-note analysis of patients with psychotic illness participating in genetic studies and has been extended and validated in response to subsequent editions of the DSM criteria. Analysis with OPCRIT has confirmed the diagnosis of George III's mental illness as recurrent episodes of acute mania – bipolar disorder type I.19 Table 1 shows the diagnostic conclusions for his episodes of acute mania based on different criteria using the OPCRIT method. No diagnosis is available for the episode in 1804, as insufficient clinical data are available in the medical records. The Willis papers do not record any clinical details of the king's illness, as the Willis brothers, physicians to George III, were excluded on the insistence of Prime Minister Henry Addington. The king was therefore under the care of Dr Samuel Foart Simons, physician to St Luke's asylum (1781–1811), but his medical notes apparently have not been preserved. This illustrates the value of using objective diagnostic methods in historical diagnosis.
Table 1.
OPCRIT analysis of King George III's mental health disorders in 1788–9, 1801 and 1810–11.
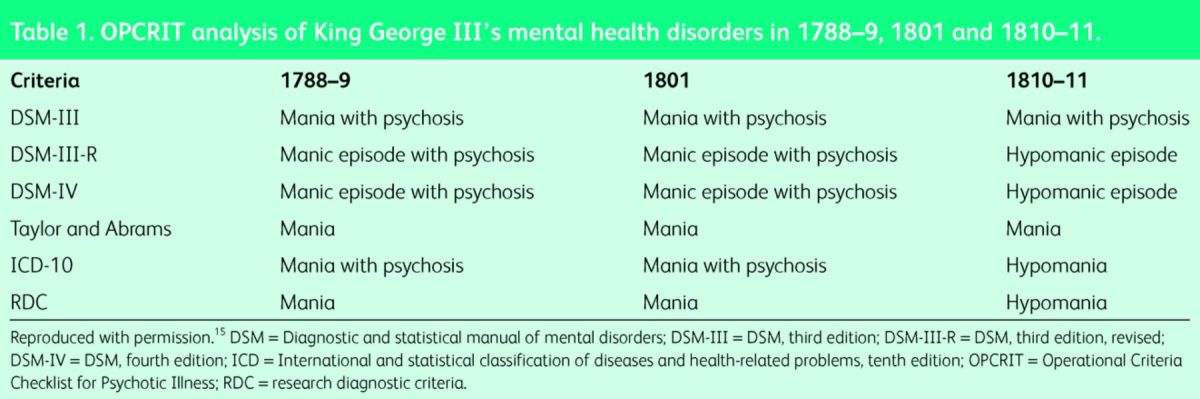
The severity of George's mania during the 1810–11 episode was probably milder than during other episodes, as reflected by a diagnosis of hypomania rather than mania for three of the five diagnostic criteria. This probably reflects the onset of dementia discussed later in this paper. The severity of the mania can also be assessed objectively when detailed clinical information exists: for example, using the methods of Young et al,20 a peak value of 40/60 is obtained for 23–28 December 1788, which corresponds to the most severe form of mania (Grade IV).
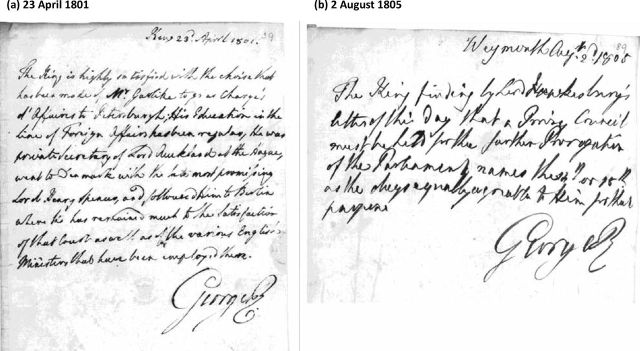
Handwriting deteriorates with age; signatures less so.21 In particular, analysis of the spatial and lexical aspects of handwriting have been shown to correlate with a subject's score on the mini-mental state examination (MMSE).16 This analytical method is used for medico–legal studies but, to date, has not been applied to distant historical figures. In a parallel study, therefore, computational linguistic analysis of changes in George III's handwriting and signatures in his letters22 is being carried out, with preliminary results presented here. More than 500 of George III's letters, ranging from his earliest on 23 June 1749 (aged 11 years) up to 1 August 1809 (aged 70 years), have been collected and analysed. Fig 1 shows examples of letters before deterioration of the king's handwriting (1801) and after (1805); note the lexical and spatial deterioration of the 1805 letter and the increased size of the individual words in this later letter, which is a feature of impaired vision.16,21
Fig 1.
George III's letters. (a) 23 April 1801 (MMSE score 21) and (b) 2 August 1805 (MMSE score 13). Reproduced with permission.23 MMSE = mini-mental state examination.
Table 2 shows preliminary scores for representative letters. Up to the age of 50 years, George III had an essentially normal MMSE score. A transient decrease occurred during his major manic episode between August 1788 and May 1789, following which the scores basically return to premorbid levels. However, from about 1803, particularly from January 1805, there is progressive deterioration in the lexical and spatial scores. Unfortunately, George was blind from December 1805 and employed an amanuensis (Colonel Herbert Taylor), so only a single holograph letter from this later period has been located. The significant decrease in MMSE scores from 1804 and deterioration of signatures from 1808 (Fig 2) is consistent with the onset of dementia, which led to the appointment of the Prince Regent in 1811 and plagued King George up to his death in 1920. Current studies are extending these findings.
Table 2.
Fontana analysis and MMSE of a range of George III's letters between 22 September 1761 and 1 August 1809.16
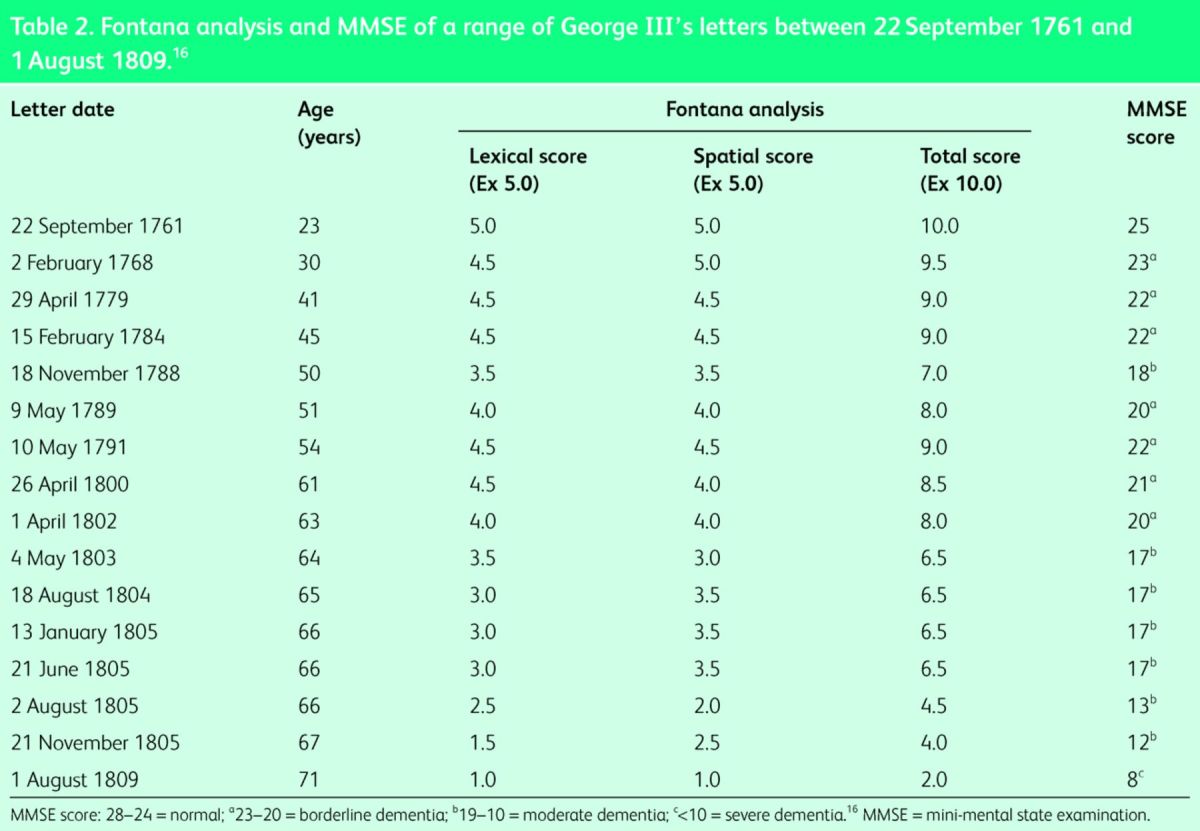
Fig 2.
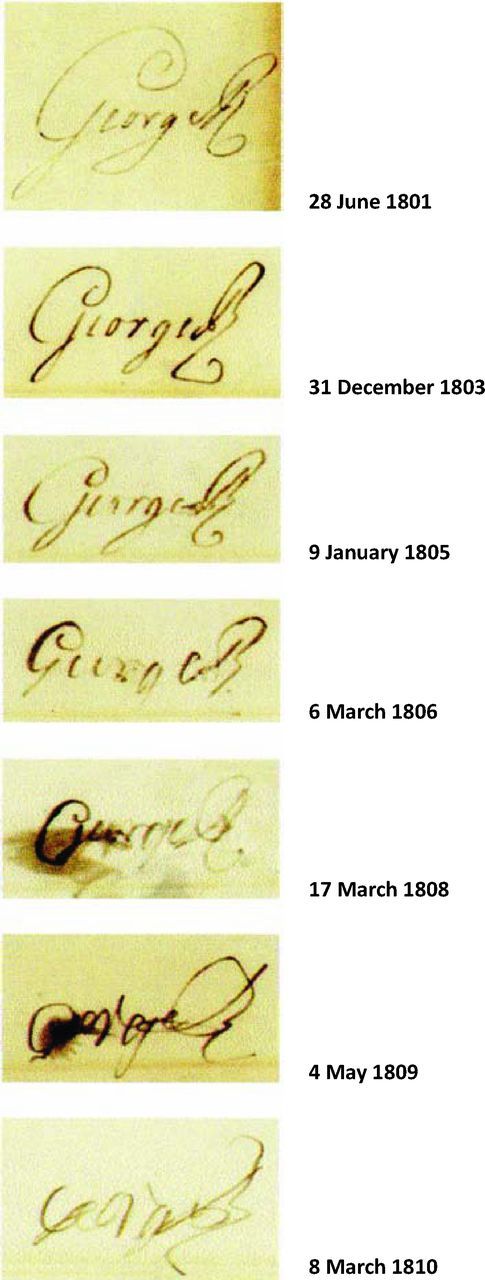
Signatures of George III taken from his annual letters to his bankers, Messrs Drummonds (28 June 1801– 8 March 1810). Reproduced with permission.24
Consequences of the claim of porphyria
As indicated earlier, widespread dissemination in 1966 of the claims of porphyria as the basis of George III's mental illness has had a plethora of literary, medical and other implications. The canonical parody ‘Eight songs for a mad king’ by Peter Maxwell Davis (1969) and Alan Bennett's play and film ‘The madness of George III’ (1991 and 1995, respectively) raised public interest in porphyria as a cause of the king's mental illness. These works, along with enthusiastic editorials in the British Medical Journal and elsewhere, further stimulated subsequent claims by Macalpine and Hunter25 and other speculators of mental illnesses that historical persons – ranging from William the Conqueror to the late Prince William of Gloucester and Princess Margaret26 – suffered from underlying porphyrias. Similarly, historical novels have posited that Charles Darwin,27 Vincent van Gogh and his siblings,28 among others, were also affected by porphyrias.
More seriously, considerable effort has consequently been spent screening many thousands of patients with mental illness for porphyria. Saphier and Shaw29 reported that some 15,000 patients in south-west London were screened for porphyria without a single case being identified. Surely the money involved could have been better used to improve patient care?
In view of the potentially questionable nature of Macalpine and Hunter's papers on the mental illnesses of George III and his ancestors and descendants, with their professional and personal claims underlying the nature and treatment of mental illnesses, should other publications by them be reconsidered?5
From the view of the professional historian, labelling of George III as porphyric has inadvertently diverted researchers from a study of the nature and causes of the various issues – both successful and unsuccessful – during his reign. With increasing evidence that patients with bipolar disorder in remission (euthymia) may exhibit behavioural and psychological changes, including low self-esteem, obsessive–compulsive features, neurocognitive impairment, excessive rumination and borderline personality disorders, these could have affected the political actions and judgement of George III and his descendants.30–35
Source
The FitzPatrick Lecture on the history of medicine is delivered annually at the Royal College of Physicians of London by a fellow of the RCP. This article is based on the 2014 lecture delivered on 14 April 2014 by Professor Timothy Peters, honorary senior research fellow at the University of Birmingham's Institute of Archaeology and Antiquity.
Acknowledgements
I thank Her Majesty the Queen for gracious permission to examine medical records in the Royal Archives and Miss Pamela Clark, registrar, for her assistance and advice. The continuing invaluable collaboration with Dr Peter Garrard and colleagues at St George's University, London, is gratefully acknowledged. The research of Peter Basham (Royal College of Physicians of London) and Harriet Wheelock (Royal College of Physicians of Ireland) have proved invaluable. The assistance and advice of the staff of the British Library, the National Archives, Royal Bank of Scotland and Wellcome Trust are gratefully acknowledged.
References
- 1 .Torrens HS. Notes on ‘The amateur’ in the development of British geology. Proc Geol Assoc 2006;117:1–8. [Google Scholar]
- 2 .Macalpine I, Hunter R. The ‘insanity’ of King George 3d: a classic case of porphyria. Br Med J 1966;1:65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3 .Macalpine I, Hunter R, Rimington C. Porphyria in the royal houses of Stuart, Hanover, and Prussia. A follow-up study of George 3d's illness. Br Med J 1968;1:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4 .Peters TJ. King George III, bipolar disorder, porphyria and lessons for historians. Clin Med 2011;11:261–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5 .Peters TJ, Wilkinson D. King George III and porphyria: a clinical re-examination of the historical evidence. Hist Psychiatry 2010;21:3–19. [DOI] [PubMed] [Google Scholar]
- 6 .Peters TJ, Beveridge A. The madness of King George III: a psychiatric re-assessment. Hist Psychiatry 2010;21:20–37. [DOI] [PubMed] [Google Scholar]
- 7 .Hift RJ, Peters TJ, Meissner PN. A review of the clinical presentation, natural history and inheritance of variegate porphyria: its implausibility as the source of the ‘royal malady’. J Clin Pathol 2012;65:2000–5. [DOI] [PubMed] [Google Scholar]
- 8 .Cannon J. George III (1738–1820). In: Oxford dictionary of national biography. Oxford: Oxford University Press, 2013. [Google Scholar]
- 9 .Goff M, Goldfinch J, Limper-Hertz K, Peden H. Georgians revealed. London: British Library, 2013. [Google Scholar]
- 10 .Historic Royal Palaces Discover Kew Palace. Hampton Court: Historic Royal Palaces, 2006. [Google Scholar]
- 11 .Dent CE. Royal malady. Br Med J 1968:1:311–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12 .Peters TJ, Willis C. Mad monarchs: comparison of the nature, causes and consequences of the mental ill health of Maria I of Portugal and George III of Great Britain. Court Historian 2014;19:29–42. [Google Scholar]
- 13 .Millward LM, Kelly P, King A, Peters TJ. Anxiety and depression in the acute porphyrias. J Inherit Metab Dis 2009;28:1099–107. [DOI] [PubMed] [Google Scholar]
- 14 .Gerrard P. Cognitive archaeology: uses, methods, and results. J Neurolinguistics 2009;22:250–65. [Google Scholar]
- 15 .Peters TJ, Garrard P. Computer-based diagnosis of illness in historical persons. J R Coll Phys Edin 2013;43:161–8. [DOI] [PubMed] [Google Scholar]
- 16 .Fontana P, Dagnino F, Cocito L, Balestrino M. Handwriting as a gauge of cognitive status: a novel forensic tool for posthumous evaluation of testamentary capacity. Neurol Sci 2008;29:257–61. [DOI] [PubMed] [Google Scholar]
- 17 .World Health Organization International statistical classification of diseases and related health problems, tenth edition Edinburgh: Churchill Livingstone, 1995. [Google Scholar]
- 18 .American Psychiatric Association Diagnostic and statistical manual of mental disorders, fourth edition, text revision Arlington, TX: APA, 2000. [Google Scholar]
- 19 .McGuffin P, Farmer A, Harvey IA. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Arch Gen Psychiat 1991;48:764–70. [DOI] [PubMed] [Google Scholar]
- 20 .Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 1978;133:429–35. [DOI] [PubMed] [Google Scholar]
- 21 .Walton J. Handwriting changes due to aging and Parkinson's syndrome. Forensic Sci Int 1997;88:197–214. [DOI] [PubMed] [Google Scholar]
- 22 .Rentoumi V, Peters T, Conlin J, et al. The acute mania of King George III: a computational linguistic analysis. Proc Nat Acad Sci USA (submitted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23 .British Library Liverpool papers. MS 38,564, ff. 1–90. [Google Scholar]
- 24 .Royal Bank of Scotland Archives Drummond letters [DR/567/1-7]. [Google Scholar]
- 25 .Macalpine I, Hunter R. George III and the mad-business. London: Allen Lane, 1969. [Google Scholar]
- 26 .Rushton AR. Royal maladies: inherited diseases in the ruling houses of Europe. Victoria: Trafford Publishing, 2008. [Google Scholar]
- 27 .Colp C. To be an invalid: the illness of Charles Darwin. Chicago, IL: University of Chicago Press, 1977. [Google Scholar]
- 28 .Arnold WN. Vincent van Gogh: chemicals, crises, and creativity. Boston, MA: Birkhauser, 1992. [Google Scholar]
- 29 .Saphier E, Shaw D. Insanity of King George III. Br Med J 1966;1:232. [Google Scholar]
- 30 .Winters KC, Neale JM. Mania and low self-esteem. J Abnorm Psychol 1984;94:282–90. [DOI] [PubMed] [Google Scholar]
- 31 .Deep CA, Savla GN, Moore DJ, et al. Short-term course of neuropsychological abilities in middle-aged and older adults with bipolar disorder. Bipolar Disord 2008;10:684–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32 .Van der Gucht, Morriss R, Lancaster G, et al. Psychological processes in bipolar affective disorder: negative cognitive style and reward processing. Br J Psychiatry 2009;194:146–51. [DOI] [PubMed] [Google Scholar]
- 33 .Nilsson KK, Jorgensen CR, Craig TKL, et al. Self-esteem in remitted bipolar disorder patients: a meta-analysis. Bipolar Disord 2010;12:585–92. [DOI] [PubMed] [Google Scholar]
- 34 .Jones SH, Tai S, Evershed K, et al. Early detection of bipolar disorder: a pilot familial high-risk study of parents with bipolar disorder and their adolescent children. Bipolar Disord 2003;8:362–72. [DOI] [PubMed] [Google Scholar]
- 35 .Maziade M, Rouleau N, Mérette C, et al. Verbal and visual memory impairment among young offspring and healthy adult relatives of patients with schizophrenia and bipolar disorder: selective generational patterns indicate different development trajectories. Schizophr Bull 2011;37:1218–28. [DOI] [PMC free article] [PubMed] [Google Scholar]